Abstract
Purpose
To report the clinical characteristics and surgical outcomes of scoliosis in patients with spinal muscular atrophy (SMA) from Mainland China.
Methods
Nineteen patients were retrospectively analyzed. Demographic, anthropometric and respiratory parameters were collected preoperatively. Surgical program was analyzed. Radiographic data were measured perioperatively. Motor status, ventilation support, sitting ability and respiratory symptoms were evaluated preoperatively and at final follow-up.
Results
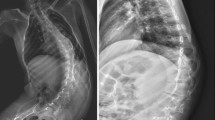
Age at surgery was 17.08 (12.83, 20.08) years. More than 40% of patients were diagnosed with low weight. Pulmonary dysfunction was observed in all patients. All patients received posterior spinal fusion (PSF). Sacroiliac fixation with sacral-2 alar iliac technique was used in 16 patients. Major curve correction rate was 54.87 ± 16.14%. Pelvic obliquity correction rate was 63.84 ± 23.70%. T1–T12 height, space-available-for-lung ratio and thoracic transverse diameter were increased (p < 0.001). Percentage of patients capable of sitting independently increased from 26.32% preoperatively to 73.68% at final follow-up. Cumulative scores of sitting-related items in muscular dystrophy spine questionnaire improved from 19.11 ± 5.40 preoperatively to 26.21 ± 5.20 at final follow-up. Total scores of symptomatic domains in St. George’s Respiratory Questionnaire decreased from 4 (2, 12) preoperatively to 1 (0, 3) at final follow-up.
Conclusions
SMA patients in China always present severe scoliosis at late adolescence, accompanied with high proportion of low weight and pulmonary dysfunction. PSF is effective for the correction of scoliosis and pelvic obliquity and the improvement of thoracic morphology. Sitting ability and respiratory symptoms were improved postoperatively.

Similar content being viewed by others
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Lefebvre S, Burglen L, Reboullet S, Clermont O, Burlet P, Viollet L, Benichou B, Cruaud C, Millasseau P, Zeviani M et al (1995) Identification and characterization of a spinal muscular atrophy-determining gene. Cell 80:155–165. https://doi.org/10.1016/0092-8674(95)90460-3
Wijngaarde CA, Brink RC, de Kort FAS, Stam M, Otto LAM, Asselman FL, Bartels B, van Eijk RPA, Sombroek J, Cuppen I, Verhoef M, van den Berg LH, Wadman RI, Castelein RM, van der Pol WL (2019) Natural course of scoliosis and lifetime risk of scoliosis surgery in spinal muscular atrophy. Neurology 93:e149–e158. https://doi.org/10.1212/WNL.0000000000007742
Schwentker EP, Gibson DA (1976) The orthopaedic aspects of spinal muscular atrophy. J Bone Joint Surg Am 58:32–38
Sponseller PD, Yang JS, Thompson GH, McCarthy RE, Emans JB, Skaggs DL, Asher MA, Yazici M, Poe-Kochert C, Kostial P, Akbarnia BA (2009) Pelvic fixation of growing rods: comparison of constructs. Spine 34:1706–1710. https://doi.org/10.1097/BRS.0b013e3181ab240e
Lorenz HM, Badwan B, Hecker MM, Tsaknakis K, Groenefeld K, Braunschweig L, Hell AK (2017) Magnetically controlled devices parallel to the spine in children with spinal muscular atrophy. JB JS Open Access 2:e0036. https://doi.org/10.2106/JBJS.OA.17.00036
Abol Oyoun N, Stuecker R (2014) Bilateral rib-to-pelvis Eiffel Tower VEPTR construct for children with neuromuscular scoliosis: a preliminary report. Spine J 14:1183–1191. https://doi.org/10.1016/j.spinee.2013.07.484
Daher YH, Lonstein JE, Winter RB, Bradford DS (1985) Spinal surgery in spinal muscular atrophy. J Pediatr Orthop 5:391–395. https://doi.org/10.1097/01241398-198507000-00001
Chang TL, Sponseller PD, Kebaish KM, Fishman EK (2009) Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine 34:436–440. https://doi.org/10.1097/BRS.0b013e318194128c
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, Muscaritoli M, Nyulasi I, Ockenga J, Schneider SM, MA de van der Schueren Singer P (2015) Diagnostic criteria for malnutrition: an ESPEN consensus statement. Clin Nutr 34:335–340. https://doi.org/10.1016/j.clnu.2015.03.001
Zong XN, Li H (2013) Construction of a new growth references for China based on urban Chinese children: comparison with the WHO growth standards. PLoS ONE 8:e59569. https://doi.org/10.1371/journal.pone.0059569
Young MF, Nguyen P, Tran LM, Avula R, Menon P (2020) A double edged sword? Improvements in economic conditions over a decade in India led to declines in undernutrition as well as increases in overweight among adolescents and women. J Nutr 150:364–372. https://doi.org/10.1093/jn/nxz251
Corona J, Sanders JO, Luhmann SJ, Diab M, Vitale MG (2012) Reliability of radiographic measures for infantile idiopathic scoliosis. J Bone Joint Surg Am 94:e86. https://doi.org/10.2106/JBJS.K.00311
Obikili EN, Okoye IJ (2006) Transverse thoracic diameter in frontal chest radiographs of an adult Nigerian population. West Afr J Med 25:186–189. https://doi.org/10.4314/wajm.v25i3.28275
Hell AK, Braunschweig L, Tsaknakis K, von Deimling U, Luders KA, Hecker M, Lorenz HM (2020) Children with spinal muscular atrophy with prior growth-friendly spinal implants have better results after definite spinal fusion in comparison to untreated patients. Neurosurgery 87:910–917. https://doi.org/10.1093/neuros/nyaa053
Gao Z, Sun X, Chen C, Teng Z, Xu B, Ma X, Wang Z, Yang Q (2021) Comparative radiological outcomes and complications of sacral-2-alar iliac screw versus iliac screw for sacropelvic fixation. Eur Spine J 30:2257–2270. https://doi.org/10.1007/s00586-021-06864-7
O’Brien JR, Yu W, Kaufman BE, Bucklen B, Salloum K, Khalil S, Gudipally M (2013) Biomechanical evaluation of S2 alar-iliac screws: effect of length and quad-cortical purchase as compared with iliac fixation. Spine 38:E1250-1255. https://doi.org/10.1097/BRS.0b013e31829e17ff
Jain A, Hassanzadeh H, Strike SA, Menga EN, Sponseller PD, Kebaish KM (2015) Pelvic fixation in adult and pediatric spine surgery: historical perspective, indications, and techniques: AAOS exhibit selection. J Bone Joint Surg Am 97:1521–1528. https://doi.org/10.2106/JBJS.O.00576
Perez A, Mulot R, Vardon G, Barois A, Gallego J (1996) Thoracoabdominal pattern of breathing in neuromuscular disorders. Chest 110:454–461. https://doi.org/10.1378/chest.110.2.454
Alhammoud A, Othman Y, El-Hawary R, Mackenzie WG, Howard JJ (2021) The impact of scoliosis surgery on pulmonary function in spinal muscular atrophy: a systematic review. Spine Deform 9:913–921. https://doi.org/10.1007/s43390-021-00302-w
Fauroux B, Griffon L, Amaddeo A, Stremler N, Mazenq J, Khirani S, Baravalle-Einaudi M (2020) Respiratory management of children with spinal muscular atrophy (SMA). Arch Pediatr 27:7S29-27S34. https://doi.org/10.1016/S0929-693X(20)30274-8
McElroy MJ, Shaner AC, Crawford TO, Thompson GH, Kadakia RV, Akbarnia BA, Skaggs DL, Emans JB, Sponseller PD (2011) Growing rods for scoliosis in spinal muscular atrophy: structural effects, complications, and hospital stays. Spine 36:1305–1311. https://doi.org/10.1097/BRS.0b013e3182194937
Lenhart RL, Youlo S, Schroth MK, Noonan KJ, McCarthy J, Mann D, Hetzel S, Sund SA, Halanski MA (2017) Radiographic and respiratory effects of growing rods in children with spinal muscular atrophy. J Pediatr Orthop 37:e500–e504. https://doi.org/10.1097/BPO.0000000000000867
Colombo L, Martini C, Bersanini C, Izzo F, Villafane JH, Berjano P, Lamartina C (2020) Effects of magnetically controlled growing rods surgery on pulmonary function in young subjects with spinal muscular atrophy type 2 and other neuromuscular scoliosis. J Neurosurg Sci 64:253–257. https://doi.org/10.23736/S0390-5616.17.04052-8
Swarup I, MacAlpine EM, Mayer OH, Lark RK, Smith JT, Vitale MG, Flynn JM, Anari JB, Pediatric Spine Study G, Cahill PJ (2021) Impact of growth friendly interventions on spine and pulmonary outcomes of patients with spinal muscular atrophy. Eur Spine J 30:768–774. https://doi.org/10.1007/s00586-020-06564-8
Holt JB, Dolan LA, Weinstein SL (2017) Outcomes of primary posterior spinal fusion for scoliosis in spinal muscular atrophy: clinical, radiographic, and pulmonary outcomes and complications. J Pediatr Orthop 37:e505–e511. https://doi.org/10.1097/BPO.0000000000001049
Acknowledgements
We thank Huanhuan Sha from Jiangsu Cancer Hospital for language editing.
Funding
This study was funded by the National Natural Science Foundation of China (Grant Numbers: 81974354, 81772424).
Author information
Authors and Affiliations
Contributions
WC and JS contributed to conceptualization and project administration; ZW was involved in data curation, formal analysis, visualization and writing—original draft; JS contributed to funding acquisition; YJ was involved in methodology; and EF, YJ, JL and JZ contributed to writing—review and editing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Written informed consents for the use of data and pictures were obtained from adult patients or legal guardians.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Z., Feng, E., Jiao, Y. et al. Surgical treatment of spinal deformities in spinal muscular atrophy: a single-center experience from China. Eur Spine J 31, 3089–3097 (2022). https://doi.org/10.1007/s00586-022-07347-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07347-z