Abstract
Background
Lung herniation is a rare condition, most often due to thoracic injury, but has also been described as a complication following cardiothoracic surgery. Here, we report two cases of post-surgical lung herniation following a neurosurgical mini-transthoracic (mini-TTA) for treatment of thoracic herniated discs. With this report we aim to make surgeons aware of this rare complication, review existing literature on surgical repairs and describe our novel correction technique using video assisted thoracic surgery (VATS) and a combination of mesh covering the muscle defect internally and nitinol rib plates for rib approximation on the outside of the thoracic cavity.
Case description
Patient A was an 85-year-old man who presented with a subcutaneous swelling at the site of surgery following a left sided mini-TTA. Computed tomography (CT) revealed pulmonary tissue herniation. He underwent VATS guided reconstruction. Using two Ventralex meshes covering the defect on the inside and a NiTi-rib H-plate for rib approximation.
Patient B was a 73-year-old woman who developed pulmonary complaints with a soft mass at the surgery site after a left sided mini-TTA. She also underwent VATS guided reconstruction. A large Sempramesh composite mesh and two NiTi-Rib H-plates were used. Recovery was uncomplicated and follow-up revealed no recurrence in both cases.
Conclusion
These cases should make surgeons aware of the possibility of post-surgical development of lung herniation and describe successful correction using a combination of mesh material and NiTi-Rib H-plates through a VATS technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung herniation is a rare and scarcely described entity in the literature, defined as expansion of pulmonary tissue beyond the pleural cavity through a chest wall defect. Most reports describe post traumatic lung herniation mostly as a late complication of thoracic trauma. However, lung herniation, is also described as a rare complication following cardiothoracic surgery.
We present 2 cases of post-surgical lung herniation, who underwent mini-transthoracic (mini-TTA) surgery for removal of thoracic herniated discs. Lung herniation as a complication following neurosurgical mini-TTA has not yet been described to our knowledge. We also describe our repairing surgical procedure using a combination of VATS intrathoracic mesh repair and a novel thoracic wall fixation technique with Niti-Rib plates (Nitinol Rib Clip, BIO DISTRIBUTION, Luxemburg) to compensate for the loss of intercostal muscle and widening of the intercostal space and we review the existing literature regarding surgical repair of lung herniation.
Case reports
Patient A was an 85-year-old man presenting with progressive weakness of both legs due to a massive non-calcified herniated disc at T10T11. In December 2019, the patient underwent a left sided mini-TTA with microscopic removal of the herniated disc. The procedure was complicated with minor cerebrospinal fluid leakage for which external lumbar drainage was performed. Postoperative course was uneventful, and the patient was discharged without neurological deficit.
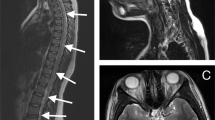
However, after 2 weeks the patient presented with a subcutaneous swelling at the site of the surgery, visible and palpable during coughing, suspected of a cerebrospinal fluid collection. Chest computed tomography (CT) scan revealed pulmonary tissue herniation through the chest wall at the intercostal level of the eighth-ninth rib and no signs of cerebrospinal fluid leakage (Fig. 1).
He underwent video assisted thoracic surgery (VATS) for reconstruction in a right lateral position. Cranially of the scar the defect in the eighth and ninth intercostal space was palpable. Inspection of the thoracic cavity showed the clearly visible defect and some adhesions of the dorsolateral wall (Fig. 2). The defect appeared to be larger than was expected based on the CT. We first inserted an 8 cm Ventralex mesh (Ventralex, Bard, Warwick RI, USA) this, however, left 6 cm of the defect uncovered. With a second overlapping 8 cm ventralex mesh the entire defect was covered. The two meshes were sutured to the thoracic wall. Since both meshes did not decrease the widened intercostal space or could prevent from further rib spreading, a nitinol H-plate was used to approximate the eighth and ninth rib together. Recovery was uncomplicated, and he was discharged on the fifth postoperative day. Follow-up of over one year in the outpatient clinic revealed no complaints or recurrence of lung herniation or widening of the intercostal space on thoracic X-ray. (Figs. 3 and 4).
Patient B was a 73-year-old woman presenting with leg weakness due to a large medially located non-calcified herniated disc at T10T11. In 2019, an uncomplicated left sided mini-transthoracic approach (mini-TTA) was performed. The postoperative course was uneventful, with the patient walking independently after two months.
However, 3 months after surgery, she developed pulmonary complaints with a soft mass at the site of the scar tissue during coughing and Valsalva maneuver. She presented with these complaints at the general surgery department in February 2020. Physical examination revealed an 8 cm, flexible and spontaneously reponable bulging. The actual thoracic wall defect was not easily palpable.
She underwent video assisted thoracic surgery (VATS) for reconstruction of the right dorsolateral thoracic wall in the ninth intercostal space in a left lateral position. Inspection of the thoracic cavity revealed a large defect (over 10 cm in length) without any intercostal muscle or fascia in the eighth intercostal space and multiple adhesions for which adhesiolysis was performed. We placed a 20 × 10 Sempramesh composite mesh (Sempramesh, Bard, Warwick RI, USA), with 6-point percutaneous suture fixation to the parietal pleura on the inside of the thoracic cavity. To decrease the widened intercostal space and decrease stress on the mesh during coughing and Valsalva, 2 × NiTi-Rib H-plates 20 were placed over the eighth intercostal space defect over the eighth and ninth rib.
Recovery was uncomplicated and she was discharged on the fifth postoperative day, relieved of her symptoms. Follow-up of over one year in the outpatient clinic revealed no complaints or recurrence of lung herniation and good positioning of the NiTi-Rib plates on thoracic X-ray.(Fig. 5, 6, 7, 8, 9).
Discussion
Lung herniation is a rare condition and was first described in 1499, with about 300 cases being published since [1]. Most literature consists of case reports, the majority describing post traumatic lung herniation. Postoperative lung herniation is a known but rare complication after cardiopulmonary thoracic surgery. Since the introduction of minimal invasive video assisted thoracoscopic surgery (VATS) procedures, intercostal lung herniation has been documented more often [2].
To our knowledge, lung herniation as a complication of mini-TTA thoracic disc surgery has not been described yet. Our 2 patients are the first cases in the literature and should make surgeons aware of the possible development of lung herniation whenever patients present with postoperative pulmonary complaints.
However, the main issue of postoperative lung herniation is prevention when possible. At the end of the primary procedure, surgeons should focus on repositioning the adjacent ribs with a suture through the cranial and caudal rib followed by reconstruction of the intercostal muscle, when possible. Once a lung herniation has developed, it can be successfully treated by minimal invasive surgery using (part of) the existing scar and one or two small extra video ports.
Literature has described different techniques of surgical repair of lung herniation which can be roughly categorized in 3 groups: primary closure of the defect, repair using periosteal flaps, and third, the use of synthetic materials [3].
Primary closure using VATS was performed for a post traumatic lung herniation where the herniated lung was reduced, and the defect was approximated and sutured [4]. Alternatively, the defect can be repaired using muscular fascia. For larger defects, mesh repair may be required [5].
The repair technique using periosteal flaps was first described in 1933 and was revisited in four cases of traumatic lung hernia. The pleura was closed with sutures, then approximated the superior and inferior flaps, bridging the gap between the ribs. For further stabilization the lower ribs were approximated with absorbable sutures [6] or stainless-steel wires [7].
Most articles describe the use of synthetic materials for the surgical repair of a lung hernia by VATS, similar to repairing an inguinal hernia with a mesh covering the defect. In case of acquired lung hernia occurring through an old anterior thoracotomy scar, VATS was performed through the old scar, and the lung hernia was reduced with dissections and the defect repaired with a Prolene mesh attached with a hernia stapler [8,9,10,11,12]. Alternatively, the mesh can be stabilized by two titanium plates on the ribs [13,14,15]. Other techniques combined synthetic materials with rib reapprochement by suturing [3, 16]. Based on the existing literature, mesh appears to be a safe and successful method of surgical repairment of lung herniations.
Due to the rare occurrence of lung herniation, there is not one preferable method for the repair of lung hernias. All published studies described successful repair techniques, however, with possible publication bias and lack of RCT’s, no evidence-based conclusion can be made. Primary closure and periosteal flaps seem to be sufficient for smaller defects, whereas repair with synthetic materials might be preferred for larger defects [3].
In the presented case reports, we described an alternate surgical technique combining minimal invasive VATS mesh repair and rib fixation. Due to the larger defects and the more lateral location following the mini-TTA procedure, we reapproximated and stabilized the ribs with a NiTi-Rib H-plate. Consequently, the widening of the intercostal space was reduced, and the ribs were secured to prevent displacement of the mesh.
In summary, intercostal lung herniation is a rare complication of a mini-TTA procedure for herniated discs. Based on our 2 cases, intercostal lung herniation can successfully be corrected using mesh material through a VATS technique. For larger defects with intercostal space widening, we recommend additional rib fixation with NiTi-Rib H-plates.
References
Roland J. [1499] De Pulmonis Sanarpot. Liber III (cap) XXV. In: De Chavliae G. Cyrugia. p144
Batıhan, G., Yaldız, D., & Ceylan, K. C. [2020]. A rare complication of video-assisted thoracoscopic surgery: lung herniation retrospective case series of three patients and review of the literature. Wideochirurgia i inne techniki maloinwazyjne = Videosurgery and other miniinvasive techniques, 15(1), 215–219. https://doi.org/10.5114/wiitm.2019.87937
Haro A, Komiya K, Taguchi Y, Nishikawa H, Kouda T, Fujishita T, Yokoyama H (2017) A rare case of an intercostal lung herniation with fractures of the fifth and sixth ribs after thoracic surgery. Int J Surg Case Rep 41:473–476. https://doi.org/10.1016/j.ijscr.2017.11.028
Reardon Michael J, Fabré Jan, Reardon Patrick R, Baldwin John C (1998) Video-assisted repair of a traumatic intercostal pulmonary hernia. Annals Thoracic Surg. 65(4):1155–1157. https://doi.org/10.1016/S0003-4975(98)00035-6
Fine J, Walters BS, Agnoni AA, Coppola CP, Scorpio RJ, Kennedy AP (2014) Pulmonary hernia in a two-year-old child. Case reports in surgery 2014:792376. https://doi.org/10.1155/2014/792376
Saiedi H, Bustangi N, Drevet G, Tronc F (2019) Periosteal flap repair for traumatic lung hernia. an old technique revisited. J Trauma Acute Care Surg. 86(3):551–553. https://doi.org/10.1097/TA.0000000000002154
Smith AT, Jamplis RW (1972) Lung hernia: a technic for repair. Ann Surg 176(6):711–712. https://doi.org/10.1097/00000658-197212000-00005
W.T. Brown, M. Hauser, and F.A. Keller. [1996] Hernia of the Lung Repaired by VATS: A Case Report. J Laparoendoscopic Surg. 427–430. Published Online: 14 Apr 2009. https://doi.org/10.1089/lps.1996.6.427
Deeik RK, Memon MA, Sugimoto JT (1998) Lung herniation secondary to minimally invasive direct coronary artery bypass grafting. Ann Thorac Surg 65(6):1772–1774. https://doi.org/10.1016/s0003-4975(98)00242-2 (PMID: 9647101)
Fazi AC, Davis ML, Kurian S, McClellan WT (2017) Acquires anterior thoracic lung herniation and repair: a rare case and discussion. W V Med J 113(1):40–42 (PMID: 29373004)
Hebra A, Cina R, Streck C (2011) [2011] Video-assisted thoracoscopic repair of a lung hernia in a child. J Laparoendosc Adv Surg Tech A 21(8):763–765. https://doi.org/10.1089/lap.2011.0147
Santini M, Fiorello A, Vicidomini G, Busiello L (2009) Pulmonary hernia secondary to limited access for mitral valve surgery and repaired by video thoracoscopic surgery. Interact Cardiovasc Thorac Surg 8(1):111–113. https://doi.org/10.1510/icvts.2008.190744
Subotic D, Wiese M, Hojski A, Lardinois D (2019) Surgical repair of the postoperative Lung Hernia by combining mesh interposition and chest wall stabilization by using synthes plates: a novel technique. Case Rep Surg 7(2019):2107083. https://doi.org/10.1155/2019/2107083
Akkas Y, Peri NG, Kocer B, Kaplan T (2016) Repair of lung herniation with titanium prosthetic ribs and Prolene mesh. Asian Cardiovasc Thorac Ann 24(3):280–282. https://doi.org/10.1177/0218492315619509
Wcisło, S., Wawrzycki, M., Misiak, P., & Brocki, M. [2015] A new technique of pulmonary hernia surgical repair using intramedullary titanium implants. Kardiochirurgia i torakochirurgia polska = Polish journal of cardio-thoracic surgery, 12(1), 26–29. https://doi.org/10.5114/kitp.2015.50564
Cafarotti S, Matarrelli E, Guerra A, Dutly AE (2014) Large intercostal pulmonary hernia secondary to limited-access aortic valve surgery: video-assisted thoracoscopic technique repair. Lung 192(2):333–334. https://doi.org/10.1007/s00408-013-9538-5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
De Vries, S.E.N., Arts, M.P. & Van Huijstee, P.J. Intercostal lung herniation; a rare complication after mini-transthoracic approach (TTA) for thoracic disc herniation. Two case reports and review of literature. Eur Spine J 31, 3708–3712 (2022). https://doi.org/10.1007/s00586-021-07023-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-07023-8