Abstract
Purpose
This study aimed to establish biomarkers to predict the progression of ossification by examining ossification volume and bone metabolism dynamics in patients with ossification of the posterior longitudinal ligament (OPLL).
Methods
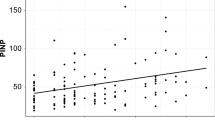
We assessed OPLL progression using computed tomography-based three-dimensional (3D) image analysis and examined bone metabolism dynamics in 107 patients with OPLL (men, 72; women, 35; mean age, 63.6 years). The volume of OPLL was calculated twice during the follow-up period, and OPLL progression was evaluated by the annual rate of ossification increase. Bone metabolism dynamics were assessed by routine blood tests and analysis of various serum biomarkers (including 25-hydroxyvitamin D, intact parathyroid hormone, fibroblast growth factor 23, intact N-terminal propeptide of type 1, tartrate-resistant acid phosphatase isoform 5b, sclerostin, and Dickkopf-1) and bone mineral density (BMD). Patients were classified into the progression (P) or non-progression (NP) group according to the annual rate of increase in previous 3D image analyses, and associated factors between these groups were compared.
Results
The P and NP groups consisted of 29 patients (23 men and 6 women) and 78 patients (49 men and 29 women), respectively. Univariate analysis revealed significant differences in terms of age, body mass index, serum phosphorus, serum sclerostin, and BMD. In multivariate analysis, age, serum phosphorus, and serum sclerostin were identified as independent factors associated with OPLL progression.
Conclusion
Younger age, hypophosphatemia, and high serum sclerostin are risk factors for OPLL progression. Serum phosphorus and sclerostin could serve as important biomarkers for predicting ossification progression.


Similar content being viewed by others
Data availability
The study data and details of materials used may be made available upon reasonable request by sending an e-mail to the first author.
References
Fragen KM, Cox JB, Hoh DJ (2012) Does ossification of the posterior longitudinal ligament progress after laminoplasty? Radiographic and clinical evidence of ossification of the posterior longitudinal ligament lesion growth and the risk factors for late neurologic deterioration. J Neurosurg Spine 17:512–524. https://doi.org/10.3171/2012.9.SPINE12548
Iwasaki M, Kawaguchi Y, Kimura T, Yonenobu K (2002) Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: more than 10 years follow up. J Neurosurg 96:180–189. https://doi.org/10.3171/spi.2002.96.2.0180
Hori T, Kawaguchi Y, Kimura T (2007) How does the ossification area of the posterior longitudinal ligament thicken following cervical laminoplasty. Spine (Phila Pa 1976) 32:551–556
Kawaguchi Y, Kanamori M, Ishihara H, Nakamura H, Sugimori K, Tsuji H, Kimura T (2001) Progression of ossification of the posterior longitudinal ligament following en bloc cervical laminoplasty. J Bone Joint Surg Am 83:1798–1802. https://doi.org/10.2106/00004623-200112000-00005
Takatsu T, Ishida Y, Suzuki K, Inoue H (1998) Radiological study of cervical ossification of the posterior longitudinal ligament. J Spinal Disord 12:271–273
Katsumi K, Izumi T, Ito T, Hirano T, Watanabe K, Ohashi M (2016) Posterior instrumented fusion suppresses the progression of ossification of the posterior longitudinal ligament: a comparison of laminoplasty with and without instrumented fusion by 3-dimensional analysis. Eur Spine J 25:1634–1640. https://doi.org/10.1007/s00586-015-4328-9
Katsumi K, Watanabe K, Izumi T, Hirano T, Ohashi M, Mizouchi T, Ito T, Endo N (2016) Natural history of the ossification of cervical posterior longitudinal ligament: a three-dimensional analysis. Int Orthop 42:835–842. https://doi.org/10.1007/s00264-017-3667-
Fujimori T, Iwasaki M, Nagamoto Y, Ishii T, Sakaura H, Kashii M, Yoshikawa H, Sugamoto K (2012) Three-dimensional measurement of growth of ossification of the posterior longitudinal ligament. J Neurosurg Spine 16:289–895. https://doi.org/10.3171/2011.11.SPINE11502
Lee DH, Cho JH, Kim NH, Kim S, Choi J, Hwang CJ, Lee CS (2018) Radiological risk factors for progression of ossification of posterior longitudinal ligament following laminoplasty. Spine J 18:1116–1121. https://doi.org/10.1016/j.spinee.2017.10.069
Lee JJ, Shin DA, Yi S, Kim KN, Yoon DH, Shin HC, Ha Y (2018) Effect of posterior instrumented fusion on three-dimensional volumetric growth of cervical ossification of the posterior longitudinal ligament: a multiple regression analysis. Spine J 18:1779–1786. https://doi.org/10.1016/j.spine.2018.03.002
Yamauchi T, Taketomi E, Matsunaga S, Sakou T (1999) Bone mineral density in patients with ossification of the posterior longitudinal ligament in the cervical spine. J Bone Miner Metab 17:296–300. https://doi.org/10.1007/s007740050098
Shin J, Choi JY, Kim YW, Chang JS, Yoon S (2019) Quantification of risk factors for cervical ossification of the posterior longitudinal ligament in Korean populations: A nationwide population-based case-control study. Spine (Phila Pa 1976) 44:957–964. https://doi.org/10.1097/BRS.0000000000003027
Lee SH, Agashe MV, Suh SW, Yoon YC, Song SH, Yang JH, Lee H, Song HR (2012) Paravertebral Ligament Ossification in Vitamin D-Resistant Rickets. Spine (Phila Pa 1976) 37:792–796. https://doi.org/10.1097/BRS.0b013e31824a3dc8
Kawaguchi Y, Kitajima I, Nakano M, Yasuda T, Seki S, Suzuki K, Yahara Y, Makino H, Ujihara Y, Ueno T, Kimura T (2019) Increase of the serum FGF-23 in ossification of the posterior longitudinal ligament. Global Spine J 9:492–498. https://doi.org/10.1177/2192568218801015
Horie S, Sawaji Y, Endo K, Suzuki H, Matsuoka Y, Nishimura H, Seki T, Yamamoto K (2018) Factors associated with bone metabolism in patients with cervical ossification of the posterior longitudinal ligament accompanied with diffuse idiopathic skeletal hyperostosis. SICOT J 4:7. https://doi.org/10.1051/sicotj/2017061
Kashii M, Matuso Y, Sugiura T, Fujimori T, Nagamoto Y, Makino T, Kaito T, Ebina K, Iwasaki M, Yoshikawa H (2016) Circulating sclerostin and dickkopf-1 levels in ossification of the posterior longitudinal ligament of the spine. J Bone Miner Metab 34:315–324. https://doi.org/10.1007/s00774-015-0671-5
Maeda K, Kobayashi Y, Koide M, Uehara S, Okamoto M, Ishihara A, Kayama T, Saito M, Marumo K (2019) The regulation of bone metabolism and disorders by wnt signaling. Int J Mol Sci 20:5525. https://doi.org/10.3390/ijms20225525
Tsuyama N (1981) The ossification of the posterior longitudinal ligament of the spine (OPLL). Nihon Seikeigeka Gakkai Zasshi 55:425–440
Kawaguchi Y, Nakano M, Yasuda T, Seki S, Hori T, Kimura T (2013) Ossification of the posterior longitudinal ligament in not only the cervical spine, but also other spinal regions: Analysis using multidetector computed tomography of the whole spine. Spine 38:E1477–E1482. https://doi.org/10.1097/BRS.0b013e3182a54f00
Hirai T, Yoshii T, Iwanami A et al (2016) Prevalence and distribution of ossified lesions in the whole spine of patients with cervical ossification of the posterior longitudinal ligament a multicenter study JOSL CT study. PLoS ONE 11:e0160117. https://doi.org/10.1371/journal.pone.0160117
Endo I, Fukumoto S, Ozono K, Namba N, Tanaka H, Inoue D, Minagawa M, Sugimoto T, Yamauchi M, Michigami T, Matsumoto T (2008) Clinical usefulness of measurement of fibroblast growth factor 23 (FGF23) in hypophosphatemic patients: proposal of diagnostic criteria using FGF23 measurement. Bone 42:1235–1239. https://doi.org/10.1016/j.bone.2008.02.014
Fukumoto S, Yamashita T (2007) FGF23 is a hormone-regulating phosphate metabolism–unique biological characteristics of FGF23. Bone 40:1190–1195. https://doi.org/10.1016/j.bone.2006.12.062
Matsunaga S, Nakamura K, Seichi A et al (2008) Radiographic predictors for the development of myelopathy in patients with ossification of the posterior longitudinal ligament: a multicenter cohort study. Spine 33:2648–2650. https://doi.org/10.1097/BRS.0b013e31817f988c
Modder UI, Hoey KA, Amin A, McCready LK, Achenbach SJ, Riggs BL, Melton LJ, Khosla S (2011) Relation of age, gender, and bone mass to circulating sclerostin levels in women and men. J Bone Miner Res 26:373–379. https://doi.org/10.1002/jbmr.217
Tanaka S, Matsumoto T (2021) Sclerostin: from bench to bedside. J Bone Miner Metab 39:332–340. https://doi.org/10.1007/s00774-020-01176-0
Acknowledgements
We greatly thank Nami Kira and Masanori Hirayama for their assistance in data collection.
Funding
This work was supported by JSPS KAKENHI Grant Number (JP18K16612) and by Health and Labor Science Research grants (201610008B).
Author information
Authors and Affiliations
Contributions
KK, WK, TH, and TI designed the study; KK, KW, TH, MO, TM, MS, HS, and YS collected the data; KK, KW, AY, TH, and MO analyzed and interpreted the data; KK, KW, AY, and TH wrote the initial draft of the manuscript; KK, and MT performed the statistical analyses. KK, KW, AY, TH, MO, TM, MS, HS, TI, YS, and HK participated in revising the manuscript. KW, AY, TH, and HK supervised the study. KK, KW, and HK acquired the funding. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
Written informed consent was obtained from each study participant before enrollment at each institution. The study protocol was approved by the ethics committee at each participating institution, i.e., Niigata Central Hospital: et2020-03, Niigata University Medical and Dental General Hospital: 2015–2525, and Uonuma Institute of Community Medicine, Niigata University Medical and Dental Hospital: 30–010.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Katsumi, K., Watanabe, K., Yamazaki, A. et al. Predictive biomarkers of ossification progression and bone metabolism dynamics in patients with cervical ossification of the posterior longitudinal ligament. Eur Spine J 32, 1282–1290 (2023). https://doi.org/10.1007/s00586-023-07565-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07565-z