Abstract
Purpose
To evaluate the association between global spinal malalignment and rapid progression of hip arthrosis.
Methods
This was a retrospective, case–control study including 90 patients, contributing 90 hips, who underwent hemi- or total hip arthroplasty at our institution. For analysis, hips were classified into a rapid progression group, defined as ≥ 2 mm destruction of the femoral head or loss of the hip joint space within a 12-month period (n = 30), and a non-rapid progression group, defined by no observable hip disease progression over a period more than 12 months (n = 60). Logistic regression analysis identified factors that predicted rapid progression, with a receiver operating characteristic curve analysis used to confirm factors.
Results
Significant between-group differences were identified for the following parameters: pelvic tilt (P = 0.002, PT), sagittal vertical axis (P = 0.002, SVA), and T1 pelvic angle (P < 0.001, TPA). On multiple logistic regression, PT (P = 0.002), SVA (P = 0.002), and TPA (P < 0.001) were predictive of a rapid progression on hip arthrosis, with the area under the curve being greater for TPA than PT (P = 0.035).
Conclusion
Global spinal alignment is associated with rapid progression of hip arthrosis. TPA could assist in identifying patients at risk for rapid progression of hip arthrosis, allowing for time management.





Similar content being viewed by others
References
Postel M, Kerboull M (1970) Total prosthetic replacement in rapidly destructive arthrosis of the hip joint. Clin Orthop Relat Res 72:138–144
Della Torre P, Picuti G, Di Filippo P (1987) Rapidly progressive osteoarthritis of the hip. Ital J Orthop Traumatol 13(2):187–200
Carli AB, Akarsu S, Tekin L, Kiralp MZ (2013) Rapidly destructive arthrosis of the hip joint. Chin Med J (Engl) 126(16):3195
Komiya S, Inoue A, Sasaguri Y, Minamitani K, Morimatsu M (1992) Rapidly destructive arthropathy of the hip. Studies on bone resorptive factors in joint fluid with a theory of pathogenesis. Clin Orthop Relat Res (284):273–282.
Ogawa K, Mawatari M, Komine M, Shigematsu M, Kitajima M, Kukita A, Hotokebuchi T (2007) Mature and activated osteoclasts exist in the synovium of rapidly destructive coxarthrosis. J Bone Miner Metab 25(6):354–360. https://doi.org/10.1007/s00774-007-0761-0
Yasuda T, Matsunaga K, Hashimura T, Tsukamoto Y, Sueyoshi T, Ota S, Fujita S, Onishi E (2020) Bone turnover markers in the early stage of rapidly progressive osteoarthritis of the hip. Eur J Rheumatol 8(2):57–61. https://doi.org/10.5152/eurjrheum.2020.20046
Masuhara K, Nakai T, Yamaguchi K, Yamasaki S, Sasaguri Y (2002) Significant increases in serum and plasma concentrations of matrix metalloproteinases 3 and 9 in patients with rapidly destructive osteoarthritis of the hip. Arthritis Rheum 46(10):2625–2631. https://doi.org/10.1002/art.10547
Yamamoto T, Bullough PG (2000) The role of subchondral insufficiency fracture in rapid destruction of the hip joint: a preliminary report. Arthritis Rheum 43(11):2423–2427. https://doi.org/10.1002/1529-0131(200011)43:11%3c2423::AID-ANR8%3e3.0.CO;2-Z
Kwon HM, Yang IH, Park KK, Cho BW, Kam JH, Kong Y, Yang JH, Lee WS (2020) High Pelvic Incidence Is Associated with Disease Progression in Nontraumatic Osteonecrosis of the Femoral Head. Clin Orthop Relat Res 478(8):1870–1876. https://doi.org/10.1097/CORR.0000000000001155
Kawai T, Shimizu T, Goto K, Kuroda Y, Okuzu Y, Fujibayashi S, Matsuda S (2021) Number of Levels of Spinal Fusion Associated with the Rate of Joint-Space Narrowing in the Hip. J Bone Joint Surg Am 103(11):953–960. https://doi.org/10.2106/JBJS.20.01578
Morimoto T, Kitajima M, Tsukamoto M, Yoshihara T, Sonohata M, Mawatari M (2018) Sagittal spino-pelvic alignment in rapidly destructive coxarthrosis. Eur Spine J 27(2):475–481. https://doi.org/10.1007/s00586-017-5282-5
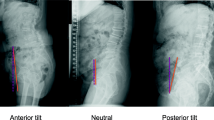
Morvan G, Mathieu P, Vuillemin V, Guerini H, Bossard P, Zeitoun F, Wybier M (2011) Standardized way for imaging of the sagittal spinal balance. Eur Spine J 20(Suppl 5):602–608. https://doi.org/10.1007/s00586-011-1927-y
Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP (2006) Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976) 31(25):E959–E967. https://doi.org/10.1097/01.brs.0000248126.96737.0f.
Protopsaltis T, Schwab F, Bronsard N, Smith JS, Klineberg E, Mundis G, Ryan DJ, Hostin R, Hart R, Burton D, Ames C, Shaffrey C, Bess S, Errico T, Lafage V; International Spine Study Group (2014) TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. 96(19):1631–1640. https://doi.org/10.2106/JBJS.M.01459.
Uemura K, Takao M, Otake Y, Koyama K, Yokota F, Hamada H, Sakai T, Sato Y, Sugano N (2017) Change in pelvic sagittal inclination from supine to standing position before hip arthroplasty. J Arthroplasty 32(8):2568–2573. https://doi.org/10.1016/j.arth.2017.03.015
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 37(12):1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2.
Homma Y, Baba T, Sumiyoshi N, Ochi H, Kobayashi H, Matsumoto M, Yuasa T, Kaneko K (2014) Rapid hip osteoarthritis development in a patient with anterior acetabular cyst with sagittal alignment change. Case Rep Orthop 2014:523426. https://doi.org/10.1155/2014/523426.
Baba T, Homma Y, Ochi H, Ozaki Y, Matsumoto M, Shitoto K, Kaneko K (2016) Total hip arthroplasty using a Kerboull-type plate for rapidly destructive coxarthrosis: comparison with uncemented acetabular component. Eur J Orthop Surg Traumatol 26(2):189–194. https://doi.org/10.1007/s00590-015-1738-7
Yoshimoto H, Sato S, Masuda T, Kanno T, Shundo M, Hyakumachi T, Yanagibashi Y (2005) Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976) 30(14):1650–1657. https://doi.org/10.1097/01.brs.0000169446.69758.fa.
Garbossa D, Pejrona M, Damilano M, Sansone V, Ducati A, Berjano P (2014) Pelvic parameters and global spine balance for spine degenerative disease: the importance of containing for the well being of content. Eur Spine J 23(Suppl 6):616–627. https://doi.org/10.1007/s00586-014-3558-6
Miura T, Miyakoshi N, Saito K, Kijima H, Iida J, Hatakeyama K, Suzuki K, Komatsu A, Iwami T, Matsunaga T, Shimada Y (2021) Association between global sagittal malalignment and increasing hip joint contact force, analyzed by a novel musculoskeletal modeling system. PLoS One 16(10):e0259049. https://doi.org/10.1371/journal.pone.0259049.
Kitamura K, Fujii M, Utsunomiya T, Iwamoto M, Ikemura S, Hamai S, Motomura G, Todo M, Nakashima Y (2020) Effect of sagittal pelvic tilt on joint stress distribution in hip dysplasia: a finite element analysis. Clin Biomech (Bristol, Avon) 74:34–41. https://doi.org/10.1016/j.clinbiomech.2020.02.011
Uehara M, Takahashi J, Ikegami S, Tokida R, Nishimura H, Sakai N, Kato H (2019) Sagittal spinal alignment deviation in the general elderly population: a Japanese cohort survey randomly sampled from a basic resident registry. Spine J 19(2):349–356. https://doi.org/10.1016/j.spinee.2018.06.346
Lazennec JY, Brusson A, Rousseau MA (2011) Hip-spine relations and sagittal balance clinical consequences. Eur Spine J 20(Suppl 5):686–698. https://doi.org/10.1007/s00586-011-1937-9
Rivière C, Lazennec JY, Van Der Straeten C, Auvinet E, Cobb J, Muirhead-Allwood S (2017) The influence of spine-hip relations on total hip replacement: a systematic review. Orthop Traumatol Surg Res 103(4):559–568. https://doi.org/10.1016/j.otsr.2017.02.014
Acknowledgements
We would like to thank Takashi Fujishiro, MD, PhD, for helpful discussions and comments on the manuscript, and Editage (www.editage.com) for English language editing.
Funding
Role of funding agency: This study was supported by the Grants-in-Aid for Scientific Research of Japan Society KAKENHI for the Promotion of Science, Grant Number 21K09239.
Author information
Authors and Affiliations
Contributions
KN, YO, HW, and SO designed the study. KN, JM, and TI analyzed the data. KN, YO, WH, JM, TI, SO, and MN wrote the manuscript. YO, HW, and MN supervised the study. KN, YO, and MN ensured the accuracy of the data and analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nakamura, K., Okamoto, Y., Wakama, H. et al. T1 pelvic angle is associated with rapid progression of hip arthrosis. Eur Spine J 32, 1463–1470 (2023). https://doi.org/10.1007/s00586-023-07580-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07580-0