Abstract
Purpose
Frailty is caused by age-related decline in physical function, which may contribute to worsening spinal alignment. Cardiovascular Health Study (CHS)-criteria for assessing physical function seem more appropriate than frailty index which evaluate comorbiduty. However, there have been no reports investigating the relationship between frailty and spinal alignment using the CHS criteria. This study aimed to examine spinal radiographic parameters using the CHS criteria in volunteers participating in a health screening study.
Methods
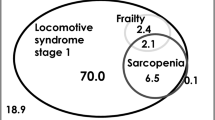
The subjects were 211 volunteers (71 males and 140 females) aged 60–89 years old who participated in the TOEI study in 2018 and 2020. They were divided into three groups (R: robust, PF: pre-frailty, and F: frailty) according to the score of the Japanese version of the CHS (J-CHS) criteria in 2018. The radiographic parameters were evaluated using a whole-spine standing X-ray.
Results
There were 67 volunteers in group R, 124 volunteers in group PF, and 20 volunteers in group F. Of the five items in the J-CHS criteria, low activity was the most common in the PF group (64%). Low activity was also the most common in the F group (100%). Regarding spinal alignment, significant differences were found in C7SVA in 2020 (R:PF:F = 26:31:62 mm, P = 0.047), C2SVA in 2018 (20:34:63 mm, P = 0.019), and C2SVA in 2020 (37:47:78 mm, P = 0.041).
Conclusion
Frailty was associated with a worsening in global alignment along the 2- year follow up. The frailty may begin with a decrease in activity and progression of exhaustion; preventing this progression is important through motivation to exercise.
Level of evidence
II



Similar content being viewed by others
References
Buchner DM, Wagner EH (1992) Preventing frail health. Clin Geriatr Med 8:1–17. https://doi.org/10.1016/S0749-0690(18)30494-4
Cardiovascular Health Study Collaborative Research Group, Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M156. https://doi.org/10.1093/gerona/56.3.m146
Mitnitski AB, Mogilner AJ, Rockwood K (2001) Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal 1:323–336. https://doi.org/10.1100/tsw.2001.58
Veronesi F, Borsari V, Martini L, Visani A, Gasbarrini A, Brodano GB, Fini M (2021) The impact of frailty on spine surgery: systematic review on 10 years clinical studies. Aging Dis 12:625–645. https://doi.org/10.14336/AD.2020.0904
Kitamura K, van Hooff M, Jacobs W, Watanabe K, de Kleuver M (2022) Which frailty scales for patients with adult spinal deformity are feasible and adequate? A systematic review. Spine J 22:1191–1204. https://doi.org/10.1016/j.spinee.2022.01.017
Leven DM, Lee NJ, Kothari P, Steinberger J, Guzman J, Skovrlj B, Shin JI, Caridi JM, Cho SK (2016) Frailty index is a significant predictor of complications and mortality after surgery for adult spinal deformity. Spine 41:E1394–E1401. https://doi.org/10.1097/BRS.0000000000001886
International Spine Study Group, Miller EK, Neuman BJ, Jain A, Daniels AH, Ailon T, Sciubba DM, Kebaish KM, Lafage V, Scheer JK, Smith JS, Bess S, Shaffrey CI, Ames CP (2017) An assessment of frailty as a tool for risk stratification in adult spinal deformity surgery. Neurosurg Focus 43:E3. https://doi.org/10.3171/2017.10.FOCUS17472
European Spine Study Group, International Spine Study Group, Miller EK, Vila-Casademunt A, Neuman BJ, Sciubba DM, Kebaish KM, Smith JS, Alanay A, Acaroglu ER, Kleinstück F, Obeid I, Sánchez Pérez-Grueso FJ, Carreon LY, Schwab FJ, Bess S, Scheer JK, Lafage V, Shaffrey CI, Pellisé F, Ames CP (2018) External validation of the adult spinal deformity (ASD) frailty index (ASD-FI). Eur Spine J 27:2331–2338. https://doi.org/10.1007/s00586-018-5575-3
AOSpine Knowledge Forum, Miller EK, Lenke LG, Neuman BJ, Sciubba DM, Kebaish KM, Smith JS, Qiu Y, Dahl BT, Pellise F, Matsuyama Y, Carreon LY, Fehlings MG, Cheung KM, Lewis S, Dekutoski MB, Schwab FJ, Boachie-Adjei O, Mehdian H, Bess S, Shaffrey CI, Ames CP (2018) External Validation of the Adult Spinal Deformity (ASD) Frailty Index (ASD-FI) in the Scoli-RISK-1 Patient Database Deformity tISSG. Spine 43:1426–1431. https://doi.org/10.1097/BRS.0000000000002717
Satake S, Arai H (2020) The revised Japanese version of the Cardiovascular Health Study criteria (revised J-CHS criteria). Geriatr Gerontol Int 20:992–993. https://doi.org/10.1111/ggi.14005
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148. https://doi.org/10.1002/jbmr.5650080915
Oe S, Yamato Y, Hasegawa T, Yoshida G, Kobayashi S, Yasuda T, Banno T, Arima H, Mihara Y, Ushirozako H, Yamada T, Ide K, Watanabe Y, Togawa D, Niwa H, Matsuyama Y (2020) Deterioration of sagittal spinal alignment with age originates from the pelvis not the lumbar spine: a 4-year longitudinal cohort study. Eur Spine J 29:2329–2339. https://doi.org/10.1007/s00586-020-06431-6
Yagi M, Michikawa T, Hosogane N, Fujita N, Okada E, Suzuki S, Tsuji O, Nagoshi N, Asazuma T, Tsuji T, Nakamura M, Matsumoto M, Watanabe K (2019) The 5-item modified frailty index is predictive of severe adverse events in patients undergoing surgery for adult spinal deformity. Spine 44:E1083–E1091. https://doi.org/10.1097/BRS.0000000000003063
Akbik OS, Al-Adli N, Pernik MN, Hicks WH, Hall K, Aoun SG, Bagley CA (2022) A comparative analysis of frailty, disability, and sarcopenia with patient characteristics and outcomes in adult spinal deformity surgery. Glob Spine J. https://doi.org/10.1177/21925682221082053
Kojima G, Iliffe S, Taniguchi Y, Shimada H, Rakugi H, Walters K (2017) Prevalence of frailty in Japan: a systematic review and meta-analysis. J Epidemiol 27:347–353. https://doi.org/10.1016/j.je.2016.09.008
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC (2012) Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 60:1487–1492. https://doi.org/10.1111/j.1532-5415.2012.04054.x
Flexman AM, Charest-Morin R, Stobart L, Street J, Ryerson CJ (2016) Frailty and postoperative outcomes in patients undergoing surgery for degenerative spine disease. Spine J 16:1315–1323. https://doi.org/10.1016/j.spinee.2016.06.017
Kim HK, Suzuki T, Saito K, Yoshida H, Kobayashi H, Kato H, Katayama M (2012) Effects of exercise and amino acid supplementation on body composition and physical function in community-dwelling elderly Japanese sarcopenic women: a randomized controlled trial. J Am Geriatr Soc 60:16–23. https://doi.org/10.1111/j.1532-5415.2011.03776.x
Oe S, Togawa D, Nakai K, Yamada T, Arima H, Banno T, Yasuda T, Kobayasi S, Yamato Y, Hasegawa T, Yoshida G, Matsuyama Y (2015) The influence of age and sex on cervical spinal alignment among volunteers aged over 50. Spine 40:1487–1494. https://doi.org/10.1097/BRS.0000000000001071
Uehara M, Takahashi J, Ikegami S, Tokida R, Nishimura H, Sakai N, Kato H (2019) Sagittal spinal alignment deviation in the general elderly population: a Japanese cohort survey randomly sampled from a basic resident registry. Spine J 19:349–356. https://doi.org/10.1016/j.spinee.2018.06.346
Funding
This study was funded by Medtronic Sofamor Danek Inc., Japan Medical Dynamic Marketing Inc., and Meitoku Medical Institution Jyuzen Memorial Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shin Oe and Yu Yamato are members of the Division of Geriatric Musculoskeletal Health, which is funded by a donor.
Consent for publication
Informed consent was obtained from all individual participants.
Ethical approval
The study protocol was approved by the institutional review board of Hamamatsu University School of Medicine, Shizuoka, Japan (IRB No.22-089).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oe, S., Yamato, Y., Hasegawa, T. et al. The relationship between frailty and spinal alignment in the elderly general population: a two-year longitudinal study. Eur Spine J 32, 2266–2273 (2023). https://doi.org/10.1007/s00586-023-07759-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07759-5