Abstract
Objectives
The aim of this study was to provide epidemiological data of pediatric patients suffering from cervical spinal trauma in Germany, in order to integrate these data in future decision-making processes concerning diagnosis and therapy.
Materials and Methods
Retrospective multicenter study includes all patients up to 16 years suffering from cervical spine injuries who were treated in six German spine centers between 01/2010 and 12/2016. The clinical databases were screened for specific trauma mechanism, level of injury as well as accompanying injuries. Diagnostic imaging and the chosen therapy were analyzed. Patients were divided into three age groups for further evaluation: age group I (0–6 years), age group II (7–9 years), age group III (10–16 years).
Results
A total of 214 children with 265 cervical spine injuries were included during the mentioned period. The mean age at the time of injury was 11.9 (± 3.9) years. In age group I, 24 (11.2%) patients were included, age group II consisted of 22 patients (10.3%), and 168 patients belonged to age group III (78.5%). Girls and boys were equally affected. In all age groups, falls and traffic accidents were the most common causes of cervical spine injuries. A total of 180 patients (84.1%) were treated conservatively, while 34 (15.9%) children underwent surgery. Distorsion/whiplash injury was the most common entity (n = 165; 68.2%). Children aged 0–9 years had significantly (p < 0.001) more frequent injuries of the upper cervical spine (C0-C2) compared to older age groups. Patients of age group III were more likely to suffer from injuries in subaxial localizations. Neurological deficits were rarely seen in all age groups. Head injuries did represent the most common accompanying injuries (39.8%, n = 92).
Conclusions
The upper cervical spine was more frequently affected in young children. Older children more often suffered from subaxial pathologies. The majority of cervical spinal column injuries were treated conservatively. Nevertheless, 15% of the hospitalized children had to be treated surgically.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pediatric patients with cervical spinal column injuries are a rarity in everyday clinical practice. This notion can be confirmed by the international literature, where the proportion of children with spinal column injuries compared to the overall number of injured children is described to range from 1 to 4% [2, 7, 9].
Most of the epidemiological data originate from the Anglo-American region, and the analysis of the incidences of spinal column injuries in adults shows considerable regional differences, as confirmed by a recent meta-analysis [9].
Thus, the aim of this study was to provide epidemiological data of pediatric patients suffering from cervical spinal trauma in Germany using a multicentric approach, in order to integrate these data in future decision-making processes for diagnosis and therapy.
Methods
At each center the present retrospective multicenter study was approved by the local ethics committee. The approval for the main study center was granted by the Ethics Committee of the State Medical Association of Rheinland-Pfalz (file number: 837.295.17).
The retrospective analysis included all patients up to 16 years of age, who were initially admitted to one of six study centers as inpatients due to a spinal column injury between January 2010 and December 2016.
An anonymous evaluation of the patients' demographic data was performed. In addition, the accident mechanism, concomitant injuries, the imaging diagnostics conducted, the injury level, the therapy performed and the duration of inpatient treatment were evaluated.
The trauma mechanism was recorded out of the medical chart and assigned:
-
fall < 3 m
-
fall > 3 m
-
car accident
-
bicycle accident
-
sports accidents
-
equestrian sports
-
jump in shallow water
-
others
Patients were divided into three age groups using the classification proposed by Meinig et al. [14]: age group I (0–6 years), age group II (7–9 years), age group III (10–16 years).
The statistical analysis was performed using SPSS Statistics (IBM, Version 23, New York, USA). In addition to the descriptive statistics, a correlation analysis according to Spearman and a group analysis was performed using the Student's t test. The significance level was set at p ≤ 0.05.
Results
A total of 214 children with 265 cervical spine injuries were included. The mean age at the time of injury was 11.9 (± 3.7) years. A total of 24 (11.2%) pediatric patients were included in the age group I, 22 (10.3%) in age group II and 168 patients (78.5%) in age group III (Fig. 1).
A total of 179 patients (83.6%) were treated conservatively, whereas 34 (16.4%) children were treated surgically.
Gender distribution
Gender distribution of the mentioned population was balanced (female n = 106, 49.5%; male n = 108; 50.5%).
Accident mechanism
Figure 2 displays the distribution of the observed accident mechanisms. Traffic accidents were the most common accident mechanism (n = 59; 27.6%), followed by sport accidents (n = 57; 26.6%) and fall from height lower than 3 m (n = 43; 20.1%).
Diagnostics
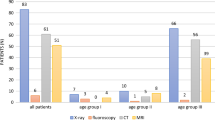
Conventional radiographs were performed in 172 (80.4%) patients. A total of 99 (46.3%) children and adolescents received a magnet resonance image (MRI). All over 74 (34.6%) patients received a computed tomography (CT). Dynamic fluoroscopic examination was performed in a minority of 31 (14.5%) children (Fig. 3).
An MRI with anesthesia was necessary in 2 patients of the age group I (32%), in one patient of age group II (4.5%), and in four patients of age group III (2.4%), respectively.
An expectable significant correlation between age distribution and diagnostics was found: the older the patients, the more frequently a CT (r = 0.202; p = 0.001) as well as conventional radiograph (r = 0.086; p = 0.430) was used for diagnostic imaging. MRI (r = –0.178; p = 0.001) or fluoroscopy (r = –0.168; p = 0.001) was significantly more frequently performed in younger patients.
Accompanying injuries
A total of 231 concomitant injuries were observed. Head injuries dominated in the mentioned cohort (n = 92, 39.8%), followed by injuries of the extremities (n = 21, 9.1%), the chest (n = 14, 6.1%), the pelvis (n = 9, 3.9%) and the abdomen (n = 6, 2.6%). A second spinal injury located at the thoracolumbar spine was found in one of the cases (Fig. 4).
ISS (Injury severity score)
Seven (3.7%) patients had an IS score of at least 16 representing severe polytraumatized patients. All of these patients did belong to age group III.
Location of injuries
The majority of the patients suffered from a whiplash injury (n = 165, 77.1%). Hereby, no specific damaged area of the cervical spine could be defined.
In the upper cervical spine (C0-2) 32 injuries were found (14.6%), while 49 (22.9%) were located at the subaxial cervical spine (Fig. 5).
Classification
Figure 6 shows the different injuries regarding the classifications. Table 1 shows the specific categorization of the atlantoaxial instabilities.
Subaxial type A fractures (according to the AO Spine Classification [23]) were seen in 10 cases (17%) and type B fractures in 10 cases (17%). Type C fractures were found in 6 patients (10.2%). All of these injuries occurred in patients of age group III (Fig. 6).
Neurological deficits
Neurological deficits were rarely found. According to the ASIA classification, 199 patients were classified grade E (92.9%), 6 patients were classified grade D (2.8%), 2 patients (0.9%) were classified grade C, and 2 patients (0.9%) were classified grade B (all in age Group III). Complete paraplegia (grade A) was documented in 6 patients (2.8%; group I: n = 2; group II: n = 1; group III: n = 3). With an increasing severity grade of the spinal injury, the degree of concomitant neurological deficit also rises (r = 0.351; p = 0.001). As expected, patients with neurological deficits demonstrated longer overall hospital stay (p = 0.001, r = 0.388).
Therapy
In the total cohort, 180 (84.1%) patients were treated conservatively, while 34 (15.8%) children received surgical treatment of overall 44 spinal injuries.
Surgical therapy was carried out using different approaches and stabilization techniques (Table 2).
Hospitalization
The mean hospital stay was 11.5 (r.: 1–180) days. Surgical therapy (p < 0.001), injury severity (p < 0.001), the presence of neurological deficits (r = 0.388; p < 0.001) as well as the presence of relevant concomitant injuries (p < 0.001) led to a significantly longer hospitalization period.
Complications
The majority of the patients showed no complications during the hospital stay (94.4%). Seven patients showed implant failure or complications related to surgery or a dislocation with the need of revision (23.5%). Two patients suffered from pneumonia. One 16-year old polytraumatized patient with a type II- odontoid fracture died 14 days following trauma due to severe head injury. A significant correlation was seen between accompanying injuries and pneumoniae occurrence (p = 0.001).
Discussion
The present multicenter study represents the largest patient cohort from German-speaking countries including 214 children with cervical spine injuries. Children of younger age were significantly more often affected at the upper cervical spine, while older children and adolescents did more often suffer from subaxial lesions. High and moderate impact injuries are the major trauma-inducing causes.
Above 80% of young patients presenting with cervical spinal column injuries were treated conservatively. In turn, surgery rarely had to be indicated and the performed surgical procedures were quite heterogeneous, partially reflecting a lack of standardization and missing algorithms.
The average age of the included patients in the current study was 11.9 years and thereby comparable to the results of Leonard et al. [13], while Platzer et al. [17] analyzed a younger cohort with an average age of 8.9 years. Very heterogeneous ratios, ranging from 0.6: 1 to 7.0: 1, are reported in the literature [15, 18], while in the present study a homogeneous gender distribution was found.
The main trauma mechanisms were shown to be age related. In the case of newborns, obstetric complications were the major contributing factor. In older ages falls from larger heights (> 1 m) did dominate. Like in our cohort high impact injuries, e.g., traffic accidents, are frequently described as a cause of cervical spine injuries [7].
There are also reports that around 19% of infants/toddlers suffered non-accidental trauma such as child abuse [16]. This could not be confirmed by our data, but according to a recent study, the incidence of child abuse in the presence of cervical spine injury is profoundly underestimated [2].
Upper cervical spine injuries are more common in the age of 0–8 years due to the unique anatomy of this population [21]. The overproportional large head size related to the rest of the body, the weak paraspinal muscles, lax ligaments, the horizontalization of the facet joints and anterior wedging of their vertebral bodies contribute to a higher likelihood of upper cervical trauma with a fulcrum of motion centered at C1 and C2. This constellation results in high torque and shear forces acting on C1 and C2, making this area more susceptible to injury. Furthermore, younger children with non-ossified synchondrosis of the dens axis are predisposed for injuries in this area due to asymmetry of the joint surfaces [14].
According to our data among adolescents’ sports and traffic accidents are the predominant cause of spinal column injuries, with motor sports injuries being the leading cause [5, 16, 20, 23].
Regarding to the literature, craniocerebral trauma and thoracic trauma are the most frequent concomitant injuries [12]. A total of 231 additional injuries were observed in this study with head injuries as the most common in 40% of the patients.
Depending on the underlying trauma mechanisms the occurrence of further spinal injuries in additional spinal localizations is quite high, with a combination of cervical and thoracic spine injuries, being the most common [17]. This could not be confirmed in the present study. Only one patient (0.93%) showed an additional spinal injury in another spinal segment. Combined injuries (multisegmental) of the cervical spine occurred in 8 patients. All of them had to undergo surgical therapy. Nevertheless only 99 (46.3%) patient received MRI; therefore, it is possible that there were more undetected injuries.
Analysis of the diagnostics showed that more than two-thirds of the children were exposed to radiation exposure induced by X-ray (80.4%).
CT imaging is recommended in the case of inadequate conventional imaging [21]. In our study, 34.6% of patients received a CT scan, in the surgical group even (91%; n = 34) for the purpose of preoperative planning.
While CT imaging is associated with higher specificities for identifying cervical spine injuries, most physicians are cautious about the use in a pediatric population due to the long-term risks of ionizing radiation [3]. Nevertheless, CT still seems to be indicated and remains the golden standard in cases of polytraumatized children. MRI, like a CT scan, presents with a high specificity in assessing cervical spine injuries. In contrast to the current literature the need of sedation was unexpectedly small (3.3%; n = 15) in our series [16].
The proportion of spinal column injuries in the growing age with accompanying neurological deficits in the literature presents with a wide range from 2.5% up to 35% [4, 18, 19].
Overall, neurological deficits in children are more common in cervical spine injuries, but are inconsistently reported in the literature. For example, only about 2–8% of all paraplegics affect children [23]. Neurological deficits were also rare in our own group of patients.
With a more severe spinal injury, the degree of neurological deficit rises (r = 0.351; p < 0.001). With a rising age, higher grades of neurological deficits were evident. Nevertheless, there might be an uncertain number of patients with lethal injuries and severe neurological deficits, who died before arrival in the emergency department.
Several studies have shown good recovery with incomplete lesions having the best prognosis [5, 15,220 23, 24]. This notion can be underlined by the results in this study since all incomplete neurological deficits did show an improvement during the hospital stay. Ribeiro et al. [19] demonstrated in 41% of their patients that complete or substantial recovery is possible after severe spinal cord injuries in children.
The main indication for surgical treatment in the literature is instability with and without neurological deficit. In the present cohort, 34 (15.8%) children underwent surgical treatment.
These results are comparable to a study published by Carreon et al. where 18% of children and adolescents underwent surgery [4].
Surgical therapy used for spinal fixation in the presented series was carried out using various surgical approaches and techniques.
As recommended in the literature [14], Halo fixation was used in 10 younger patients with instabilities of the upper cervical spine; in three patients, it was used initially until the definitive stabilization was performed.
Some authors raised concerns with the use of a Halo fixation regarding complications as pin site infections, dural penetration, pin loosening or supra orbital nerve injury [8, 17].
In the patients of the present study, pin loosening or loss of reduction was seen in 4 patients (40%).
As described in the literature, the operative therapy of adolescents in our cohort (age group III) is comparable to the operative therapy in adults [14].
The majority of the patients showed no complications in the inpatient stay (94.4%); a number of 8 patients showed implant failure or complications related to the operation or a dislocation with a revision surgery (3.7%). However, assuming the number of 34 operated children the percentage of complications remains relatively high (n = 8/34, 23.5%) underlining the complexity of these operations.
The present study has several limitations. The retrospective study design naturally limits the analysis, as an evaluation of the treatment results is not possible. Due to the rarity of the injuries, it was impossible to generate a sufficiently large number of cases to carry out reasonable statistical subgroup analyses of the individual injury levels, types of injury in relation to patient age.
Therefore, only a limited number of conclusions could be drawn about different diagnostic strategies, surgical indication, approaches and surgical techniques, the outcome and follow up, which influenced the recent published recommendation of the study group of this work [14].
Nevertheless, there is a lack of evidence-based standardized diagnostics and treatment algorithms, both nationally and internationally. Prospective data acquisition has to be recommended to overcome the described difficulties in order to develop consistent algorithms.
Conclusion
Cervical spine injuries in childhood affect girls and boys almost equally. In all age groups, falls and traffic accidents were the most common causes of cervical spine injuries. MRI plays an important role in the diagnostic work-up aside of conventional X-ray, functional X-ray and CT scans. Typical concomitant injuries were located at the head. Younger children majorly showed injuries of the upper cervical region, older children in the subaxial segments. Accompanying neurological deficits are rare and related to higher-graded spinal trauma reflecting severity of underlying trauma. The majority was treated conservatively. Nevertheless, 15% of the hospitalized children from the present multicenter study required surgical treatment with a still reasonable high number of complications.
References
Anderson LD, D’Alonzo RT (1974) Fractures of the odontoid process of the axis. J Bone Joint Surg Am 56:1663–1674
Baerg J, Thirumoorthi A, Hazboun R et al (2017) Cervical spine injuries in young children: pattern and outcomes in accidental versus inflicted trauma. J Surg Res 219:366–373
Baumann F, Ernstberger T, Neumann C, Nerlich M, Schroeder GD, Vaccaro AR et al (2015) Pediatric cervical spine injuries: a rare but challenging entity. J Spinal Disord Tech 28(7):377–384
Carreon LY, Glassman SD, Campbell MJ (2004) Pediatric spine fractures: a review of 137 hospital admissions. J Spinal Disord Tech 17:477–482
Chaudhry AS, Prince J, Sorrentino C, Fasanya C, McGinn J, Atanassov KD, Bloom S, Price M (2016) Identification of risk factors for cervical Spine injury from pediatric trauma registry. Pediatr Neurosurg 51(4):167–174. https://doi.org/10.1159/000444192. (Epub 2016 Mar 19 PMID: 26992002)
De Caffiniere JY, Seringe R, Roy-Camille R, Saillant G (1972) Physio-pathological study of severe ligament lesions in injuries of the spino-occipital joint. Rev Chir Orthop Reparatrice Appar Mot 58:11–19
Dietrich AM, Ginn-Pease ME, Bartkowski HM et al (1991) Pediatric cervical spine fractures: predominantly subtle presentation. J Pediatric Surg 26:995–999
Dogan S, Safavi-Abbasi S, Theodore N et al (2007) Thoracolumbar and sacral spinal injuries in children and adolescents: a review of 89 cases. J Neurosurg 106:426–433
Fielding JW, Hawkins RJ (1977) Atlanto-axial rotatory fixation. Fixed rotatory subluxation of the atlanto-axial joint. J Bone Joint Surg Am 59:37–44
Gehweiler JA, Osborne RL, Becker RF (1980) The radiology of vertebral trauma. W.B. Saunders Company, Philadelphia
Hasler RM, Exadaktylos AK, Bouamra O, Benneker LM, Clancy M, Sieber R, Zimmermann H, Lecky F (2011) Epidemiology and predictors of spinal injury in adult major trauma patients: European cohort study. Eur Spine J 20:2174–2180
Knox JB, Schneider JE, Cage JM et al (2014) Spine trauma in very young children: a retrospective study of 206 patients presenting to a level 1 pediatric trauma center. J Pediatr Orthop 34:698–702
Leonard JR, Jaffe DM, Kuppermann N, Olsen CS, Leonard JC (2014) Pediatric emergency care applied research network (PECARN) cervical spine study group. Pediatrics 133(5):e1179–e1188. https://doi.org/10.1542/peds.2013-3505. (Cervicalspineinjurypatternsinchildren PMID: 24777222)
Meinig H, Matschke S, Ruf M, Pitzen T, Disch A, Jarvers JS, Herren C, Weiß T, Jung MK, Rüther H, Welk T, Badke A, Gonschorek O, Heyde CE, Kandziora F, Knop C, Kobbe P, Scholz M, Siekmann H, Spiegl U, Strohm P, Strüwind C, Kreinest M (2020) Diagnostics and treatment of cervical spine trauma in pediatric patients: recommendations from the Pediatric Spinal Trauma Group. Unfallchirurg 123:252–268
Parent S, Mac-Thiong JM, Roy-Beaudry M, Sosa JF, Labelle H (2011) Spinal cord injury in the pediatric population: a systematic review of the literature. J Neurotrauma 28(8):1515–1524. https://doi.org/10.1089/neu.2009.1153. (Epub 2011 Jun 9. Review. PMID: 21501096)
Patel JC, Tepas JJ 3rd, Mollitt DL et al (2001) Pediatric cervical spine injuries: defining the disease. J Pediatr Surg 36:373–376
Platzer P, Jaindl M, Thalhammer G et al (2007) Cervical spine injuries in pediatric patients. J Trauma 62:389–396
Pieretti-Vanmarcke R, Velmahos GC, Nance ML et al (2009) Clinical clearance of the cervical spine in blunt trauma patients younger than 3 years: a multicenter study of the American Association for the Surgery of Trauma. J Trauma 67:543–549
Ribeiro Da Silva M, Linhares D, Cacho Rodrigues P et al (2016) Paediatric cervical spine injures. nineteen years experience of a single centre. Int Orthop 40:1111–1116
Ruffing T, Wiehmann M, Winkler H et al (2016) Xray of the thoracic and lumbar spine in injured children and adolescents : incidence, fracture rates and therapeutic consequences. Unfallchirurg 121:30
Schoneberg C, Schweiger B, Hussmann B et al (2013) Diagnosis of cervical spine injuries in children: a systematic review. Eur J Trauma Emerg Surg 39:653–665
Vaccaro AR, Koerner JD, Radcliff KE, Oner FC, Reinhold M, Schnake KJ, Kandziora F, Fehlings MG, Dvorak MF, Aarabi B, Rajasekaran S, Schroeder GD, Kepler CK, Vialle LR (2016) AOSpine subaxial cervical spine injury classification system. Eur Spine J 25(7):2173–2184. https://doi.org/10.1007/s00586-015-3831-3. (Epub 2015 Feb 26 PMID: 25716661)
Yang NP, Deng CY, Lee YH et al (2008) The incidence and characterisation of hospitalised acute spinal trauma in Taiwan–a population-based study. Injury 39:443–450
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jarvers, JS., Herren, C., Jung, M.K. et al. Pediatric cervical spine injuries—results of the German multicenter CHILDSPINE study. Eur Spine J 32, 1291–1299 (2023). https://doi.org/10.1007/s00586-023-07532-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07532-8