Abstract
Purpose
There is no data that shows if it is possible to determine if a curve is structural or non-structural or to assess flexibility of an adolescent idiopathic scoliosis (AIS) by magnetic resonance imaging (MRI) instead of bending radiographs (BR). We investigated if the results of BR may be compared to those of MRI.
Methods
We retrospectively analyzed prospectively collected data of patients with AIS in whom a selective spinal fusion was performed and in whom a MRI, BR and full-spine X-rays were obtained preoperatively. We measured the Cobb angles of the main and of the minor curve in full-spine X-ray (FSR), BR and MRI and analyzed the degree of the intervertebral disk degeneration in the MRI.
Results
After applying inclusion and exclusion criteria, 25 patients were included. We found a significant correlation (p < 0.05, Corr Coeff = 0.41) between the Cobb angle of the main curve in FSR and the Cobb angle of the main curve in the MRI and between the Cobb angle of the minor curve in FSR and the Cobb angle of the minor curve in the MRI (p < 0.001, Corr Coeff = 0.04). All patients with a minor curve of less than 25° in the BR had a Cobb angle of less than 30° in the MRI.
Conclusion
Spinal curves showed a significant correlation between bending radiographs and recumbent images (MRI). In our group of patients, a Cobb angle of the minor curve of less than 30° in the MRI indicated that this minor curve was non-structural according to the classification of Lenke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is a three-dimensional deformity of the spine. AIS has an incidence of 5% [1]. The degree of the deformity can be graded by the Cobb angle. Depending on the degree of the deformity, conservative or operative therapy is recommended [2]. A common technique for operative therapy of AIS is the selective spinal fusion. To perform selective spinal fusion, a prior discrimination of structural and non-structural curves of the total deformity according to the Lenke classification [3, 5] is important. Furthermore, the appropriate lowest instrumented vertebra (LIV) must be determined. [3, 4]. Bending radiographs (BR) of the spine are necessary to classify a deformity according to the Lenke classification. Spinal curves, which can be corrected to less than 25° in a bending radiograph, are classified as “non-structural” [5]. A further information that is obtained by BR is the possible potential for correction of the deformity by surgery [6, 7]. Different types of bending radiographs are described in literature: push-prone radiographs (PPR) [8], fulcrum bending radiographs [6], supine side bending radiographs [9] and radiographs with traction under general anesthesia [10]. A disadvantage of all types of BR is that they lead to an additional amount of exposure to radiation for the patient and some of them, like the push-prone radiographs, lead to an additional amount of radiation to the medical personal, too.
Numerous radiographs are usually performed during conservative or operative treatment of AIS. The cumulative effective dose of standard radiographs, performed for diagnosis and follow-up of scoliosis, correlates with incidence of breast cancer in scoliosis patients and with an increasing incidence for infertility [11, 12]. Therefore, it seems to be relevant to reevaluate the need of each radiograph performed during the treatment of AIS. According to this, we wanted to analyze if the flexibility of the spine can be evaluated without BR. Some surgeons perform a MRI if AIS is treated by surgery. Since this imaging technique is performed recumbent, the difference between Cobb angles in standing or recumbent position could be evaluated to analyze flexibility.
Previous investigations of our study group showed that Cobb angels of push-prone bending radiographs (PPR) show a significant correlation with Cobb angles in preoperative CT scan (CTS) and that a Cobb angle of a minor curve in a CTS of less than 35° determined a non-structural curve. [13]
To our knowledge, there is no data that shows if it is possible to determine if a curve is structural or non-structural by MRI. If this would be possible, preoperative MRI could theoretically replace BR. This could lead to a reduction of the exposure to radiation for the patient and for the medical personnel.
We conducted this investigation to analyze if MRI instead of BR could provide information on flexibility and type of curves in patients with AIS.
Patients and methods
We retrospectively analyzed prospectively collected data in a single-center study. In our clinical documentation system, we identified consecutive patients in whom an operative treatment for AIS was performed from 04/2017 to 04/2021 by diagnostic code. We included patients who were treated by a selective spinal fusion with PIN and who had a full-spine X-ray in posterior–anterior view (FSR), BR and MRI in the preoperative planning. In our institution, PPR are performed as BR. We excluded patients with incomplete sets of radiological data. We recorded demographical data like sex and age, and recorded the Lenke classification of the included patients.
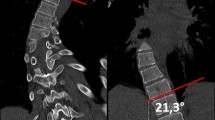
The radiographs were analyzed by the IDS 7-PACS®-System (Sectra, Linköping, Sweden). In all available radiographs (FSR, PPR and the MRI), the Cobb angle of the main curve and of the upper and lower minor curve was measured. Furthermore, we measured the segmental Cobb angle of the intervertebral space under the lowest vertebra of the main curve (ISE) and the angle of the first flexible intervertebral space below the main curve (FFI). Measurement of Cobb angle in the MRI is demonstrated in (Fig. 1). Measurement was performed in coronal reconstructions of the MRI. Due to the 3D character of the spinal deformity in patients with scoliosis in the performed MRI scans, there were no single slides, i.e., no single images, which showed the entire curve of a patient. Thus, to gain more comparability between the patients, we decided to perform the measurement of the Cobb angle in the way we presented in Fig. 1. End vertebras were identified in the FSR. The angle between the superior endplate of the cranial end vertebra and the horizontal plane and the angle between the inferior endplate of the caudal end vertebra and the horizontal plane were measured. These two angles were added to obtain the Cobb angle of the according curve (Fig. 1).
Measurement of Cobb Angle in a MRI. A Coronal reconstruction of a MRI scan of the spine (T2 weighed). The superior endplate of the cranial end vertebra of the according curve is depicted. End vertebra were identified in the FSR. The angle between the superior endplate of the cranial end vertebra and the horizontal plane was 33.9°. B Coronal reconstruction of a MRI scan (T2 weighed) of the spine. The inferior endplate of the caudal end vertebra of the according curve is depicted. End vertebra were identified in the FSR. The angle between the inferior endplate of the caudal end vertebra and the horizontal plane was measured with 29.4°. Summation of these two angles (33.9 in 1A + 29.4 in 1B) determines a Cobb angle of 63.3 degree for this thoracic curve
Identification and measurement of the ISE and the FFI
The lowest intervertebral space of the main curve was defined as the intervertebral space between the caudal end vertebra of the main curve and the cranial end vertebra of the caudal minor curve in the FSR. We measured the angle between the inferior endplate of the cranial vertebra and the superior endplate of the caudal vertebra in the FSR, PPR and the MRI.
The FFI below the main curve was defined as the intervertebral space caudal of the main curve of the deformity that opened to different sides in the PPR (Fig. 2). We measured the angle between the inferior endplate of the cranial vertebra of this intervertebral space and the superior endplate of the caudal vertebra in the FSR, PPR and the MRI.
Identification of the FFI in the PPR—The FFI below the main curve was defined as the intervertebral space caudal of the main curve of the deformity that opened to different sides in the PPR. A Part of a PPR of the spine with bending to the left. Zoom is on the caudal end of the main curve. End vertebra were identified in the FSR. Marked is the first intervertebral space below the main curve of the deformity that opens to the concave side with regard to the analyzed curve. The angle between the inferior endplate of the cranial vertebra of this intervertebral space and the superior endplate of the caudal vertebra is measured. B Part of a PPR of the spine with bending to the right. Zoom is on the caudal end of the main curve. End vertebra were identified in the FSR. Marked is the first intervertebral space below the main curve of the deformity that opens to the other side than the same intervertebral space in A. The angle between the inferior endplate of the cranial vertebra of this intervertebral space and the superior endplate of the caudal vertebra is measured
Statistical analysis was performed by SPSS® 25 (IBM, Armonk, USA). Descriptive data is given as mean and standard error of mean (SEM). We tested all continuous variables for normal distribution by Kolmogorov–Smirnov tests. All variables showed normal distribution. Thus, we assessed correlation by Pearson’s correlation index.
For the analysis of the PPR, we always analyzed the angles of the PPR to the concavity of the main curve: In curves with a right convexity, we analyzed the according PPR to the left and in curves with a left convexity, we analyzed the according PPR to the right.
This study was approved by the local ethics committee (Register number 2020-913) and was conducted according to the revised Declaration of Helsinki.
Results
We identified 35 consecutive patients who were treated operatively for AIS in our institution between 04/2017 and 04/2021 and received a preoperative MRI by diagnostic code. After application of the inclusion and exclusion criteria, we enrolled 25 patients to our investigation. Sixteen patients were female (64%), and nine patients were male (36%). The average age at the date the radiographs were performed was 15.48 (3.30) years. According to the Lenke classification, 18 patients had a type 1 curve, three patients a type 5 curve, two patients type 2 and two patients a type 6 curve.
In Table 1, we present data of the Cobb angle of the main and of the minor curve in the FSR, PPR and the MRI.
In a subgroup analysis of all patients with a minor curve of less than 40° in the FSR (more than 40° characterizes a structural curve), we analyzed the Cobb angles of the minor curve in the PPR and MRI. If the minor curve was less than 30° in the MRI, it was also less than 25° in the PPR in 100% of these patients.
Tables 1, 2, 3 and 4 show values of Cobb angles of the FSR, PPR and the MRI.
There was a significant correlation (p < 0.05, Corr Coeff = 0.41) between the Cobb angle of the main curve in FSR and the Cobb angle of the main curve in the MRI.
Furthermore, we found significant correlations between the minor curves in the different types of radiographs. There was a significant correlation (p < 0.001, Corr Coeff = 0.04) between the Cobb angle of the minor curve in FSR and the Cobb angle of the minor curve in the MRI.
The difference between the Cobb angle of the main curve in the FSR and in the PPR shows a significant correlation (p < 0.05, Corr Coeff = 0.41) to the difference between the Cobb angle of the main curve in the FSR and the Cobb angle of the main curve in the MRI.
The difference between the Cobb angle of the minor curve in the FSR and in the PPR shows a significant correlation (p < 0.001, Corr Coeff = 0.9) to the difference between the Cobb angle of the minor curve in the FSR and the Cobb angle of the minor curve in the MRI. There was a significant correlation (p < 0.05, Corr Coeff = 0.47) between the difference of the Cobb angle of the ISE in the FSR and in the PPR and the difference of the Cobb angle of the ISE in the FSR and in the MRI.
According to the Cobb angles of the FFI, there were no significant correlations between the different images.
Discussion
In this study, we found a significant correlation (p < 0.05) for all analyzed Cobb angles between BR and MRI.
Brink et al. reported a significant correlation of the morphology of the scoliotic spine in all three planes between standard upright X-ray, MRI and CT scan [14]. Keenan et al. [15] showed 2014 that there is a statistically significant relationship between the Cobb angle in supine and upright position for the major curve. However, minor curves were not analyzed, especially not with regard to the flexibility of the curve. There is presently no data that compares the assessment of flexibility of the minor curve in BR versus MRI scans.
According to the data of this study, it does seem likely that Cobb angles of the main and the minor curves in MRI may provide similar information as a PPB.
Furthermore, our data show that it is possible to determine if a minor curve is structural or non-structural by analyzing the Cobb angle in the MRI. Every patient with a Cobb angle of the minor curve of less than 40° in the FSR and a Cobb angle of the minor curve less than 25° in the PPB showed a Cobb angle of the minor curve in the MRI of less than 30°. These curves are, according to the Lenke classification, non-structural and do not have to be included in the selective spinal fusion [3]. According to this data, in our group of patients a Cobb angle of < 35° in the recumbent MRI scan determined a non-structural curve. This is comparable to the results of a former investigation of our group where we showed that a Cobb angle of the minor curve of less than 35° in the CTS indicated that this minor curve was non-structural [13].
These results may indicate that neither PPR’s nor CTS are necessary to determine if a curve is structural or non-structural. This may provide a means for the reduction of the dose of radiation for scoliosis patients and for the medical personal. However, it also has to be taken into account that the costs for performing an MRI instead of plane radiographs are approximately three times higher. Furthermore, it has to be mentioned that MRI’s are not equally available in all regions and the waiting time for obtaining an MRI as well as the technique itself takes longer than BR. But since we discuss a technique for an elective surgery without any emergency character, these above-mentioned points should be, in our opinion, considered as minor consequence compared with the fact that exposure to radiation might be reduced.
If some patients might have contraindications against an MRI (e.g., anxiety or a pacemaker), it could be necessary to fall back to the technique with plain radiographs.
Furthermore, we saw that there are significant correlations between the Cobb angles of the ISE in the analyzed radiographs. However, statistical power was rather low, especially in the correlations between the PPR and the MRI. Thus, we presently cannot apply the MRI as a tool to analyze the flexibility of the ISE.
A limitation of our investigation is that we performed a retrospective data analysis. Furthermore, we only analyzed the correlation between the PPR and the MRI and did not investigate other types of BR. However, former analyses showed that PPR are appropriate to determine the effects of a correction of the main curve on the curves above and below the level of fusion by better predicting the translational correction of the lowest instrumented vertebra and the rotation of the lowest instrumented vertebra than other types of BR [16]. The available data show that none of the common types of BR is superior to the others [6, 8, 10, 15, 17, 18].
Conclusion
Cobb angels of push-prone bending radiographs show a significant correlation with Cobb angles in MRI scans. In our group of patients, a Cobb angle of a minor curve in a recumbent MRI scan of less than 30° determined a non-structural curve in 100% of all cases.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available due data protection but are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Abbreviations
- AIS:
-
Adolescent idiopathic scoliosis
- LIV:
-
Lowest instrumented vertebra
- BR:
-
Bending radiographs
- CTS:
-
Preoperative CT scan
- MRI:
-
Magnetic resonance imaging
- PPR:
-
Push-prone radiographs
- IVD:
-
Intervertebral disk
- PIN:
-
Pedicle screw insertion guided by navigation
- FSR:
-
Full-spine X-ray in posterior–anterior view
- ISE:
-
Intervertebral space below the end vertebra of the main curve
- FFI:
-
Frist flexible intervertebral space below the main curve
- SEM:
-
Standard error of mean
- Corr Coeff:
-
Correlation coefficient
- p :
-
Level of significance
References
Konieczny MR, Senyurt H, Krauspe R (2013) Epidemiology of adolescent idiopathic scoliosis. J Child Orthop 7(1):3–9. https://doi.org/10.1007/s11832-012-0457-4
Trobisch P, Suess O, Schwab F (2010) Idiopathic scoliosis. Dtsch Arzteblatt Int 107(49):875–884. https://doi.org/10.3238/arztebl.2010.0875
Lenke LG, Betz RR, Haher TR, Lapp MA, Merola AA, Harms J, Shufflebarger HL (2001) Multisurgeon assessment of surgical decision-making in adolescent idiopathic scoliosis: curve classification, operative approach, and fusion levels. Spine 26(21):2347–2353. https://doi.org/10.1097/00007632-200111010-00011
King HA, Moe JH, Bradford DS, Winter RB (1983) The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Jt Surg 65(9):1302–1313
Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Jt Surg Am 83(8):1169–1181
Cheung KM, Luk KD (1997) Prediction of correction of scoliosis with use of the fulcrum bending radiograph. J Bone Jt Surg 79(8):1144–1150. https://doi.org/10.2106/00004623-199708000-00005
Kleinman RG, Csongradi JJ, Rinksy LA, Bleck EE (1982) The radiographic assessment of spinal flexibility in scoliosis: a study of the efficacy of the prone push film. Clin Orthop Relat Res 162:47–53
Rodrigues LM, Ueno FH, Gotfryd AO, Mattar T, Fujiki EN, Milani C (2014) Comparison between different radiographic methods for evaluating the flexibility of scoliosis curves. Acta Ortoped Brasil 22(2):78–81. https://doi.org/10.1590/1413-78522014220200844
Aronsson DD, Stokes IA, Ronchetti PJ, Richards BS (1996) Surgical correction of vertebral axial rotation in adolescent idiopathic scoliosis: prediction by lateral bending films. J Spinal Disord 9(3):214–219
Vaughan JJ, Winter RB, Lonstein JE (1996) Comparison of the use of supine bending and traction radiographs in the selection of the fusion area in adolescent idiopathic scoliosis. Spine 21(21):2469–2473. https://doi.org/10.1097/00007632-199611010-00012
Doody MM, Lonstein JE, Stovall M, Hacker DG, Luckyanov N, Land CE (2000) Breast cancer mortality after diagnostic radiography: findings from the U.S. Scoliosis Cohort Study. Spine 25(16):2052–2063. https://doi.org/10.1097/00007632-200008150-00009
Simony A, Christensen SB, Jensen KE, Carreon LY, Andersen MO (2015) Incidence of cancer and infertility, in patients treated for adolescent idiopathic scoliosis 25 years prior. Eur Spine J 24(S6):S740. https://doi.org/10.1007/s00586-015-4130-8
Prost M, Windolf J, Konieczny MR (2021) May bending radiographs be replaced by recumbent CT scans in patients with adolescent idiopathic scoliosis? Eur Spine J 30(12):3490–3497. https://doi.org/10.1007/s00586-021-06945-7
Brink RC, Colo D, Schlösser T, Vincken KL, van Stralen M, Hui S, Shi L, Chu W, Cheng J, Castelein RM (2017) Upright, prone, and supine spinal morphology and alignment in adolescent idiopathic scoliosis. Scoliosis Spinal Disord 12:6. https://doi.org/10.1186/s13013-017-0111-5
Keenan BE, Izatt MT, Askin GN, Labrom RD, Pearcy MJ, Adam CJ (2014) Supine to standing Cobb angle change in idiopathic scoliosis: the effect of endplate pre-selection. Scoliosis 9:16. https://doi.org/10.1186/1748-7161-9-16
Vedantam R, Lenke LG, Bridwell KH, Linville DL (2000) Comparison of push-prone and lateral-bending radiographs for predicting postoperative coronal alignment in thoracolumbar and lumbar scoliotic curves. Spine 25(1):76–81. https://doi.org/10.1097/00007632-200001010-00014
Klepps SJ, Lenke LG, Bridwell KH, Bassett GS, Whorton J (2001) Prospective comparison of flexibility radiographs in adolescent idiopathic scoliosis. Spine 26(5):E74–E79. https://doi.org/10.1097/00007632-200103010-00002
Pruijs JE, Hageman MA, Keessen W, van der Meer R, van Wieringen JC (1994) Variation in Cobb angle measurements in scoliosis. Skeletal Radiol 23(7):517–520. https://doi.org/10.1007/BF00223081
Funding
Open Access funding enabled and organized by Projekt DEAL. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Contributions
MP was involved in conception and design, administrative support, collection and assembly of data, provision of study materials or patients, data analysis and interpretation, manuscript writing, final approval of manuscript. MR helped in administrative support, collection and assembly of data, provision of study materials or patients, data analysis and interpretation, manuscript writing, final approval of manuscript. RT contributed to administrative support, collection and assembly of data, provision of study materials or patients, data analysis and interpretation, manuscript writing, final approval of manuscript. JW was involved in administrative support, provision of study materials or patients, manuscript writing, final approval of manuscript. MRK helped in administrative support, collection and assembly of data, provision of study materials or patients, data analysis and interpretation, manuscript writing, final approval of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
MP none. MER none. RT none. JW none. MRK reports personal fees from Globus Medical and Depuy Synthes, outside the submitted work. The other authors declare no conflict of interest relevant to this work.
Ethical approval
This study was approved by the local ethics committee (Register number 2020-913) and was conducted according to the revised declaration of Helsinki.
Consent to participate
Not applicable because of the retrospective design of the investigation.
Consent for publication
Not applicable because of the retrospective design of the investigation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Prost, M., Röckner, M.E., Taday, R. et al. May bending radiographs be replaced by magnetic resonance imaging in patients with adolescent idiopathic scoliosis?. Eur Spine J 32, 1771–1776 (2023). https://doi.org/10.1007/s00586-023-07659-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07659-8