Abstract
Purpose
Indication for surgical decompression in metastatic spinal cord compression (MSCC) is often based on prognostic scores such as the modified Bauer score (mBs), with favorable prognosis suggestive of surgery and poor prognosis of non-surgical management. This study aimed to clarify if (1) surgery may directly affect overall survival (OS) aside from short-term neurologic outcome, (2) explore whether selected patient subgroups with poor mBs might still benefit from surgery, and (3) gauge putative adverse effects of surgery on short-term oncologic outcomes.
Methods
Single-center propensity score analyses with inverse-probability-of-treatment-weights (IPTW) of OS and short-term neurologic outcomes in MSCC patients treated with or without surgery between 2007 and 2020.
Results
Among 398 patients with MSCC, 194 (49%) underwent surgery. During a median follow-up of 5.8 years, 355 patients (89%) died. MBs was the most important predictor for spine surgery (p < 0.0001) and the strongest predictor of favorable OS (p < 0.0001). Surgery was associated with improved OS after accounting for selection bias with the IPTW method (p = 0.021) and emerged as the strongest determinant of short-term neurological improvement (p < 0.0001). Exploratory analyses delineated a subgroup of patients with an mBs of 1 point who still benefited from surgery, and surgery did not result in a higher risk of short-term oncologic disease progression.
Conclusion
This propensity score analysis corroborates the concept that spine surgery for MSCC associates with more favorable neurological and OS outcomes. Selected patients with poor prognosis might also benefit from surgery, suggesting that even those with low mBs may be considered for this intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal metastases occur in 40% of cancer patients, and in up to 20% of these cases further progression to symptomatic metastatic spinal cord compression (MSCC) may occur [1, 2]. While spinal decompression surgery and stabilization is an established treatment strategy for MSCC, selection of patients who will benefit from surgery is challenging in clinical practice, since any patient-individual treatment strategy must provide the maximum palliative and minimum operative morbidity effect [3]. In this context, the Modified Bauer score (mBs) to predict overall survival (OS) provides a rational selection basis for a proper treatment strategy based on the sum of four simple variables (assigning one point each for: no visceral metastases, no lung cancer, solitary skeletal metastases, and the tumor entities breast, kidney, lymphoma, and myeloma) [4, 5]. Recommendations range from extensive surgery for patients with beneficial prognosis (mBs: 3–4 points), limited surgery for moderate prognosis (mBs: 2 points), and non-operative supportive care for patients with poor prognosis [mBs: 0–1 point(s)] [6].
This allocation naturally results in a selection bias, as patients with a favorable prognosis prediction are more likely to be selected for surgery. While the beneficial effect of surgical decompression and stabilization on neurologic outcome in MSCC has been demonstrated in a prospective randomized setting and a meta-analysis [7, 8], and the correlation between low disease load with long time post-operative survival has been proven prospectively [9], the question whether surgery itself might directly affect clinical outcome and prognosis, probably even in patients with unfavorable mBs scores, remains unclear. As decompression surgery in MSCC is an established and recommended technique in patients with good prognosis, performing a randomized controlled trial to examine overall survival outcomes of treatment with and without spine surgery is challenging from an ethical standpoint. On the other hand, in clinical practice, patients may undergo surgery despite their mBs stratification being indicative of poor prognosis or be treated without surgery in case of beneficial prognosis. In this setting of a non-randomized treatment allocation, propensity score analysis on observational data is an accepted method to minimize the mentioned selection bias and explore which patients could directly benefit from decompressive surgery [10, 11].
While the benefit of surgery on neurologic outcomes in MSCC is less debated, an ongoing discussion revolves around potential adverse effects of spine surgery on oncologic outcomes. It is not unplausible that in a metastatic cancer patient with high burden of malignant disease, a surgical intervention might have the potential to weaken a patient’s condition, which in turn might trigger disease progression [12].
Therefore, we conducted this study to clarify if (1) aside from earlier reported neurological improvement, surgery for MSCC may also directly affect OS, (2) explore whether certain patients in whom surgery is not primarily recommended based on prognostic scores might benefit from surgery, and (3) gauge putative adverse effects of surgery on short-term oncologic outcomes.
Methods
Ethics statement
This study was approved by the local Institutional Ethical Review Board (IRB) (Reference number: EK-Nr. 30-252 ex 17/18) and performed in accordance with relevant guidelines and regulations; informed consent for later retrospective analysis of their data was obtained from all participants.
Study population
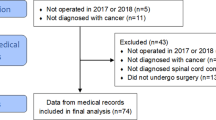
All referrals (n = 1788) to a single orthopedic surgery department for evaluation of radiologically confirmed spinal metastases between 2007 and 2020 were retrospectively included in this study (Supplementary Fig. 1). Case history and clinical follow-up were retrieved from the hospital’s intern, and associated centers’ data systems using keyword identification of all written examination reports, complete follow-up on all-cause mortality for all patients’ data/dates were received from insurance data. Demographic data and cancer specific medical history (first diagnosis and entity; date of any new metastasis; spinal metastasis including location, date, fracture; onset of MSCC, neurologic impairment (Frankel scale A-D) and recovery (at least Frankel scale D; or E if D initially) within the first 6 weeks of decision, mBs, date of decision and surgery and/or radiation) were collected from all patients. No patients with intradural metastases were included in this study.
MSCC and institutional standard procedure
Patients with symptomatic MSCC with neurologic impairment (n = 398) and timepoint of onset of symptom were identified from our data system. A decision (A) decompressive surgery with dorsal stabilization and subsequent recommendation of radiation (B) no surgery, recommendation of radiation was documented in all cases. According to our clinic internal protocol, this decision was based on the calculated mBs, time since onset of neurologic impairment, general health state, and patients’ consent to surgery. Extent of surgical intervention was performed according to mBs recommendation in most cases [6]. Radiation was recommended in all MSCC cases, if residual radiation dose was available for the region involved.
Statistical methods
All statistical analyses were performed by FP with Stata (Windows version 17.0, Stata Corp., Houston, TX, USA). Continuous variables were reported as medians [25th–75th percentile] and count data as absolute frequencies (column %). The distribution of variables between two or more other variables was assessed with rank-sum tests, χ2-tests, and Fisher’s exact tests, as appropriate. Risks of death-from-any-cause (overall survival) and progression-free survival were estimated with 1-Kaplan–Meier estimators, compared between two or more groups with log-rank tests, and modeled with uni- and multivariable Cox regression models. Risks of radiographic disease progression were estimated with competing risk cumulative incidence estimators accounting for death-from-any-cause as the competing event of interest, compared between two or more groups with Gray’s test, and modeled with Fine and Gray competing risk regression models. Predictors of spine surgery were examined with logistic regression. The magnitude of difference in the distribution of variables between patients with and without spine surgery was quantified with standardized mean differences (SMDs). Propensity score analyses were performed with inverse-probability-of-treatment-weights (IPTW), and balance diagnostics were performed as previously described. The propensity score model was developed on multiply imputed data (chained equations algorithm, 10 imputation datasets, separate imputation models for continuous, binary, and ordinal variables) including all ten available variables of the dataset, whereas other analyses were done according to the complete-case principle. The full analysis code is available on reasonable request from FP (florian.posch@medunigraz.at).
Results
Study cohort
Of 1778 referrals to our department for orthopedic evaluation of radiologically confirmed spinal metastases, 398 patients had symptomatic MSCC with neurologic impairment (Table 1). Median age was 66 years [25th–75th percentile: 56–74], and 144 patients (36%) were female. The most frequent tumor entities were prostate, lung, and breast cancer. During a median follow-up of 5.8 years according to the reverse Kaplan–Meier estimator and 0.5 years according to the median of observation times, 355 patients (89%) died. This corresponded to 3-month, 6-month, 12-month, and 3-year all-cause mortality of 34% (95%CI 30–39), 51% (95%CI 46–56), 64% (95%CI 59–69), and 85% (95%CI 81–88), respectively (Supplementary Fig. 2).
Spine surgery for symptomatic MSCC with neurologic impairment
One-hundred-ninety-four patients (49%) were treated with spine surgery, whereas the remaining 204 patients were treated non-surgically. The most important predictor of spine surgery was the mBs; twenty-eight percent, 34%, 52%, 64%, and 81% of patients with mBs of 0, 1, 2, 3, and 4 points were treated with surgery, respectively (p < 0.0001). Other predictors of spine surgery were younger age, a pathologic fracture, and selected tumor entities (e.g., breast cancer, renal cancer, endocrine cancer), whereas brain metastases or a new metastatic site in the 3 prior months were associated with lower odds of spine surgery (Table 2).
Predictors of overall survival outcomes
A low mBs emerged as the strongest predictor for an adverse survival experience. In detail, 6-month mortality estimates were 82%, 75%, 46%, 32%, and 0% in patients with mBs of 0, 1, 2, 3, and 4 points, respectively (log-rank p < 0.0001, Fig. 1). In further univariable analysis, factors associated with more favorable survival were younger age, selected tumor entities (e.g., breast cancer, sarcoma, and renal cell cancer), no brain metastases, no new metastatic sites within the preceding 3 months, and treatment with spine surgery (Table 3).
Risk of death-from-any-cause according to the modified Bauer score. Curves were obtained with 1-Kaplan–Meier estimators. Vertical ticks on the curves represent censored observations. The modified Bauer score externally validates as a strong prognostic factor for mortality in patients with malignant spinal cord compression
Overall survival outcomes with spine surgery versus non-surgical management–Propensity score analysis
Patients who were treated with spine surgery had more favorable survival outcomes than patients being treated non-surgically (6-month mortality: 46% vs. 81%, log-rank p < 0.0001, Hazard ratio (HR) = 0.43, 95%CI 0.34–0.54, p < 0.0001, Fig. 2A). However, spine surgery was associated with many favorable prognostic factors for survival such as a higher mBs (Table 1). The association between spine surgery and lower mortality prevailed after accounting for the mBs in stratified analysis (stratified log-rank p < 0.0001) as well as multivariable analysis (HR for all-cause death for spine surgery adjusted for the mBs = 0.57, 0.45–0.72, p < 0.0001). Nonetheless, we still anticipated bias in comparing outcomes between patients with and without spine surgery due to the non-random indication of this procedure in our retrospective study. To control this anticipated selection bias, we performed a propensity score analysis. The propensity score model (Supplementary Table 1) included all ten variables available to us, and the resulting propensity score covered the whole probability range from 0 to 1 (Supplementary Fig. 3A). The resulting IPTW (Supplementary Fig. 3B) led to a considerable reduction in standardized mean differences and statistical significances between patients who were treated with and without spine surgery including in the most important prognostic variables such as the mBs and brain metastases (Supplementary Fig. 4, Table 1). In IPTW-analysis, spine surgery was still associated with more favorable survival outcomes (IPTW-adjusted log-rank p = 0.021, Fig. 2B, IPTW-Adjusted HR for death with spine surgery = 0.68, 0.49–0.94, p = 0.021).
Risk of death-from-any-cause according to spine surgery—Unadjusted and propensity score analysis results. Panel A–Unadjusted 1-Kaplan–Meier analysis. Panel B–1-Kaplan–Meier analysis with inverse probability of treatment weighting (ITPW, i.e., propensity score analysis. Spine surgery emerged as a predictor of a more favorable survival experience in both unadjusted analysis (Panel A) and after controlling for selection bias with propensity score analysis (Panel B)
Subanalysis–Survival outcomes analyses by modified Bauer score
In subanalysis, spine surgery appeared to be associated with favorable overall survival across all mBs groups except in those patients with a mBs of 0 points (p for interaction = 0.058, Fig. 3). Also, in patients with a mBs of 1 point (n = 91), patients who were treated with spine surgery (n = 31) experienced a more favorable OS prognosis than patients not treated with spine surgery (1-year mortality: 63% vs. 92%, log-rank p = 0.0003, Fig. 4). This suggested that there may be a subgroup within this mBs group that may benefit from spine surgery. To further delineate those patients, we explored predictors of OS in patients with an mBs of 1 point (Table 4). Here, lower age, female sex, non-genitourinary malignancies, and no new metastatic sites within the preceding 3 months emerged as variables for delineating patients with an mBs of 1 point and a more favorable OS prognosis.
Associations of spine surgery with death-from-any-cause across subgroups of the modified Bauer score. Data represent hazard ratios with 95% confidence intervals from Cox regression models. The upper panel is from an unadjusted analysis, and the lower panel from a multivariable analysis adjusting for age and any new metastatic site within 3 months prior decision. Blue diamonds are hazard ratios, and the grey boxes around these diamonds are proportional in size to the number of patients in that modified Bauer score group. The results show that spine surgery is associated with a more favorable survival experience in all modified Bauer score subgroups except the group with a modified Bauer score of 0 points
Risk of death-from-any-cause according to spine surgery in patients with a modified Bauer score of 1 point (n = 91). Curves are from 1-Kaplan–Meier estimators. The figure shows that spine surgery is associated with lower risk of death-from-any-cause within the subgroup of patients with a modified Bauer score of 1, suggesting that selected patients with a modified Bauer score of 1 may derive some overall survival benefit from spine surgery
Subanalysis–Progression of disease after surgery
One-hundred-and-five patients experienced radiographic disease progression after spine surgery. The risk of radiographic disease progression was significantly higher in patients undergoing spine surgery than in patients treated without spine surgery (6-month competing risk cumulative incidences: 20.9% vs. 11.8%, Gray’s test p = 0.016, Supplementary Fig. 5A), and this association weakened after adjusting for the mBs (Subdistribution hazard ratio (SHR) for radiographic disease progression with spine surgery adjusted for mBs = 1.51, 0.86–2.64, p = 0.151). Given the more favorable OS with spine surgery reported above, this association likely indicated reverse causality. We therefore performed a joint analysis of radiographic progression and mortality [i.e., progression-free survival (PFS)], in which spine surgery was associated with more favorable PFS (6-month risk of radiographic progression or death: 46.4% vs. 74.9%, log-rank p < 0.0001, HR for radiographic progression or death with spine surgery = 0.45, 0.34–0.58, p < 0.0001, Supplementary Fig. 5B).
Exploratory analysis–Short-term neurologic outcome
A subset of 71% of our cohort (n = 281) had data on short-term neurologic outcome available (described in the Methods section). Here, any neurologic improvement was seen in 126 (75%) of the 168 patients undergoing spine surgery, and 21 (19%) of the 113 patients treated without spine surgery (χ2 p < 0.0001). Spine surgery and the mBs were the strongest determinants of neurologic improvement (Fig. 5, Supplementary Table 2).
Proportion of patients with any neurologic improvement—Distribution by spine surgery status and modified Bauer score. Data were only available for a subset of n = 281 patients. The figure shows that spine surgery is associated with a higher proportion of patients with neurologic improvement, and higher-modified Bauer score is associated with a higher probability of neurologic improvement
Discussion
This study was motivated by the current uncertainty regarding the potential beneficial or detrimental effect of spine surgery for MSCC patients beyond the established positive effect on immediate neurological improvement. We sought to clarify this question performing an IPTW analysis on the largest cohort of MSCC patients to date, with comparable characteristics to earlier published cohorts concerning distribution of tumor entities, localization of spinal metastasis, incidence of MSCC and overall survival [2, 4]. Similar to earlier publications [4], the mBs consistently validated as an accurate tool for mortality risk stratification of MSCC patients in our cohort. Notably, our data revealed that a higher mBs was also prognostic for improved short-term neurologic outcome, externally validating the mBs as a solid tool for both assessing short-term overall survival and potential neurologic improvement, irrespective of surgical management in patients with MSCC.
As intended by this study, aside from earlier reported neurological improvement [8], our results from the IPTW analysis suggest for the first time that surgical decompression and stabilization in MSCC are associated with improved OS. Our analysis further suggests this positive OS effect even in certain patients in whom surgery is not primarily recommended based on pre-operative mBs.
A possible explanation for this finding might be the correlation of recent immobilization with pulmonary embolism and increased mortality [13]. Additionally, oncologists often indicate antineoplastic therapy based on performance status, wherefore patients with low Karnofsky indices or high Eastern Cooperative Oncology Group (ECOG) performance scores are not considered candidates for further chemotherapy [14]. Consequently, a better health status resulting from decompressive spine surgery may lead to a higher dose-density of oncologic therapy.
Although the “tumor-debulking” effect of decompressive spine surgery is likely limited, an OS benefit of spine surgery is also conceivable considering the recent literature on improved OS with metastasectomy in colorectal cancer [15] soft tissue sarcoma [16] and renal cell carcinoma [11] as well as the OS benefit of stereotactic radiotherapy in oligometastatic cancers [17].
Coming to the question, which factors beyond the mBs might still lead to a benefit from surgery in terms of improved OS, our analysis suggests that younger patient age, non-genitourinary malignancies, and no brain metastasis or new metastatic sites within the last 3 months additionally determined the OS experience. The detrimental OS effect of brain metastasis and short time interval since last tumor progression is in line with earlier published data from a retrospective multivariate analysis on 62 patients [18].
These results demonstrate that several variables inform prognosis beyond the mBs, delineating a subgroup of patients with poor survival prediction, who still had a benefit from surgery in terms of improved OS, most significantly when they were young, female, had no genitourinary malignancy, and have had no new metastatic sites within the preceding 3 months. As an early surgical intervention within 24 h of MSCC diagnosis is an established factor for improved neurologic outcome [2], our results may also help refining surgical indication in this acute setting where comprehensive staging exams are often not available, and thus, a full mBs variable set cannot be computed.
In summary, our data suggest that the weight of prognostic considerations for the indication of decompressive surgery in MSCC may be reduced, especially in the acute setting. This is in line with recent studies, suggesting baseline performance status should take priority over expected survival in the surgical decision-making process [3, 19]. Other authors, reporting rapid improvement of quality of life and pain relief following spine surgery for MSCC, sustaining for up to 2 years after surgery [20, 21], may also support this approach.
Finally, we aimed to address the ongoing discussion concerning the impact of surgical stress on tumor progression and promotion of new metastases as possible contradictors for surgical intervention in palliative patients [12, 22]. Although the risk of disease progression was significantly higher in patients undergoing spine surgery, our data indicate that this is caused by reverse causality, due to more favorable overall survival and more staging examinations performed. Indeed, a joint analysis of progression and mortality revealed that spine surgery was associated with even more favorable PFS, indicating no significant tumor-promoting effect of surgery in our MSCC cases.
One main limitation of our study is that in clinical practice, besides mBs, additional factors influence treatment decision whether decompressive surgery is indicated in acute MSCC or not. These factors may be measurable, such as burden of disease, poor performance status, severe comorbidities (e.g., renal/lung/cardiac function, dementia, anticoagulation therapy), and inoperability of a lesion, or unmeasurable, such as “clinical gestalt.” As with all retrospective studies, also, our analysis may have been affected by an omission of these measured or unmeasured variables, which may have led to an over- or underestimation of the “effect” of surgery on OS and neurologic outcomes. This, in addition to the single center design of this study limits generalizability of our results. Due to the retrospective design of this study, we could solely display Frankel scale as functional postoperative performance status measurement. Since recommended radiation therapy was frequently performed in external centers, we could not record a complete retrospective follow-up of patients receiving radiotherapy in their remaining lifetime.
Additional studies need to be done on quality of survival rather than just survival.
Conclusion
Our results suggest that the beneficial effect of decompressive surgery in patients with MSCC is not exclusively limited to neurological symptoms, as it is also associated with more favorable OS within a propensity score analysis. Notably, we observed that selected cases with a predicted poor prognosis according to the mBs might also benefit from surgery, and these patients can be delineated based on four clinical variables. Furthermore, no convincing evidence was found that surgical intervention in MSCC impairs oncologic outcomes in terms of PFS. In summary, these results support a more liberal threshold toward a surgical approach in MSCC. Further prospective studies with additional focus on quality of life should be conducted to confirm this approach.
References
Barzilai O, Laufer I, Yamada Y, Higginson DS, Schmitt AM, Lis E, Bilsky MH (2017) Integrating evidence-based medicine for treatment of spinal metastases into a decision framework: neurologic, oncologic, mechanicals stability, and systemic disease. J Clin Oncol 35:2419–2427
Meyer HS, Wagner A, Raufer A, Joerger AK, Gempt J, Meyer B (2022) Surgery in Acute Metastatic Spinal Cord Compression: Timing and Functional Outcome. Cancers (Basel) 14:2249
Dea N, Versteeg AL, Sahgal A, Verlaan JJ, Charest-Morin R, Rhines LD, Sciubba DM, Schuster JM, Weber MH, Lazary A et al (2020) Metastatic spine disease: should patients with short life expectancy be denied surgical care? An international retrospective cohort study. Neurosurgery 87:303–311
Dardic M, Wibmer C, Berghold A, Stadlmueller L, Froehlich EV, Leithner A (2015) Evaluation of prognostic scoring systems for spinal metastases in 196 patients treated during 2005–2010. Eur Spine J 24:2133–2141
Hibberd CS, Quan GMY (2017) Accuracy of preoperative scoring systems for the prognostication and treatment of patients with spinal metastases. Int Sch Res Notices 2017:1320684
Leithner A, Radl R, Gruber G, Hochegger M, Leithner K, Welkerling H, Rehak P, Windhager R (2008) Predictive value of seven preoperative prognostic scoring systems for spinal metastases. Eur Spine J 17:1488–1495
Klimo P Jr, Thompson CJ, Kestle JR, Schmidt MH (2005) A meta-analysis of surgery versus conventional radiotherapy for the treatment of metastatic spinal epidural disease. Neuro Oncol 7:64–76
Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, Mohiuddin M, Young B (2005) Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 366:643–648
Verlaan JJ, Choi D, Versteeg A, Albert T, Arts M, Balabaud L, Bunger C, Buchowski JM, Chung CK, Coppes MH et al (2016) Characteristics of patients who survived < 3 months or > 2 years after surgery for spinal metastases: can we avoid inappropriate patient selection? J Clin Oncol 34:3054–3061
Austin PC (2014) The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med 33:1242–1258
Maisel F, Smolle MA, Mollnar S, Riedl JM, Barth DA, Seles M, Terbuch A, Rossmann CH, Eisner F, Mannweiler S et al (2022) Benefit of metastasectomy in renal cell carcinoma: a propensity score analysis. Clin Genitourin Cancer 20:344–353
Tohme S, Simmons RL, Tsung A (2017) Surgery for Cancer: A Trigger for Metastases. Cancer Res 77:1548–1552
Nauffal D, Ballester M, Reyes RL, Jimenez D, Otero R, Quintavalla R, Monreal M, Investigators R (2012) Influence of recent immobilization and recent surgery on mortality in patients with pulmonary embolism. J Thromb Haemost 10:1752–1760
Van Cutsem E, Cervantes A, Nordlinger B, Arnold D, Group EGW (2014) Metastatic colorectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 25(Suppl 3):iii1–iii9
Arhin ND, Shen C, Bailey CE, Matsuoka LK, Hawkins AT, Holowatyj AN, Ciombor KK, Hopkins MB, Geiger TM, Kam AE et al (2021) Surgical resection and survival outcomes in metastatic young adult colorectal cancer patients. Cancer Med 10:4269–4281
Smolle MA, Kogler A, Andreou D, Scheipl S, Bergovec M, Castellani C, Till H, Benesch M, Posch F, Szkandera J et al (2023) Prognostic impact of pulmonary metastasectomy in bone sarcoma patients: a retrospective Single-Centre Study. Cancers (Basel) 15:1773
Palma DA, Olson R, Harrow S, Gaede S, Louie AV, Haasbeek C, Mulroy L, Lock M, Rodrigues GB, Yaremko BP et al (2019) Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet 393:2051–2058
De Meue E, Smeijers S, Langmans C, Clement PM, Depreitere B (2022) Identifying new predictive factors for survival after surgery for spinal metastases: an exploratory in-depth retrospective analysis. Acta Clin Belg 77:606–615
Karhade AV, Fenn B, Groot OQ, Shah AA, Yen HK, Bilsky MH, Hu MH, Laufer I, Park DY, Sciubba DM et al (2022) Development and external validation of predictive algorithms for 6-week mortality in spinal metastasis using 4,304 patients from 5 institutions. Spine J. https://doi.org/10.1016/j.spinee.2022.07.089
Choi D, Fox Z, Albert T, Arts M, Balabaud L, Bunger C, Buchowski JM, Coppes MH, Depreitere B, Fehlings MG et al (2016) Rapid improvements in pain and quality of life are sustained after surgery for spinal metastases in a large prospective cohort. Br J Neurosurg 30:337–344
Ju DG, Zadnik PL, Groves ML, Hwang L, Kaloostian PE, Wolinksy JP, Witham TF, Bydon A, Gokaslan ZL, Sciubba DM (2013) Factors associated with improved outcomes following decompressive surgery for prostate cancer metastatic to the spine. Neurosurgery 73:657–666 (Discussion 666)
Tsuchiya Y, Sawada S, Yoshioka I, Ohashi Y, Matsuo M, Harimaya Y, Tsukada K, Saiki I (2003) Increased surgical stress promotes tumor metastasis. Surgery 133:547–555
Funding
Open access funding provided by Medical University of Graz.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests. No external source of funding was used in this study.
Ethical approval
This study was approved by the Institutional Ethical Review Board (Reference number: 30-252 ex 17/18) and performed in accordance with relevant guidelines and regulations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leitner, L., Bratschitsch, G., Kostwein, A. et al. More help than harm: surgery for metastatic spinal cord compression is associated with more favorable overall survival within a propensity score analysis. Eur Spine J 32, 2468–2478 (2023). https://doi.org/10.1007/s00586-023-07755-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07755-9