Abstract
Purpose
The aim of this study was to assess safety and efficacy of vertebral body stenting (VBS) by analyzing (1) radiographic outcome, (2) clinical outcome, and (3) perioperative complications in patients with vertebral compression fractures treated with VBS at minimum 6-month follow-up.
Methods
In this retrospective cohort study, 78 patients (61 ± 14 [21–90] years; 67% female) who have received a vertebral body stent due to a traumatic, osteoporotic or metastatic thoracolumbar compression fracture at our hospital between 2012 and 2020 were included. Median follow-up was 0.9 years with a minimum follow-up of 6 months. Radiographic and clinical outcome was analyzed directly, 6 weeks, 12 weeks, 6 months postoperatively, and at last follow-up.
Results
Anterior vertebral body height of all patients improved significantly by mean 6.2 ± 4.8 mm directly postoperatively (p < 0.0001) and remained at 4.3 ± 5.1 mm at last follow-up compared to preoperatively (p < 0.0001). The fracture kyphosis angle of all patients improved significantly by mean 5.8 ± 6.9 degrees directly postoperatively (p < 0.0001) and remained at mean 4.9 ± 6.9 degrees at last follow-up compared to preoperatively (p < 0.0001). The segmental kyphosis angle of all patients improved significantly by mean 7.1 ± 7.6 degrees directly postoperatively (p < 0.0001) and remained at mean 2.8 ± 7.8 degrees at last follow-up compared to preoperatively (p = 0.03). Back pain was ameliorated from a preoperative median Numeric Rating Scale value of 6.5 to 3.0 directly postoperatively and further bettered to 1.0 six months postoperatively (p = 0.0001). Revision surgery was required in one patient after 0.4 years.
Conclusion
Vertebral body stenting is a safe and effective treatment option for osteoporotic, traumatic and metastatic compression fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thoracolumbar compression fractures affect a minimum of five million people worldwide per year [1,2,3]. Occurring in young and elderly patients, vertebral compression fractures constitute a major health-care problem of increasing impact [4]. Even though there is still no general consensus for treatment of compression fractures with no accompanying neurological impairment, surgical vertebral augmentation may be warranted to prevent progressive loss of vertebral body height, spinal kyphosis, pain, reduced mobility and independence, as well as psychological stress [5,6,7,8]. Moreover, a recent meta-analysis evaluating sixteen clinical trials favors surgical treatment for vertebral compression fractures [9]. Percutaneous vertebral augmentation procedures—such as vertebroplasty, balloon kyphoplasty and vertebral body stents—have emerged as valid anterior column reconstruction techniques for thoracolumbar compression fractures. They provide early mobilization, higher pain alleviation and long-term bone consolidation compared to conservative treatment options [10, 11]. Vertebroplasty is mainly applied for fracture stabilization without the intention of vertebral height restoration, while balloon kyphoplasty aims to correct the deformity through creation of an intravertebral cavity filled with cement. However, loss of vertebral body height and realignment after deflation of the balloon remained challenging [12]. Therefore, the vertebral body stenting system (VBS) was developed, which utilizes a balloon-catheter-mounted stent. The stent is deployed through inflation of the balloon inside the vertebral body, creating intrinsic mechanical stability after balloon deflation. Height restoration is held through polymethylmethacrylate (PMMA) cement injection [12, 13]. In comparison to balloon kyphoplasty or vertebroplasty, vertebral body stenting (VBS) intends to combine fracture consolidation and permanent height restoration [12, 14, 15]. Due to the relative novelty of this technique [16,17,18], there are currently only a few, yet promising studies evaluating the vertebral body stenting system [12, 13, 15, 18, 19]. However, there is only limited clinical and radiological evidence proving safety and efficacy of the vertebral body stenting system in terms of restoration and maintenance related to anterior column reconstruction in thoracolumbar compression fractures.
Therefore, the aim of this study was to assess safety and efficacy of vertebral body stenting by analyzing (1) radiographic outcome, (2) clinical outcome, and (3) perioperative complications in patients with vertebral compression fractures treated with VBS at minimum 6-month follow-up.
Material and methods
We conducted a single-center, retrospective cohort study. Institutional Review Board approval was provided (KEK2020/02976). All patients undergoing VBS procedures for traumatic, osteoporotic, or metastatic thoracolumbar compression fractures between 01/2012 and 12/2020 were included in the study. Minimum follow-up period was 6 months after surgery. The patient selection process is outlined in Fig. 1. Traumatic fractures were defined as fractures from high-energy trauma (Table 2). Osteoporotic fractures were specified as low-energy traumatic or fractures without previous trauma and previous documented diagnosis of osteoporosis. All low-energy and atraumatic fractures underwent intraoperative vertebral biopsy. In case of a positive biopsy result, fractures were classified as a metastatic fracture.
Study population
In total, 78 patients (mean age, 61 ± 14 [21–90] years; 66.7% female) with 80 pairs of vertebral body stents (= 160 VBS total) were included. Of those, 57 patients (73%) received additional posterior instrumentation (52 = percutaneous instrumentation, 5 = open instrumentation,) one vertebra above and one vertebra below the fractured vertebra [20,21,22,23]. Four (5.1%) patients underwent further decompression at the fracture site and 32 (40%) adjacent segment cementation. Forty-nine patients with traumatic fractures were allocated to the ‘traumatic group’. Twenty-four patients with osteoporotic fractures were allocated to the ‘osteoporotic group’. The remaining five patients with metastatic fractures were assigned to the ‘metastatic group’. Median follow-up was 0.9 [0.6; 1.2] years with 49 (62.8%) patients having a minimum of 12-month follow-up. Patient demographics are outlined in Table 1. The underlining trauma mechanism was in 25 percent an atraumatic fracture occurrence, in 12 percent due to an inadequate low-energy trauma, and in 63 percent a high-energy trauma. Patients presented with mean 1.4 ± 0.8 [1,2,3,4,5] fractures with 28 percent of all patients suffering from multiple fractures. Three patients (3.8%) suffered from a preoperative neurological deficit at first clinical presentation. Detailed fracture characteristics are shown in Table 2.
VBS stenting procedure
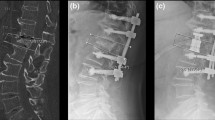
All procedures were performed under general anesthesia and according to the surgical guideline for vertebral body stenting by DePuy Synthes [24, 25]. Patients were placed in prone position on a radiolucent table. Access Kit 4.7 (DePuy Synthes Spine, Inc., Raynham, MA, USA) was utilized for transpedicular access. Under biplanar fluoroscopic-guidance, access instruments were advanced through two small skin incisions until they contacted the pedicle. After radiographic confirmation of the correct trajectory, instruments were advance through the pedicle and into the vertebral body, using a bilateral transpedicular approach. An access channel was created through trocars guided through the access instruments. The afterward inserted plunger was used to decide on the correct vertebral body balloon size. After advancement of two VBS systems through the corresponding channel into the vertebra, the VBS balloons were simultaneously inflated with a contrast-saline solution up to a pressure of 30 atmospheres until full balloon expansion was achieved followed by deflation and removal of the balloons, leaving the former surrounding stents in the vertebra to support the restored vertebral height. Under fluoroscopic guidance, polymethylmethacrylate (PMMA) cement (Vertecem V + , DePuy Synthes, Raynham, MA, USA) was injected bilaterally into the stent cavities until the stents were completely filled with some cement outside the stent interdigitating with the surrounding bone (Fig. 2). Depending on the underlying fracture type, the described procedure was followed by open or percutaneous posterior instrumentation. Postoperative regimen included supine positioning, immediate mobilization, pain medication according to the guidelines provided by the WHO, physiotherapeutic interventions and standing radiographs prior to hospital dismissal, 6 weeks, 12 weeks, 6 months and 12 months postoperatively.
Assessment of radiographic outcome
Radiographic and clinical analyses were performed preoperatively, directly postoperatively as well as 6 weeks, 12 weeks, 6 months and 12 months postoperatively. Radiographic vertebral measurements were conducted on plain anterior–posterior (ap) and lateral radiographs according to the method described by Eschler et al. [26]. These include the anterior, middle and posterior vertebral body height, as well as the fracture kyphosis, scoliosis and segmental kyphosis angle [26]. Global alignment parameters, enclosing lumbar lordosis (LL), lower lumbar lordosis (L4 to S1 [LLL]), pelvic incidence (PI) and pelvic tilt (PT) were determined on plain radiographs according to the method described by Fujii et al. [27]. Postoperative thoracic, thoracolumbar or lumbar radiographs were taken according to the underlying fracture level. Minimally clinical relevance was set at ≥ 2 mm or ≥ 2.5 degrees difference [28]. Figure 3 depicts the radiographic outcome measures. Radiographic data collection was conducted by an experienced and fellowship-trained spine surgeon, who was not involved in subsequent statistical analysis.
Radiographic outcome measurements in a lateral view and b anterior–posterior view on plain lumbar x-rays. PH = posterior vertebral body height. MH = middle vertebral body height. AH = anterior vertebral body height. FKA = fracture kyphosis angle. SKA = segmental kyphosis angle. FSA = fracture scoliosis angle
Assessment of clinical outcome
Clinical outcome was analyzed using the numeric rating scale (NRS) for pain evaluation and with patient-related outcome measurements (PROMs) such as COMI and EQ-5D [29, 30]. Complication rates were analyzed intraoperatively (such as blood loss and material failure), as well as radiographically (such as stent cut out, cement leakage or secondary fractures) and clinically (requirement of revision surgery).
Assessment of complications
Assessment of complications was categorized as material failure, cement leakage, VBS cutout or migration, and systemic complications related to the procedure. Material failure was categorized in insufficient balloon inflation or insufficient stent deployment. Insufficient balloon inflation was defined as a burst balloon or leaking contrast agent despite compliance with the maximum permitted filling volume and pressure. Insufficient stent deployment was specified as any non-ubiquitous round deployment. Cement leakage was defined as any cement outside the cortical border or intravascular cement. Any stent laying at any part outside of the vertebral cortical border was taken into account for a stent cut out. Systemic adverse events were defined as any event resulting in death, any life-threatening medical condition, permanent physical impairment or severe allergic reaction. Analysis was conducted by two authors neither involved in the patients’ operation nor clinical care.
Statistical analysis
Statistical Analysis was performed with GraphPad PRISM Version 8.0.1 (GraphPad Software, San Diego, California, USA). Normal Gaussian distribution was tested with Shapiro–Wilk test. If normally distributed, descriptive statistics are presented as mean ± standard deviation (range minimum—maximum {95% confidence interval of median lower, upper}). For non-normally distributed data, descriptive statistics are shown with median [Interquartile range (IQR) 25% percentile; 75% percentile] (range minimum–maximum {95% confidence interval of median lower, upper}). Single group comparisons were conducted with paired (un-paired) t-test for normally distributed data and with Wilcoxon signed rank test (Mann–Whitney U-Test) for non-normally distributed data. For paired multiple group comparisons, mixed effects analysis with Tukey’s multiple comparisons test was performed. Statistical significance was set at α ≤ 0.05.
Results
Anterior vertebral body height
Anterior vertebral body height of all patients improved significantly by mean 6.2 ± 4.8 (− 5.2–15.2) mm directly postoperatively compared to preoperatively (p < 0.0001). Mean correction remained at 4.3 ± 5.1 (− 8.6–14.8) mm at last follow-up compared to preoperatively (p < 0.0001). Loss of height correction was mean − 1.8 ± 2.4 (− 8.8–3.1) mm at last follow-up compared to postoperatively (p < 0.0001). In the osteoporotic group, mean anterior vertebral body height restoration was 5.6 ± 3.8 (− 0.8–13.3) mm directly postoperatively compared to preoperatively (p < 0.0001). At last follow-up mean correction stayed at 3.9 ± 4.7 (− 4–14.8) mm compared to preoperatively (p = 0.006). Loss of height correction was mean − 1.6 ± 2.7 (− 8.8–2.8) mm at last follow-up compared to directly postoperatively (p = 0.08). In the traumatic group, the anterior vertebral body height improved significantly by mean 6.6 ± 5.2 (− 5.2 to 5.2) mm directly postoperatively compared to preoperatively (p < 0.0001). The correction remained at mean 4.5 ± 5.9 (− 8.6–13.4) mm at last follow-up compared to preoperatively (p < 0.0001). Loss of height improvement presented as mean − 1.9 ± 2.3 (− 6.6–3.1) mm at last follow-up compared to directly postoperatively (p < 0.0001). In the metastatic group, mean vertebral body height restoration was 5.1 ± 5.7 (− 0.4–13.1) mm directly postoperatively compared to preoperatively. At last follow-up, mean correction stayed at 4.0 ± 6.2 (− 3.8–12.4) mm compared to preoperatively. Loss of height correction was mean − 1.1 ± 1.5 (− 3.4–0.2) mm at last follow-up compared to directly postoperatively. In patients with underwent posterior instrumentation, anterior vertebral body height correction improved significantly by mean 6.4 ± 5.2 (− 5.2–15.2) mm directly postoperatively compared to preoperatively (p < 0.0001). Mean correction remained at 4.5 ± 5.6 (− 8.6–14.8) mm at last follow-up compared to preoperatively (p < 0.0001). Loss of height correction was mean − 0.9 ± 4.9 (− 8.8—24) mm at last follow-up compared to postoperatively (p < 0.0001). In patients without posterior instrumentation, anterior vertebral body height correction improved significantly by mean 5.5 ± 3.6 (− 2.3–13.3) mm directly postoperatively compared to preoperatively (p < 0.0001). The correction remained at mean 3.7 ± 3.5 (-3.8—9.2) mm at last follow-up compared to directly preoperatively (p = 0.001). Loss of height correction was mean − 1.7 ± 2.4 (− 6.6–3.1) mm at last follow-up compared to directly postoperatively (p = 0.04). There was a significant difference in the anterior vertebral body height between instrumented and non-instrumented patients preoperatively (22.3 [16.4; 26.4] (9.8–26.8 {19.8; 24.4}) mm vs. 20.0 [14.0; 22.9] (10.0–19.9 {14.2; 22.9}) mm; p = 0.04) as well as at last follow-up (27.5 [24.4; 30.2] (13.6–20.8 {25.4; 28.7}) mm vs. 21.2 [19.2; 26.3] (16.8–34.0 {19.2; 26.1}) mm; p = 0.001).
Fracture kyphosis angle
The fracture kyphosis angle of all patients improved significantly by mean 5.8 ± 6.9 (7–29.9) degrees directly postoperatively compared to preoperatively (p < 0.0001). Mean correction remained at 4.9 ± 6.9 (7.9–27.2) degrees at last follow-up compared to preoperatively (p < 0.0001). Loss of kyphosis correction was mean − 0.9 ± 4.3 (− 14.1–15.3) degrees at last follow-up compared to directly postoperatively (p > 0.34). In the osteoporotic group, mean fracture kyphosis angle correction was 3.7 ± 5.9 (− 7–16.8) degrees directly postoperatively compared to preoperatively (p = 0.07). At last follow-up mean correction stayed at 4.2 ± 6.8 (− 7.9–19.5) degrees compared to preoperatively (p = 0.08). Loss of fracture kyphosis angle correction was mean − 0.5 ± 3.5 (− 7.7–8.1) degrees at last follow-up compared to directly postoperatively (p = 0.99). In the traumatic group, the fracture kyphosis angle improved significantly by mean 5.9 ± 6.4 (− 2.8–27.6) degrees directly postoperatively compared to preoperatively (p < 0.0001). The correction remained at mean 4.3 ± 6.4 (− 6–20.5) degrees at last follow-up compared to directly postoperatively (p = 0.0002). Loss of fracture kyphosis angle improvement presented as mean − 1.4 ± 3.7 (− 14.1–4.8) degrees at last follow-up compared to directly postoperatively (p = 0.14). In the metastatic group, mean fracture kyphosis angle correction was 14.6 ± 10 (− 3.0–29.9) degrees directly postoperatively compared to preoperatively. At last follow-up, mean correction stayed at 11.1 ± 9.1 (4.6–27.2) degrees compared to preoperatively. Loss of fracture kyphosis angle correction was mean − 3.4 ± 5.7 (− 9.1–5.2) degrees at last follow-up compared to directly postoperatively. In patients who underwent additional posterior instrumentation, the fracture kyphosis angle of all patients improved significantly by mean 6.2 ± 7.1 (− 7–29) degrees directly postoperatively compared to preoperatively (p < 0.0001). Mean correction remained at 5.3 ± 6.6 (− 5.6–27.2) degrees at last follow-up compared to preoperatively (p < 0.0001). Loss of kyphosis correction was mean − 0.9 ± 4.0 (− 9.1–15.3) degrees at last follow-up compared to directly postoperatively (p = 0.68). In patients without posterior instrumentation, the fracture kyphosis angle of all patients improved significantly by mean 5.3 ± 6.5 (− 4.3–16.7) degrees directly postoperatively compared to preoperatively (p = 0.02). The correction remained at mean 3.9 ± 7.4 (− 7.9–19.5) degrees at last follow-up compared to directly postoperatively (p = 0.2). Loss of fracture kyphosis angle improvement presented as mean -1.3 ± 5.3 (− 8.1–14.1) degrees at last follow-up compared to directly postoperatively (p = 0.91). There was no significant difference in the preoperative median fracture kyphosis angle between instrumented and non-instrumented patients (8.5 [3.5; 15.0] (0.1–32.3 {5.7; 10.2}) degrees vs. 7.9 [3.2; 14.3] (0–19.5 {3.2; 19.5}) degrees; p > 0.4). However, a significant difference was detected at last follow-up (4.3 [1.9; 7.1] (0–21.6 {2.9; 5.4}) degrees vs. 7.9 [3.2; 14.3] (0–19.5 {3.2; 14.1}) degrees; p = 0.01), showing a lower median fracture kyphosis angle in patients with posterior instrumentation.
Segmental kyphosis angle
The segmental kyphosis angle of all patients improved significantly by mean 7.1 ± 7.6 (− 8.6–28.3) degrees directly postoperatively compared to preoperatively (p < 0.0001). Mean correction remained at 2.8 ± 7.8 (− 16.6–31.3) degrees at last follow-up compared to preoperatively (p = 0.03). Loss of segmental kyphosis angle correction was mean − 3.9 ± 5.3 (− 18.4–15.4) degrees at last follow-up compared to directly postoperatively (p < 0.0001). In the osteoporotic group, mean segmental kyphosis angle correction was 6 ± 7.7 (− 28.3–8.6) degrees directly postoperatively compared to preoperatively (p = 0.01). At last follow-up mean correction stayed at − 2.3 ± 9.5 (− 31.3–7.6) degrees compared to preoperatively (p = 0.9). Loss of segmental kyphosis angle correction was mean 3.8 ± 6 (− 5.4–15.4) degrees at last follow-up compared to directly postoperatively (p = 0.07). In the traumatic group, the segmental kyphosis angle improved significantly by mean 7.8 ± 7.3 (− 5.7–22.4) degrees directly postoperatively compared to preoperatively (p < 0.0001). The correction remained at mean 3.0 ± 6.7 (− 12.5–18.8) degrees at last follow-up compared to directly postoperatively (p = 0.04). Loss of segmental kyphosis angle improvement presented as mean − 4.1 ± 5.1 (− 18.4–15.4) degrees at last follow-up compared to directly postoperatively (p < 0.0001). In the metastatic group, mean segmental kyphosis angle correction was 6.4 ± 10.4 (− 2.6–23.4) degrees directly postoperatively compared to preoperatively. At last follow-up, mean correction stayed at 3.4 ± 11.1 (− 5.4–21.5) degrees compared to preoperatively. Loss of segmental kyphosis angle correction was mean -3.0 ± 3.1 (− 8.5–1.2) degrees at last follow-up compared to directly postoperatively. In patients who underwent additional posterior instrumentation, the segmental kyphosis angle of all patients improved significantly by mean 8.2 ± 7.2 (− 5.7–28.3) degrees directly postoperatively compared to preoperatively (p < 0.0001). Mean correction remained at 3.2 ± 8.0 (− 12.5–31.3) degrees at last follow-up compared to preoperatively (p = 0.06). Loss of kyphosis correction was mean − 4.2 ± 5.1 (− 15.4–15.4) degrees at last follow-up compared to directly postoperatively (p < 0.001). In patients without posterior instrumentation, the segmental kyphosis angle of all patients improved by mean 4.6 ± 7.7 (− 8.6–19.0) degrees directly postoperatively compared to preoperatively (p = 0.13). The correction remained at mean 1.7 ± 7.0 (− 16.6–13.2) degrees at last follow-up compared to directly postoperatively (p = 0.89). Loss of segmental kyphosis angle improvement presented as mean − 2.8 ± 5.6 (− 18.4–5.4) degrees at last follow-up compared to directly postoperatively (p = 0.27). Between instrumented and non-instrumented patients, no significant difference was seen preoperatively (11.2 [0.2; 18.7] (− 22.7–32.8 {6.4; 13.8}) degrees vs. 16.8 [2.2; 21.7] (− 15.1–32.8 {2.3; 21.6}) degrees; p = 0.2) in the median segmental kyphosis angle. Yet, a significant difference was detected at last follow-up (7.3 [2.1; 12.4] (− 17.9–26.2 {4.3; 10.8}) degrees versus 14.0 [3.8; 18.9] (− 15.2–28.1 {5.1; 28.1}) degrees; p = 0.01), indicating a lower median segmental kyphosis angle in patients with posterior instrumentation. Radiographic outcome is described in Table 3.
Clinical outcome
Back pain, quantified by the Numeric Rating Scale (NRS) was 6.5 [5; 8] (0–10 {6; 7}) preoperatively. Directly postoperatively, a pain of 3.0 [3; 4] (2–8 {3; 4}) (p = 0.0001), 6 weeks postoperatively a pain of 2.0 [0; 4] (0–8 {2;3}) (p = 0.0001), 6 months postoperatively a pain of 1.0 [0; 4] (0–8 {0; 2}) (p = 0.0001) and 12 months postoperatively a pain of 0.5 [0; 2] (0–6 {0;1}) (p = 0.0001) was present. The COMI-Back Questionnaire, presented a median score of 6.9 [3.1; 8.1] (1.5–10.0 {3.1; 9.0}) preoperatively. Six weeks postoperatively, a score of 4.5 [2.2; 6.3] (0–8 {3; 6.2}) (p = 0.11), 6 months postoperatively a score of 3.3 [1.5; 5.6] (0–8.8 {1.7; 5.5}) (p = 0.06) and 12 months postoperatively a score of 2.6 [0.9; 3.5] (0–7.7 {0; 5}) (p = 0.07) was measured. Health-related quality of life, measured with the EQ-5D questionnaire, showed a score of 0.5 [-0.1; 0.9] (− 0.4–0.9 {− 0.4; 0.85}) preoperatively. A score of 0.8 [0.6; 0.9] (− 0.02–1.0 {0.6; 0.8}) (p = 0.1) was determined 6 weeks postoperatively, a score of 0.7 [0.7; 1.0] (0.2–1.0 {0.7; 1.0}) (p = 0.1) 6 months postoperatively and a score of 0.8 [0.7; 1.0] (0.5–1.0 {0.7; 1.0}) (p = 0.4) 12 months postoperatively. Clinical outcome is illustrated in Fig. 4.
The clinical outcome is shown. NRS = Numeric Rating Scale. COMI = Core Outcome Measures Index for Back Pain. EQ-5D = EuroQuol-5D Questionnaire. X-axis = absolute score. Y-axis = time point of measurement: preoperative, directly postoperative, 6 weeks, 6 months and 12 months postoperative. Values are displayed as median with error bars representing the interquartile range
Complications
Intraoperative material failure was present in 5% (n = 4); therein no stent deployment could be seen in two patients and insufficient ballooning in further two patients. A stent cut out was detected in 3.8% (n = 3) and an adjacent segment fracture in 1.3% (n = 1) of all patients. No secondary fracture surrounding the stent was present. Cement leakage could be seen in 41.3% (n = 33) of all patients. Cement leakage into the anterolateral, paravertebral region was present in 21 patients, intradiscal cement leakage in eleven patients and posterior cement leakage into the spinal canal in one patient. No vascular cement leakage was detected. None of the cement leakages had a clinically relevant consequence requiring further treatment. Clinically, revision surgery was required in one (1.3%) patient after 0.4 years. The patient suffered from multiple hematogenic infections with Streptococcus mitis, Staphylococcus aures and Serratio marcensens at the time point of the initial trauma and index surgery. Five months after index surgery, he developed potential procedure related spondylodiscitis with subsequent bone necrosis at the VBS level. Therefore, a subtotal corporectomy with cage replacement, disc biopsy and posterior instrumentation was performed. Intraoperative biopsies and sonication remained negative. However, due to the prior infections with known pathogen, an empirical antibiotic therapy was installed. In the six-year follow-up, the patient reported a very good clinical outcome with intermittently mild pain (VAS 2) and restored mobility. His general health status remained reduced due to a chronically severely decompensated ethyl toxic liver cirrhosis. Radiographic follow-up showed no adjacent segment pathologies nor material failure. Complications are displayed in Table 4.
Discussion
Percutaneous vertebral augmentation procedures have emerged as valid anterior column reconstruction techniques for thoracolumbar compression fractures. They provide early mobilization, higher pain alleviation and long-term bone consolidation compared to conservative treatment options [10, 11]. The vertebral body stenting augmentation technique combines fracture consolidation and permanent height restoration in comparison to balloon kyphoplasty or vertebroplasty [12, 14, 15]. Due to the relative novelty of the vertebral body stenting system, there are currently only a few, yet promising studies evaluating the vertebral body stenting system [12, 13, 15,16,17,18,19]. Therefore, we have conducted a single-center retrospective cohort study, aiming to determine the short- and long-term radiographic and clinical outcome of patients who have received a VBS due to a traumatic, osteoporotic or metastatic thoracolumbar compression fracture.
In this study, a mean anterior vertebral body height correction of 6.2 ± 4.8 mm directly postoperatively and of 4.3 ± 5.1 mm at last follow-up was detected (p < 0.0001). Garnon et al. evaluated the restoration of the preoperative most depressed vertebral body height, not differentiating between anterior-, middle-, and posterior height reconstruction. They reported a mean restoration of 3.8 mm [15], which is a lower height restoration than measured in this study. Diel et al. analyzed an anterior vertebral body height of mean 20.3 to 24.5 mm six months postoperatively, which is similar to our findings (mean 21.5 to 26.6 mm; p < 0.0001) [12]. With vertebroplasty (VP), a mean anterior height restoration of 1.8–2.5 mm is described, whereas a correction of mean 2.2 mm is reported in balloon kyphoplasty (BKP) [31, 32]. Thus, the VBS system led to a higher anterior vertebral body height restoration compared to VP or BKP in this study.
Here, a fracture kyphosis angle reduction of mean 5.8 ± 6.9 degrees directly postoperatively was measured (p < 0.0001). The reduction remained stable at 4.9 ± 6.9 degrees at last follow-up postoperatively (p < 0.0001). Other studies reported a lower angle correction directly postoperatively, ranging between 3.2 and 4.6 degrees, however exact long-term results—six- and 12 months postoperatively—were not specifically provided [15, 17, 18, 33, 34]. In the fracture group, a fracture angle correction of 5.9 ± 6.4 degrees was achieved. This lays in accordance with reported angle correction of 3.2 to 7.3 degrees in the literature [17, 34, 35]. Hiwatashi et al. showed a kyphosis angle reduction of mean 3 degrees with BKP and a reduction of mean 2.7 degrees with VP [32]. This indicates that VBS can achieve a higher fracture kyphosis angle reduction than BKP or VP.
Back pain was ameliorated from a preoperative median Numeric Rating Scale value of 6.5 [5; 8] to 3.0 [3; 4] directly postoperatively and further bettered to 1.0 [0; 4] six months postoperatively (p = 0.0001). This represents better pain alleviation as reported by Klezl et al., who measured a mean pain score of 4.0 in the osteoporotic and 2.2 in the traumatic group six months postoperatively while also having analyzed a higher preoperative pain value of mean 8.9 in the osteoporotic and 9.7 in the traumatic groups[17]. Other studies evaluating the outcome of VBS have not taken back pain measurements into account. Comparable results were found in a meta-analysis of vertebroplasties and balloon kyphoplasties, in which patients showed a pain reduction on the NRS of 3.9 and 4.1 points, respectively [36].
Cement leakage occurred in 33 patients (41.5%) in this study. However, there was only one relevant posterior leakage and no vascular cement leakage. None of the patients suffered from clinical consequences requiring surgical revision. Other studies reported similar cement leakage rates with the VBS system, ranging from 0 to 55.4% [33, 37,38,39]. VPs and BKPs show mostly similar rates of cement leakages [40,41,42,43]. Cement leakages in vertebroplasties range from nine to thirty-eight percent, which is comparable to our findings with VBS. Noriega et al. reported a cement leakages in balloon kyphoplasties between seven and fifteen percent, whereas Vendeuvre et al. reported a cement leakage rate of 41.7%, which is an equal rate compared to our study [33, 42, 43]. A slightly higher rate of cement leakages with the VBS system could be attributed to different patient population characteristics: Patients treated with VBS suffered more often from high-energy fractures, or thoracolumbar burst fractures, involving the posterior wall and bursting of the endplates [33, 34, 43]. This increases the likelihood of cement leakage compared to the fracture pattern of patients treated with vertebroplasty or balloon kyphoplasty. Zhang et al. described high preoperative compression ratios as a statistical significant independent risk factor for cement leakage with an Odds Ratio of 0.23 (p = 0.025) [44]. Patients treated with VP or BKP often suffered from low-energy and non-traumatic osteoporotic fractures, implicating a lower impact on vertebral walls and endplates [9, 40]. Thus, cement leakage is less likely in vertebroplasty and balloon kyphoplasty than in VBS augmentation due to the different fracture patterns treated and not due to the surgical technique itself. Cement leakage in the VBS system, as in other vertebral augmentation techniques, can be reduced technically by vertebral body lavage prior to augmentation [45]. Additionally, a longer waiting period between cement preparation and injection as well as in between the cement injections aim to reduce cement leakage due to higher cement viscosity.
Revision surgery was required in one (1.3%) patient after 0.4 years, which lays well in the range reported in the literature [12, 34].
The VBS system implies higher product cost in comparison to other vertebral augmentation techniques, such as balloon kyphoplasty. Besides the higher production costs due to the included metal stent in VBS, this is mostly due to technical reasons: In balloon kyphoplasties, the balloon can be reused multiple times even in multilevel surgeries. Whereas in VBS, the balloon, mounted with the stent, cannot be reused. One stent-balloon combination is needed per pedicle site in order to inflate the stent. However, when looking at the advantages of the VBS system, which are related to the stent remaining in-situ, higher costs seem acceptable [12, 14, 15].
This is the first study also evaluating other relevant vertebral alignment parameter such as segmental kyphosis angle correction and vertebral scoliosis angle as well as global alignment parameters. Additionally, this is the first investigation measuring clinical outcome with the validated PROMs COMI and EQ-5D.
Limitations of this study lay in its retrospective nature with no control group. Additionally, the sample size of patients with metastatic fractures was small (n = 5), leaving too less power to provide statistical testing. However, this is the first study presenting absolute radiographic outcome data on this study population. Cianfoni et al. analyzed overall, yet not specific radiographic outcome of vertebral body stenting for metastatic fractures [46]. Moreover, additional posterior instrumentation may maintain sagittal and coronal alignment parameters independently of the anterior column reconstruction wit VBS. However, while the degree of correction was higher with additional instrumentation, restoration and maintenance of vertebral body height, fracture kyphosis angle and segmental kyphosis was achieved for all fractures treated with VBS independently of posterior instrumentation.
Conclusion
This study revealed that the VBS restored and maintained focal and global sagittal and coronal alignment parameters in patients suffering from traumatic, osteoporotic and metastatic fractures of the thoracolumbar spine. The rate and degree of complications did not exceed these from different surgical treatment modalities for these type of pathologies making it a safe and valid treatment option for anterior column reconstruction in these patients. Future studies such as prospective randomized controlled trials are warranted to confirm these findings.
References
Kraemer WJ, Schemitsch EH, Lever J, McBroom RJ, McKee MD, Waddell JP (1996) Functional outcome of thoracolumbar burst fractures without neurological deficit. J Orthop Trauma 10:541–544
Wood KB, Li W, Lebl DR, Ploumis A (2014) Management of thoracolumbar spine fractures. The Spine Journal: Official Journal of the North American Spine Society 14:145–164
Bigdon SF, Saldarriaga Y, Oswald KAC, Muller M, Deml MC, Benneker LM, EckerAlbers TMCE (2022) Epidemiologic analysis of 8000 acute vertebral fractures: evolution of treatment and complications at 10-year follow-up. J Orthop Surg Res 17:270
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Min Res Off J Am Soc Bone Miner Res 22:465–475
Cortet B, Blotman F, Debiais F, Huas D, Mercier F, Rousseaux C, Berger V, Gaudin AF, Cotte FE (2011) Management of osteoporosis and associated quality of life in post menopausal women. BMC Musculoskelet Disord 12:7
Rao RD, Singrakhia MD (2003) Painful osteoporotic vertebral fracture. Pathogenesis, evaluation, and roles of vertebroplasty and kyphoplasty in its management. J Bone Joint Surg Am 85:2010–2022
Varacallo MA, Fox EJ (2014) Osteoporosis and its complications. Med Clin North America 98:817–831
Venmans A, Lohle PN, van Rooij WJ (2014) Pain course in conservatively treated patients with back pain and a VCF on the spine radiograph (VERTOS III). Skeletal Radiol 43:13–18
Halvachizadeh S, Stalder AL, Bellut D, Hoppe S, Rossbach P, Cianfoni A, Schnake KJ, Mica L, Pfeifer R, Sprengel K, Pape HC (2021) Systematic Review and Meta-Analysis of 3 Treatment Arms for Vertebral Compression Fractures: A Comparison of Improvement in Pain, Adjacent-Level Fractures, and Quality of Life Between Vertebroplasty, Kyphoplasty, and Nonoperative Management. JBJS Rev 9(10):21
Maestretti G, Sutter P, Monnard E, Ciarpaglini R, Wahl P, Hoogewoud H, Gautier E (2014) A prospective study of percutaneous balloon kyphoplasty with calcium phosphate cement in traumatic vertebral fractures: 10-year results. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 23:1354–1360
Orcel P, Funck-Brentano T (2011) Medical management following an osteoporotic fracture. Orthopaed Traumatol Surg Res OTSR 97:860–869
Diel P, Roder C, Perler G, Vordemvenne T, Scholz M, Kandziora F, Furderer S, Eiskjaer S, Maestretti G, Rotter R, Benneker LM, Heini PF (2013) Radiographic and safety details of vertebral body stenting: results from a multicenter chart review. BMC Musculoskelet Disord 14:233
Rotter R, Martin H, Fuerderer S, Gabl M, Roeder C, Heini P, Mittlmeier T (2010) Vertebral body stenting: a new method for vertebral augmentation versus kyphoplasty. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 19:916–923
Bousson V, Hamze B, Odri G, Funck-Brentano T, Orcel P, Laredo JD (2018) Percutaneous vertebral augmentation techniques in osteoporotic and traumatic fractures. Semin Interv Radiol 35:309–323
Garnon J, Dore B, Auloge P, Caudrelier J, Dalili D, Ramamurthy N, Koch G, Cazzato RL, Gangi A (2019) Efficacy of the vertebral body stenting system for the restoration of vertebral height in acute traumatic compression fractures in a non-osteoporotic population. Cardiovasc Intervent Radiol 42:1579–1587
Furderer S, Anders M, Schwindling B, Salick M, Duber C, Wenda K, Urban R, Gluck M, Eysel P (2002) Vertebral body stenting. A method for repositioning and augmenting vertebral compression fractures. Orthopade 31:356–361
Klezl Z, Majeed H, Bommireddy R, John J (2011) Early results after vertebral body stenting for fractures of the anterior column of the thoracolumbar spine. Injury 42:1038–1042
Muto M, Greco B, Setola F, Vassallo P, Ambrosanio G, Guarnieri G (2011) Vertebral body stenting system for the treatment of osteoporotic vertebral compression fracture: follow-up at 12 months in 20 cases. Neuroradiol J 24:610–619
Itshayek E, Fraifeld S, Vargas AA, Schroeder J, Kaplan L, Barzilay Y, Rosenthal G, Shoshan Y, Cohen JE (2014) Efficacy and safety of vertebral stenting for painful vertebral compression fractures in patients with metastatic disease. Neurol Res 36:1086–1093
Blattert TR et al (2018) Nonsurgical and surgical management of osteoporotic vertebral body fractures: recommendations of the spine section of the german society for orthopaedics and trauma (DGOU). Global spine journal 8:50S-55S
Hoppe S, Aghayev E, Ahmad S, Keel MJB, Ecker TM, Deml M, Benneker LM (2017) short posterior stabilization in combination with cement augmentation for the treatment of thoracolumbar fractures and the effects of implant removal. Glob Spine J 7:317–324
Schnake KJ et al (2018) Classification of osteoporotic thoracolumbar spine fractures: recommendations of the spine section of the german society for orthopaedics and trauma (DGOU). Global spine journal 8:46S-49S
Vaccaro AR, Schroeder GD, Kepler CK, Cumhur Oner F, Vialle LR, Kandziora F, Koerner JD, Kurd MF, Reinhold M, Schnake KJ, Chapman J, Aarabi B, Fehlings MG, Dvorak MF (2016) The surgical algorithm for the AOSpine thoracolumbar spine injury classification system. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 25:1087–1094
Eschler A, Ender SA, Schiml K, Mittlmeier T, Gradl G (2015) Bony healing of unstable thoracolumbar burst fractures in the elderly using percutaneously applied titanium mesh cages and a transpedicular fixation system with expandable screws. PLoS ONE 10:e0117122
Fujii K, Kawamura N, Ikegami M, Niitsuma G, Kunogi J (2015) Radiological improvements in global sagittal alignment after lumbar decompression without fusion. Spine 40:703–709
Kyrola KK, Salme J, Tuija J, Tero I, Eero K, Arja H (2018) Intra- and interrater reliability of sagittal spinopelvic parameters on full-spine radiographs in adults with symptomatic spinal disorders. Neurospine 15:175–181
Grieve R, Grishchenko M, Cairns J (2009) SF-6D versus EQ-5D: reasons for differences in utility scores and impact on reported cost-utility. Eur J Health Econ 10:15–23
Mannion AF, Porchet F, Kleinstuck FS, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D (2009) The quality of spine surgery from the patient’s perspective. Part 1: the Core Outcome Measures Index in clinical practice. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 18(3):367–373
Hiwatashi A, Moritani T, Numaguchi Y, Westesson PL (2003) Increase in vertebral body height after vertebroplasty. AJNR Am J Neuroradiol 24:185–189
Hiwatashi A, Westesson PL, Yoshiura T, Noguchi T, Togao O, Yamashita K, Kamano H, Honda H (2009) Kyphoplasty and vertebroplasty produce the same degree of height restoration. AJNR Am J Neuroradiol 30:669–673
Vendeuvre T, Brossard P, Pic JB, Billot M, Gayet LE, Pries P, Teyssedou S, Germaneau A, Rigoard P (2021) Vertebral balloon kyphoplasty versus vertebral body stenting in non-osteoporotic vertebral compression fractures at the thoracolumbar junction: a comparative radiological study and finite element analysis (BONEXP study). Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 30:3089–3098
Werner CM, Osterhoff G, Schlickeiser J, Jenni R, Wanner GA, Ossendorf C, Simmen HP (2013) Vertebral body stenting versus kyphoplasty for the treatment of osteoporotic vertebral compression fractures: a randomized trial. J Bone Joint Surg Am 95:577–584
Hartmann F, Griese M, Dietz SO, Kuhn S, Rommens PM, Gercek E (2015) Two-year results of vertebral body stenting for the treatment of traumatic incomplete burst fractures. Minim Invasive Ther Allied Technol 24:161–166
Beall D, Lorio MP, Yun BM, Runa MJ, Ong KL, Warner CB (2018) Review of vertebral augmentation: an updated meta-analysis of the effectiveness. Int J Spine Surg 12:295–321
Bozkurt M, Kahilogullari G, Ozdemir M, Ozgural O, Attar A, Caglar S, Ates C (2014) Comparative analysis of vertebroplasty and kyphoplasty for osteoporotic vertebral compression fractures. Asian Spine J 8:27–34
Korovessis P, Vardakastanis K, Vitsas V, Syrimpeis V (2014) Is Kiva implant advantageous to balloon kyphoplasty in treating osteolytic metastasis to the spine? Comparison of 2 percutaneous minimal invasive spine techniques: a prospective randomized controlled short-term study. Spine 39:E231-239
Tutton SM, Pflugmacher R, Davidian M, Beall DP, Facchini FR, Garfin SR (2015) KAST study: the kiva system as a vertebral augmentation treatment-a safety and effectiveness trial: a randomized, noninferiority trial comparing the kiva system with balloon kyphoplasty in treatment of osteoporotic vertebral compression fractures. Spine 40:865–875
Chang X, Lv YF, Chen B, Li HY, Han XB, Yang K, Zhang W, Zhou Y, Li CQ (2015) Vertebroplasty versus kyphoplasty in osteoporotic vertebral compression fracture: a meta-analysis of prospective comparative studies. Int Orthop 39:491–500
Diel P (2010) SWISSspine-a nationwide health technology assessment registry for balloon kyphoplasty: methodology and first results. Spine J Off J North Am Spine Soc 10:961–971
Noriega D, Marcia S, Theumann N, Blondel B, Simon A, Hassel F, Maestretti G, Petit A, Weidle PA, Mandly AG, Kaya JM, Touta A, Fuentes S, Pflugmacher R (2019) A prospective, international, randomized, noninferiority study comparing an implantable titanium vertebral augmentation device versus balloon kyphoplasty in the reduction of vertebral compression fractures (SAKOS study). Spine J Off J North Am Spine Soc 19:1782–1795
Noriega DC, Rodriotaguez-Monsalve F, Ramajo R, Sanchez-Lite I, Toribio B, Ardura F (2019) Long-term safety and clinical performance of kyphoplasty and SpineJack(R) procedures in the treatment of osteoporotic vertebral compression fractures: a pilot, monocentric, investigator-initiated study. Osteoporos Int Journal Established Result Cooperation Between Eur Foundat Osteoporosis Nat Osteoporos Found USA 30:637–645
Zhang TY, Zhang PX, Xue F, Zhang DY, Jiang BG (2020) Risk factors for cement leakage and nomogram for predicting the intradiscal cement leakage after the vertebra augmented surgery. BMC Musculoskelet Disord 21:792
Hoppe S, Elfiky T, Keel MJ, Aghayev E, Ecker TM, Benneker LM (2016) Lavage prior to vertebral augmentation reduces the risk for cement leakage. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 25:3463–3469
Cianfoni A, Distefano D, Pravata E, Espeli V, Pesce G, Mordasini P, La Barbera L, Scarone P, Bonaldi G (2019) Vertebral body stent augmentation to reconstruct the anterior column in neoplastic extreme osteolysis. J Neurointerv Surg 11:313–318
Funding
Funding for this study was provided by DePuy Synthes Inc., Raynham, MA, USA, to the institution of the authors, Department of Orthopaedic Surgery & Traumatology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Author information
Authors and Affiliations
Contributions
CEA contributed to conceptualization and design; KACO, JK and CT performed data collection and analysis; KACO performed writing—original draft preparation; CEA; JK; CT; MCD, SFB, SH, and LB performed writing—review and editing; CEA performed supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors indicate no potential conflict of interest.
Ethical approval
Institutional Review Board approval was provided (KEK2020/02976).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oswald, K.A.C., Kälin, J., Tinner, C. et al. Anterior thoracolumbar column reconstruction with the vertebral body stent—safety and efficacy. Eur Spine J 32, 934–949 (2023). https://doi.org/10.1007/s00586-023-07537-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07537-3