Abstract
Purpose
Odontoid fractures are the most common cervical spine fractures in the elderly, with a controversial optimal treatment. The objective of this review was to compare the outcome of surgical and conservative treatments in elderly (≥ 65 years), by updating a systematic review published by the authors in 2013.
Methods
A comprehensive search was conducted in seven databases. Clinical outcome was the primary outcome. Fracture union- and stability were secondary outcomes. Pooled point estimates and their respective 95% confidence intervals (CIs) were derived using the random-effects model. A random-effects multivariable meta-regression model was used to correct for baseline co-variates when sufficiently reported.
Results
Forty-one studies met the inclusion criteria, of which forty were case series and one a cohort study. No clinical differences in outcomes including the Neck Disability Index (NDI, 700 patients), Visual Analogue Scale pain (VAS, 180 patients), and Smiley-Webster Scale (SWS, 231 patients) scores were identified between surgical and conservative treatments. However, fracture union was higher in surgically treated patients (pooled incidence 72.7%, 95% CI 66.1%, 78.5%, 31 studies, 988 patients) than in conservatively treated patients (40.2%, 95% CI 32.0%, 49.0%, 22 studies, 912 patients). This difference remained after correcting for age and fracture type. Fracture stability (41 studies, 1917 patients), although numerically favoring surgery, did not appear to differ between treatment groups.
Conclusion
While surgically treated patients showed higher union rates than conservatively treated patients, no clinically relevant differences were observed in NDI, VAS pain, and SWS scores and stability rates. These results need to be further confirmed in well-designed comparative studies with proper adjustment for confounding, such as age, fracture characteristics, and osteoporosis degree.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Odontoid fractures account for 9 to 18% of all cervical spine fractures and are most frequently caused by either hyperextension or hyperflexion [1,2,3,4]. In the elderly, odontoid fractures are the most common cervical spine fractures [5, 6]. Moreover, as the population ages, these fractures will become increasingly relevant to clinical practice [4]. The optimal treatment of odontoid fractures in the elderly is, however, still subject to controversy. This age group typically suffers from an increased risk of operative complications when treated surgically but is also at a higher risk of non-union and prolonged treatment duration when treated conservatively.
The treatment for odontoid fractures is typically based on fracture pattern (such as defined by Anderson and d’Alonzo), patient age, neurological deficits and the patient’s medical condition, in an effort to weigh fracture healing versus treatment complications [2, 4, 7]. The general presumption is that a surgical intervention, i.e., either anterior odontoid screw fixation or posterior atlantoaxial fusion, leads to a stable cervical spine. However, the condition of the patient may deteriorate by undergoing (major) cervical spine surgery. Surgical intervention carries significant risks particularly in a very old patient (≥ 80 years). An alternative to surgical stabilization is conservative treatment, involving rigid or non-rigid immobilization. This treatment, however, can also fail and prolong fracture instability, requiring secondary surgery, which unnecessarily lengthens treatment duration. Additionally, conservative treatment can cause immobilization-related complications, e.g., pneumonia, pressure sores.
The objective of this review was to summarize and compare the outcomes of surgical and conservative treatments for type II and III odontoid fractures in the elderly (≥ 65 years), focusing primarily on clinical outcomes and secondarily on fracture union and stability rates. This review is an update of a systematic review published by the authors in 2013 [8].
Methods
Search methods for identification of studies
The PRISMA checklist was used for this review. A systematic search was conducted in seven databases of medical literature: MEDLINE, Embase, Cochrane Central Register of Controlled Trials, Web of Science, Emcare, Academic Search Premier, and PEDro to update the author’s previously published systematic review in 2013 (Supplementary Material). The updated search spanned between April 2012 and January 2022. No restriction was made with regard to language or date. ‘Os odontoideum’ was included in the search, as this term is sometimes incorrectly used to describe odontoid fractures. Duplicate references were removed. References from the included studies were also screened in order to identify additional primary studies not previously identified. Two review authors (JH, CV) working independently examined titles and abstracts from the electronic search. Full texts were obtained for titles and abstracts that were approved by pairs of reviewers. A third review author was consulted, if consensus was not reached.
Criteria for considering studies for this review
Studies were included if the following criteria were met: 1—Studies described one or more outcomes of at least ten patients treated for acute type II or III odontoid fractures, with or without associated fractures or dislocation. 2—Participants were at least 65 years old, and their data could be extracted separately from studies that also involved younger subjects. 3—Inclusion criteria were explicit, and the follow-up period was at least two weeks. 4—The study evaluated any surgical and/or conservative treatment and results were given for each distinct treatment. 5—Patients were not treated for odontoid fractures in the past. 6—Patients did not suffer from systemic comorbidity expected to influence outcome (e.g., rheumatoid arthritis). 7—The paper was published in a peer-reviewed journal. Case reports were excluded.
Clinical outcome was the primary outcome. The Neck Disability Index (NDI) was the most commonly used instrument to assess clinical outcome. The NDI is a 50-point scale, in which a higher score represents a higher degree of disability. The minimal clinically important change/difference (MCID) for the NDI was determined to be 7.5 [9,10,11,12]. The Visual Analogue Scale (VAS) pain score was also commonly reported. The VAS is a 10-point scale (derived from a 100 mm scale), in which a higher score represents a higher degree of pain, and of which the MCID was determined to be 1 (10 mm) [13, 14]. The Smiley-Webster Scale (SWS) was the third commonly used instrument. The SWS is an ordinal scale from 1 to 4, in which 1 represents excellent functioning and 4 represents poor functioning. Fracture union- and stability rates were the secondary outcomes. Fracture union was defined as the presence of bony consolidation of the fracture. Fracture stability was defined as the presence of either bony consolidation or fibrous union of the fracture.
Data collection and analysis
Two review authors (KB, CR) working independently conducted the data extraction. From each study, both demographic/descriptive data (e.g., study population, sample size, number of patients followed-up, fracture types, age, gender, applied treatment) and quantitative data regarding outcomes and complications were extracted. Outcomes were extracted at 52 weeks when available, and, if missing, outcomes at the last follow-up moment were extracted. Outcomes reported over wide and equally spaced intervals, such as NDI and VAS pain scores, were treated as continuous variables, and means and standard deviations were extracted and meta-analyzed. Unless otherwise specified, a random-effects model was used to calculate pooled point estimates with 95% confidence intervals for the NDI, fracture union, and fracture stability. A fixed-effect model was used for VAS scores to avoid negative values for the lower bound of the 95% CI. Outcomes reported over narrow or unequally spaced intervals, such as the SWS score, were treated as categorical ordinal variables, of which medians and their respective ranges were extracted. Given that medians cannot be meta-analyzed, weighted medians were calculated by multiplying the sample size in each study by its respective median, divided by the total number of patients in all studies, of which the result was rounded off. This was similar to the fixed-effect model using sample size as the weighting method. Forest plots were generated to summarize the results. P-values for heterogeneity (< 0.10) and I-squared were computed. I-squared values for heterogeneity were categorized as low (0–25%), moderate (25–50%) and substantial (> 50%). A random-effects multivariable meta-regression model was used to correct for baseline co-variates when sufficiently reported. Both baseline co-variates and clinical outcomes were heterogeneously and sparsely reported. Correction in the meta-regression analysis was therefore only feasible for mean age and fracture type (II, II/III) in relation to the radiological outcomes. The heterogeneous reporting of clinical outcomes made further analyses of these outcomes infeasible. Three meta-regression analyses were done for fracture union and fracture stability. The first model included treatment type, age and fracture type. The other models were for each treatment type separately: one for surgical and one for conservative treatment, including only age and fracture type to the model. A two-tailed p-value < 0.05 was considered statistically significant, unless otherwise indicated. Analyses were performed using Comprehensive Meta-Analysis Software (CMA), version 4.
Assessment of risk-of-bias for the included studies
Two review authors (KB, CR) working independently conducted the risk-of-bias assessment. Studies were classified as cohort studies if confounding variables were corrected for; otherwise, studies were treated as two separate case series extracted from one original study even if these studies were labelled as cohort studies by the authors. Risk-of-bias of the individual studies was assessed with methodology scores based on the type of study: Newcastle–Ottawa Quality Assessment Scale (NOS) for cohort studies and a self-designed appraisal form for uncontrolled case series based on three other studies [15,16,17,18, Supplementary Material]. For the NOS, cohort selection, comparability and outcome assessment were scored on a 0 to 9 range. Items were scored as positive if they fulfilled the criterion, negative when bias was likely or marked as inconclusive if there was insufficient information. If an item was scored positive, one point was awarded. The number of positively scored items was summed per study, adding up to a score between 0 and 22 points for this instrument. Differences in the scoring of the risk-of-bias assessment were discussed during a consensus meeting. For outcomes reported in at least ten studies, the potential for small study bias was assessed using funnel plots, along with Begg’s test for categorical outcomes and Egger’s test for continuous outcomes [19, 20]. Because of high heterogeneity in the results, the trim-and-fill method was not used to address the potential publication bias if an asymmetry was found in the funnel plot [19]. Instead, the classic fail safe n, which is the number of missing studies that would bring the p-value to > alpha, was conducted and reported for each outcome.
Results
Search and selection results
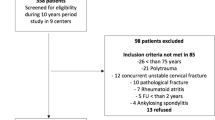
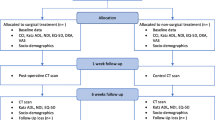
The initial search yielded 1,337 unique references, after removal of duplicates also identified in the search for the previous review [8]. After screening studies based on title and abstract, 127 studies were selected for full-text screening. Additionally, reference and citation tracking were carried out, yielding no further references. A total of thirty-one studies were initially identified. The seventeen unique studies from the previous review were also included, adding up to a total of forty-eight. Seven studies were subsequently excluded, all because they were believed to (partially) describe the same patient cohorts as other studies included in this review [20,21,22,23,24,25,26]. These studies were excluded in favor of studies (partially) reporting on the same patients, but that reported on larger samples and/or more appropriate clinical/radiological outcomes. A total of 41 studies were eventually included (Fig. 1 and Table 1). Four studies were carried out prospectively. Thirty-nine studies were published in English, one in French and one in German. Twenty-four studies systematically reported clinical outcome and hence, were primarily included, as this review’s primary focus was on clinical outcome. The other seventeen systematically reported union- and/or stability rates only and were consequently secondarily included. Overall, forty studies reported fracture union, and all forty-one reported fracture stability.
Risk-of-bias assessment
Only one study corrected for confounding variables and was hence classified as cohort study, while the remaining studies were classified as case-series (Supplementary Material). All but four studies were retrospective case series. Quality scores for case series ranged between 10 and 20 on a 22-point scale. For the case series, baseline demographics and results were mostly adequately reported, whereas baseline clinical status was generally poorly and heterogeneously reported. Funnel plots were only feasible for the outcomes of fracture union and fracture stability, as clinical outcomes were reported in fewer than ten studies (Supplementary Material). Begg’s test showed a significant small study effect for the surgically treated group for both fracture union and fracture stability (p = 0.048 and p = 0.049, respectively). Of note, the source of asymmetry in a funnel plot could be due to other reasons than publication bias (e.g., true heterogeneity, data irregularities, selection bias) [20]. Given the source of asymmetry was driven by publication bias, the classic fail safe n showed a very large number of missing studies that would be needed to bring the pooled results to become non-significant. This reinforced that the results were robust to any potential publication bias.
Baseline characteristics
A total of 2099 patients were included, of which 1104 (53%) were treated surgically. A total of 1917 patients were followed-up clinically and/or radiologically, representing a 91% follow-up rate. The pooled mean age was 80.6 (95% CI 79.0, 82.1) for surgically treated patients and 81.7 (95% CI 79.7, 83.7) for conservatively treated patients. A total of 1742 (83%) patients were treated for type II fractures, while the remaining 357 patients were enrolled in studies describing both type II and III fractures, in which outcomes were not typically split out by fracture type. The pooled mean follow-up time was 47.9 (95% CI 39.3, 56.4) weeks for surgically treated patients and 55.9 (95% CI 45.3, 66.5) weeks for conservatively treated patients. ASA scores were most frequently used to report baseline functioning, yet were still only provided in fourteen studies. Mean fracture displacement could be derived from only nine studies. Analysis of a difference in baseline functioning and fracture displacement between treatment groups was not feasible.
Clinical outcomes
Analysis of clinical outcome was only feasible for the three most commonly used instruments (Tables 2, 3 and Fig. 2). The remaining studies used other tools that were reported too sparsely to be compared.
Forest plots showing the pooled average reported outcome (for continuous data) or pooled incidence (for discrete data) stratified by treatment type, surgery and conservative. The squares represent the point estimate of each study with the horizontal lines denoting the 95% CI. The size of the square is proportional to the weight of each study. The center of the gray diamond is the pooled point estimate for each subgroup using a random effects model and its width reflects the 95% CI
Neck Disability Index (NDI)
Seven studies reported NDI scores, of which four for both surgically and conservatively treated patients. NDI scores were available for 700 patients, of which 156 (22%) were treated surgically. The pooled mean NDI score was 14.2 (95% CI 8.79, 19.5) for surgically treated patients and 16.0 (95% CI 12.0, 19.9) for conservatively treated patients. The difference was not clinically relevant (< 7.5), and the data were substantially heterogeneous (p-heterogeneity surgical < 0.001, I-squared 97.4%; p-heterogeneity conservative < 0.001, I-squared 98.9%).
Visual Analogue Scale (VAS) pain
Five studies reported VAS pain scores, of which one for both surgically and conservatively treated patients. VAS scores were available for 180 patients, of which 150 (83%) were treated surgically. The pooled mean VAS score was 1.53 (95% CI 1.35, 1.72) for surgically treated patients and 0.73 (95% CI 0.30, 1.16) for conservatively treated patients. The difference was not clinically relevant (< 1), and the data were substantially heterogeneous (p-heterogeneity surgical < 0.001, I-squared 98.2%).
Smiley-Webster Scale (SWS)
Six studies reported the SWS, of which two for both surgically and conservatively treated patients. Median SWS scores were available for 231 patients, of which 98 (42%) were treated surgically. Weighted median SWS score was 1 (range 1–4) for surgically treated patients, which was not clinically different from the median of 2 (range 1–4) for conservatively treated patients. Of note, both a SWS score of 1 and 2 represents return to full-time work/activity, the difference being no consumption of pain medication for 1 and occasional consumption of pain medication for 2.
Radiological outcome
Fracture union
Forty studies reported extractable fracture union rates, including thirteen that reported union rates for surgical and conservative groups (Table 2 and Fig. 2). Union data were available for 1900 patients, of which 988 (52%) were treated surgically. Union was achieved in 72.7% (95% CI 66.1%, 78.5%) of surgically treated patients and in 40.2% (95% CI 32.0%, 49.0%) of conservatively treated patients. This difference was clinically significant, although the data were substantially heterogeneous (p-heterogeneity surgical < 0.001, I-squared 75.1%; p-heterogeneity conservative < 0.001, I-squared 74.3%).
Fracture stability
Forty-one studies reported extractable fracture stability rates, including fourteen that reported stability rates for surgical and conservative groups (Table 2 and Fig. 2). Stability data were available for 1917 patients, of which 994 (52%) were treated surgically. Stability was achieved in 82.6% (95% CI 74.9%, 88.3%) of surgically treated patients and in 70.1% (95% CI 57.7%, 80.1%) of conservatively treated patients. Data were substantially heterogeneous (p-heterogeneity surgical < 0.001, I-squared 75.7%; p-heterogeneity conservative < 0.001, I-squared 88.3%).
Complications and mortality
Complications and mortality were heterogeneously reported across studies. Complications in the surgical group were mostly related to the operation, whether intraoperative (e.g., screw malposition) or postoperative (e.g., wound infections). Complications in the conservative group were mostly immobilization-related, such as pressure ulcerations and pneumonia. Analysis of a difference in complications and mortality between treatment groups was not feasible.
Meta-regression analysis
Meta-regression analysis: Fracture union
In the model including treatment type, surgically treated patients showed significantly more union than conservative treated patients when corrected for age and fracture type (p < 0.001), although data were still substantially heterogeneous (new I-squared 75.6%). Individually, increased age and fracture type were not identified to significantly influence fracture union (Table 4).
Meta-regression analysis: Fracture stability
In the model including treatment type, no significant difference in stability rates was identified between surgically and conservatively treated patients when corrected for age and fracture type (p = 0.09). Data were substantially heterogeneous (new I-squared 83.8%). Individually, increased age and fracture type were not identified to significantly influence fracture stability (Table 4).
Discussion
Multiple studies describing treatment outcomes for odontoid fractures in the elderly have been published since publication of the previous systematic review by the authors in 2013 [8]. Although these studies typically reported larger samples, only four studies included in this updated review were performed prospectively. Only one study corrected for confounding variables and was therefore classified as cohort study. The other studies were classified as case series. Reported data suffered from substantial heterogeneity. These factors limited the analyses that could be executed. As a result, no strong recommendations can be made regarding the optimal treatment for odontoid fractures in the elderly, even though interesting observations were made.
Evaluation of outcomes of odontoid fractures usually focused on the radiological outcome. Clinical outcome was less often described, but can be considered the most relevant. Focusing primarily on clinical outcomes in the current literature review, no clinically relevant differences were observed between surgically and conservatively treated patients for the NDI and VAS pain scores. Median SWS score was 1 for surgically treated patients and 2 for conservatively treated patients, although both a SWS score of 1 and 2 represents return to full-time work/activity, the difference being no consumption of pain medication for 1 and occasional consumption of pain medication for 2. This difference was also not considered clinically relevant. The clinical outcome measures that were reported in the remaining studies varied widely and could not be used for generalized conclusions.
Fracture union was achieved more often in surgically treated patients than in conservatively treated patients. This difference remained after correction for age and fracture type (II/III vs. II) in the meta-regression analysis. A similar difference in fracture stability was not identified between the treatment groups. Multiple studies used fracture union and/or stability as primary outcome, but the correlation with clinical outcome was not properly studied. It remains unclear whether patients indeed benefit clinically from favorable radiological outcomes. Consequently, debate remains as to what the exact goal of treatment should be (e.g., favorable clinical outcome, osseous union and/or fracture stability), and as to how outcome should be measured.
Patient age in the included studies was comparable between treatment groups. However, different age criteria were applied among studies, describing patients ≥ 65, ≥ 70, ≥ 75 or ≥ 80 years. Moreover, surgically and conservatively treated groups described in the included studies may not be comparable with respect to other patient characteristics (e.g., co-morbidity, osteoporosis, severity of comminution). Outcome diversification per age group among the elderly was mostly absent and needs further study. Furthermore, it is often postulated that treatment outcome depends on patient age. Other factors must, however, play some role, as different studies have shown different outcomes for the same treatment, which cannot be explained by patient age alone.
Complications and mortality were common in both treatment groups, although not uniformly reported and therefore not reliably analyzable. Complications relating to the operation, both intraoperatively (e.g., screw malposition) and postoperatively (e.g., wound infections), were the most common complications in surgically treated patients. Immobilization-related complications, such as pressure ulcerations and pneumonia, were the most prevalent complications in patients treated conservatively.
Vaccaro et al. published the only prospective cohort study included in this review that directly compared surgical to conservative treatment [27]. In this study involving 159 patients, of which 101 treated surgically, higher union rates after surgical treatment were reported. This study reported an NDI increase (clinical worsening) between baseline and 52 weeks after both surgical and conservative treatment. This increase was only significant for conservatively treated patients, even though selection bias and residual confounding may have influenced these findings (e.g., no correction for osteoporosis, no adjusted odds ratios reported). Of note, the outcomes presented in this systematic review were not comparisons between baseline and 52 weeks, but rather the pooled point estimates at 52 weeks specifically. In that respect, Vaccaro et al. reported a mean NDI at one year follow-up of 28.0 (SE 2.49) for surgically treated patients and 31.6 (SE 3.34) for conservatively treated patients, also not reaching a minimally clinically important difference (> 7.5), similar to the findings in this systematic review. As already mentioned, the most relevant outcome parameter remains debated.
Strengths and limitations
This meta-analysis had a few limitations. The studies were mostly case series with their associated limitations, such as missing data, confounding bias and variability in outcome assessment. Outcomes were not uniformly reported at 52 weeks, and, when missing, were extracted for the last available follow-up time point. As a result, data collected for this review suffered from substantial heterogeneity throughout the dataset. Meta-regression analyses were feasible for the radiological outcomes only, where only mean age and fracture type could be corrected for. Outcomes should therefore be interpreted with caution. Results were certainly affected by residual confounding. Illustrative in this respect is the study by Molinari et al, in which patients with < 50% fracture displacement were treated conservatively and patients with ≥ 50% fracture displacement were treated surgically, introducing heterogeneity between treatment groups even within one study [28]. For the primary analysis, type II and III fractures were analyzed as one group. It is plausible that type II fractures were more often treated surgically, whereas conservative management was preferred for type III fractures. This may have influenced the findings. In studies describing patients with both type II and III fractures (n = 10), results were not typically sub-grouped by fracture type. Consequently, adjustment for fracture type was only possible for type II/III versus type II (the other studies, n = 31) fractures, not for type II versus type III fractures as would ideally have been the case. Additionally, bone quality was only scarcely described, even when it is known to be an important factor in bone healing. Finally, a variety of both surgical and conservative treatments were analyzed in only two groups. Further diversification of outcomes for different surgical (e.g., anterior, posterior approach) and conservative (e.g., collar, halo vest) treatments was not deemed feasible due to the data limitations. Nevertheless, this study had some strengths. No restriction was made with regard to language or date, which led to a substantially large number of studies to be meta-analyzed for some outcomes. Consequently, this enabled the authors to conduct a multivariable meta-regression analysis to control for confounding as much as the reported data allowed. Lastly, the classic fail safe n conducted gave reassurance that publication bias was unlikely to be the reason of the asymmetry observed in a few funnel plots.
Conclusions
Implications for clinical practice
No clinically relevant differences between surgically and conservatively treated patients were identified in term of the NDI, VAS pain and SWS scores. When corrected for age and fracture type, surgically treated patients showed higher union rates than conservatively treated patients, although selection mechanisms might (partially) explain this difference. When corrected for age and fracture type, no difference in stability rates was observed between surgically and conservatively treated patients. Data were substantially heterogeneous, limiting the possibilities for analysis and strengths of the recommendations derived from these results.
Implications for research
These results need to be further confirmed in well-designed comparative studies with proper adjustment for confounding, such as age, fracture characteristics, and degree of osteoporosis. The correlation between clinical and radiological outcomes needs to be further explored.
Abbreviations
- CI:
-
95% Confidence Interval
- MCID:
-
Minimal clinically important difference
- NDI:
-
Neck Disability Index
- NOS:
-
Newcastle–Ottawa Quality Assessment Scale
- SD:
-
Standard deviation
- SE:
-
Standard error
- SWS:
-
Smiley-Webster Scale
- VAS:
-
Visual Analogue Scale
References
Grauer JN, Shafi B, Hilibrand AS, Harrop JS, Kwon BK, Breiner JM et al (2005) Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J 5(2):123–129
Hsu WK, Anderson PA (2010) Odontoid fractures: update on management. J Am Acad Orthop Surg 18(7):383–394
Shears E, Armitstead CP (2008) Surgical versus conservative management for odontoid fractures. Cochrane Database Syst Rev 4:CD005078
White AP, Hashimoto R, Norvell DC, Vaccaro AR (2010) Morbidity and mortality related to odontoid fracture surgery in the elderly population. Spine (Phila Pa 1976) 35(9 Suppl):S146–S157
Harrop JS, Hart R, Anderson PA (2010) Optimal treatment for odontoid fractures in the elderly. Spine (Phila Pa 1976) 35(21 Suppl):S219–S227
Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG (2006) Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma 60(1):199–203
Anderson LD, D’Alonzo RT (1974) Fractures of the odontoid process of the axis. J Bone Jt Surg Am 56(8):1663–1674
Huybregts JG, Jacobs WC, Vleggeert-Lankamp CL (2013) The optimal treatment of type II and III odontoid fractures in the elderly: a systematic review. Eur Spine J 22(1):1–13
Carreon LY, Glassman SD, Campbell MJ, Anderson PA (2010) Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J 10(6):469–474
Cleland JA, Fritz JM, Whitman JM, Palmer JA (2006) The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine (Phila Pa 1976) 31(5):598–602
Young BA, Walker MJ, Strunce JB, Boyles RE, Whitman JM, Childs JD (2009) Responsiveness of the neck disability index in patients with mechanical neck disorders. Spine J 9(10):802–808
Young IA, Cleland JA, Michener LA, Brown C (2010) Reliability, construct validity, and responsiveness of the neck disability index, patient-specific functional scale, and numeric pain rating scale in patients with cervical radiculopathy. Am J Phys Med Rehabil 89(10):831–839
Kelly AM (2001) The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J 18(3):205–207
Myles PS, Myles DB, Galagher W, Boyd D, Chew C, MacDonald N et al (2017) Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth 118(3):424–429
Wells A, Shea B, O'Connell D, Peterson J, Welch V, Losos M et al (2021) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Chan K, Bhandari M (2011) Three-minute critical appraisal of a case series article. Indian J Orthop 45(2):103–104
Cowley DE (1995) Prostheses for primary total hip replacement. A critical appraisal of the literature. Int J Technol Assess Health Care 11(4):770–778
University of Wales CoM (2011) Critical appraisal form 2011 [Available from: http://www.core-info.cardiff.ac.uk/thermal/FULL_COTS_critical%20appraisal%20FORM%20B%202007.pdf
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2007) Performance of the trim and fill method in the presence of publication bias and between-study heterogeneity. Stat Med 26(25):4544–4562
Fehlings MG, Arun R, Vaccaro AR, Arnold PM, Chapman JR, Kopjar B (2013) Predictors of treatment outcomes in geriatric patients with odontoid fractures: AOSpine North America multi-centre prospective GOF study. Spine (Phila Pa 1976) 38(11):881–886
Smith JS, Kepler CK, Kopjar B, Harrop JS, Arnold P, Chapman JR et al (2013) Effect of type II odontoid fracture nonunion on outcome among elderly patients treated without surgery: based on the AOSpine North America geriatric odontoid fracture study. Spine (Phila Pa 1976) 38(26):2240–2246
Raudenbush B, Molinari R (2015) Longer-term outcomes of geriatric odontoid fracture nonunion. Geriatr Orthop Surg Rehabil 6(4):251–257
Molinari RW, Dahl J, Gruhn WL, Molinari WJ (2013) Functional outcomes, morbidity, mortality, and fracture healing in 26 consecutive geriatric odontoid fracture patients treated with posterior fusion. J Spinal Disord Tech 26(3):119–126
Molinari RW, Khera OA, Gruhn WL, McAssey RW (2012) Rigid cervical collar treatment for geriatric type II odontoid fractures. Eur Spine J 21(5):855–862
Faure A, Prost S, Mansouri N, Farah K, Blondel B, Fuentes S (2018) Odontoid fracture in patients age >75 years surgically managed by the harms technique: bone healing and 1-year mortality rate in 57 cases. World Neurosurg 116:e1087–e1091
Josten C, Jarvers JS, Glasmacher S, Spiegl UJ (2018) Odontoid fractures in combination with C1 fractures in the elderly treated by combined anterior odontoid and transarticular C1/2 screw fixation. Arch Orthop Trauma Surg 138(11):1525–1531
Vaccaro AR, Kepler CK, Kopjar B, Chapman J, Shaffrey C, Arnold P et al (2013) Functional and quality-of-life outcomes in geriatric patients with type-II dens fracture. J Bone Jt Surg Am 95(8):729–735
Molinari WJ 3rd, Molinari RW, Khera OA, Gruhn WL (2013) Functional outcomes, morbidity, mortality, and fracture healing in 58 consecutive patients with geriatric odontoid fracture treated with cervical collar or posterior fusion. Glob Spine J 3(1):21–32
Chibbaro S, Mallereau CH, Ganau M, Zaed I, Teresa Bozzi M, Scibilia A et al (2021) Odontoid type II fractures in elderly: What are the real management goals and how to best achieve them? A multicenter European study on functional outcome. Neurosurg Rev
Moscolo F, Meneghelli P, Boaro A, Impusino A, Locatelli F, Chioffi F et al (2021) The use of Grauer classification in the management of type II odontoid fracture in elderly: Prognostic factors and outcome analysis in a single centre patient series. J Clin Neurosci 89:26–32
McIlroy S, Lam J, Khan MF, Mirza AB, Philip JA, Grahovac G et al (2020) Conservative management of type II odontoid fractures in older people: a retrospective observational comparison of osseous union versus nonunion. Neurosurgery 87(6):E648–E654. https://doi.org/10.1093/neuros/nyaa256. PMID: 32570274
Gembruch O, Lemonas E, Ahmadipour Y, Sure U, El Hindy N, Dodel R et al (2019) Treatment of odontoid type II fractures in octogenarians: balancing two different treatment strategies. Neurospine 16(2):360–367
Girardo M, Rava A, Gargiulo G, Coniglio A, Artiaco S, Masse A et al (2018) Clinical and radiological union rate evaluation of type 2 odontoid fractures: a comparison between anterior screw fixation and halo vest in elderly patients. J Craniovertebr Junction Spine 9(4):254–259
Lofrese G, Musio A, De Iure F, Cultrera F, Martucci A, Iaccarino C et al (2019) Type II odontoid fracture in elderly patients treated conservatively: Is fracture healing the goal? Eur Spine J 28(5):1064–1071
Alhashash M, Shousha M, Gendy H, Barakat AS, Boehm H (2018) Percutaneous posterior transarticular atlantoaxial fixation for the treatment of odontoid fractures in the elderly: a prospective study. Spine (Phila Pa 1976) 43(11):761–766
Aquila F, Tacconi L, Baldo S (2018) Type II fractures in older adults: Can they be treated conservatively?: A single-center experience and review of the literature. World Neurosurg 118:e938–e945
Scholz C, Klingler JH, Scheiwe C, Naseri Y, Masalha W, Hubbe U (2018) Atlantoaxial instability in patients older than 70 years: What is the outcome when further conservative treatment is not an option? J Neurol Surg Part A Cent Eur Neurosurg 79(5):372–379
Ishak B, Schneider T, Gimmy V, Unterberg AW, Kiening KL (2017) Early complications, morbidity, and mortality in octogenarians and nonagenarians undergoing posterior intra-operative spinal navigation-based C1/2 fusion for type II odontoid process fractures. J Neurotrauma 34(24):3326–3335
Dobran M, Nasi D, Esposito DP, Iacoangeli M (2016) Posterior fixation with C1 lateral mass screws and C2 pars screws for type II odontoid fracture in the elderly: long-term follow-up. World Neurosurg 96:152–158
Joestl J, Lang N, Bukaty A, Platzer P (2016) A comparison of anterior screw fixation and halo immobilisation of type II odontoid fractures in elderly patients at increased risk from anaesthesia. Bone Jt J 98-b:1222–1226
Josten C, Jarvers JS, Glasmacher S, Heyde CE, Spiegl UJ (2016) Anterior transarticular atlantoaxial screw fixation in combination with dens screw fixation for type II odontoid fractures with associated atlanto-odontoid osteoarthritis. Eur Spine J 25(7):2210–2217
Henaux PL, Cueff F, Diabira S, Riffaud L, Hamlat A, Brassier G et al (2011) Anterior screw fixation of type IIB odontoid fractures in octogenarians. Eur Spine J 21:335–339
Hou Y, Yuan W, Wang X (2011) Clinical evaluation of anterior screw fixation for elderly patients with type II odontoid fractures. J Spinal Disord Tech 24:E75–E81
Osti M, Philipp H, Meusburger B, Benedetto KP (2011) Analysis of failure following anterior screw fixation of type II odontoid fractures in geriatric patients. Eur Spine J 20:1915–1920
Butler JS, Dolan RT, Burbridge M, Hurson CJ, O’Byrne JM, McCormack D et al (2010) The long-term functional outcome of type II odontoid fractures managed non-operatively. Eur Spine J 19(10):1635–1642
Lefranc M, Peltier J, Fichten A, Desenclos C, Toussaint P, Le GD (2009) Odontoid process fracture in elderly patients over 70 years: morbidity, handicap, and role of surgical treatment in a retrospective series of 27 cases. Neurochirurgie 55(6):543–550
Kaminski A, Gstrein A, Muhr G, Muller EJ (2008) Transarticular C1–C2 screw fixation: results of unstable odontoid fractures and pseudarthrosis in the elderly. Unfallchirurg 111(3):167–172
Koech F, Ackland HM, Varma DK, Williamson OD, Malham GM (2008) Nonoperative management of type II odontoid fractures in the elderly. Spine (Phila Pa 1976) 33(26):2881–2886
Platzer P, Thalhammer G, Oberleitner G, Schuster R, Vecsei V, Gaebler C (2007) Surgical treatment of dens fractures in elderly patients. J Bone Jt Surg Am 89(8):1716–1722
Seybold EA, Bayley JC (1998) Functional outcome of surgically and conservatively managed dens fractures. Spine (Phila Pa 1976) 23(17):1837–1845
Traynelis VC, Fontes RBV, Abode-Iyamah KO, Cox EM, Greenlee JD (2021) Posterior fusion for fragility type 2 odontoid fractures. J Neurosurg Spine 35:644–650
Allia J, Darmante H, Barresi L, De Peretti F, Trojani C, Bronsard N (2020) Early mortality and morbidity of odontoid fractures after 70 years of age. Orthop Traumatol Surg Res 106:1399–1403
Hong J, Zaman R, Coy S, Pastel D, Simmons N, Ball P et al (2018) A cohort study of the natural history of odontoid pseudoarthrosis managed nonoperatively in elderly patients. World Neurosurg 114:e1007–e1015
Perry A, Graffeo CS, Carlstrom LP, Chang W, Mallory GW, Puffer RC et al (2018) Fusion, failure, fatality: long-term outcomes after surgical versus nonoperative management of type II odontoid fracture in octogenarians. World Neurosurg 110:e484–e489
Schwarz F, Lawson McLean A, Waschke A, Kalff R (2018) Cement-augmented anterior odontoid screw fixation in elderly patients with odontoid fracture. Clin Neurol Neurosurg 175:144–148
Faure A, Graillon T, Pesenti S, Tropiano P, Blondel B, Fuentes S (2017) Trends in the surgical management of odontoid fractures in patients above 75 years of age: retrospective study of 70 cases. Orthop Traumatol Surg Res 103(8):1221–1228
Waschke A, Ullrich B, Kalff R, Schwarz F (2016) Cement-augmented anterior odontoid screw fixation for osteoporotic type II odontoid fractures in elderly patients: prospective evaluation of 11 patients. Eur Spine J 25(1):115–121
Bisson EF, Mumert ML, Mazur MD, Dailey AT, Schmidt MH (2015) The fate of type II odontoid fractures after posterior atlantoaxial fusion: Where does healing occur? J Neurol Surg Part A Cent Eur Neurosurg 76(4):274–278
Scheyerer MJ, Zimmermann SM, Simmen HP, Wanner GA, Werner CM (2013) Treatment modality in type II odontoid fractures defines the outcome in elderly patients. BMC Surg 13:54
Dailey AT, Hart D, Finn MA, Schmidt MH, Apfelbaum RI (2010) Anterior fixation of odontoid fractures in an elderly population. J Neurosurg Spine 12(1):1–8
Koivikko MP, Kiuru MJ, Koskinen SK, Myllynen P, Santavirta S, Kivisaari L (2004) Factors associated with nonunion in conservatively-treated type-II fractures of the odontoid process. J Bone Jt Surg Br 86(8):1146–1151
Borm W, Kast E, Richter HP, Mohr K (2003) Anterior screw fixation in type II odontoid fractures: Is there a difference in outcome between age groups? Neurosurgery 52(5):1089–1092
Andersson S, Rodrigues M, Olerud C (2000) Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J 9(1):56–59
Kuntz C, Mirza SK, Jarell AD, Chapman JR, Shaffrey CI, Newell DW (2000) Type II odontoid fractures in the elderly: early failure of nonsurgical treatment. Neurosurg Focus 8(6):e7
Berlemann U, Schwarzenbach O (1997) Dens fractures in the elderly. Results of anterior screw fixation in 19 elderly patients. Acta Orthop Scand 68(4):319–324
Hanigan WC, Powell FC, Elwood PW, Henderson JP (1993) Odontoid fractures in the elderly patient. In: Clinical research 41(3):A710-A710
Hanssen AD, Cabanela ME (1987) Fractures of the dens in adult patients. J Trauma 27(8):928–934
Acknowledgements
The authors are thankful to Mr. Jan Schoones of the Walaeus Library for carrying out the database search. The authors are thankful to Mr. Samuel B. Polak, MD, for his assistance in reference selection.
Funding
The authors did not receive support from any organization for the submitted work. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Karma A. Barot and Camila Recio are co-junior authors.
Rania A. Mekary and Carmen L. A. Vleggeert-Lankamp are co-senior authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huybregts, J.G.J., Barot, K.A., Recio, C. et al. The optimal treatment of type II and III odontoid fractures in the elderly: an updated meta-analysis. Eur Spine J 32, 3434–3449 (2023). https://doi.org/10.1007/s00586-023-07779-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07779-1