Abstract
Purpose
To determine the variation in the global treatment practices for subaxial unilateral cervical spine facet fractures based on surgeon experience, practice setting, and surgical subspecialty.
Methods
A survey was sent to 272 members of the AO Spine Subaxial Injury Classification System Validation Group worldwide. Questions surveyed surgeon preferences with regard to diagnostic work-up and treatment of fracture types F1–F3, according to the AO Spine Subaxial Cervical Spine Injury Classification System, with various associated neurologic injuries.
Results
A total of 161 responses were received. Academic surgeons use the facet portion of the AO Spine classification system less frequently (61.6%) compared to hospital-employed and private practice surgeons (81.1% and 81.8%, respectively) (p = 0.029). The overall consensus was in favor of operative treatment for any facet fracture with radicular symptoms (N2) and for any fractures categorized as F2N2 and above. For F3N0 fractures, significantly less surgeons from Africa/Asia/Middle East (49%) and Europe (59.2%) chose operative treatment than from North/Latin/South America (74.1%) (p = 0.025). For F3N1 fractures, significantly less surgeons from Africa/Asia/Middle East (52%) and Europe (63.3%) recommended operative treatment than from North/Latin/South America (84.5%) (p = 0.001). More than 95% of surgeons included CT in their work-up of facet fractures, regardless of the type. No statistically significant differences were seen in the need for MRI to decide treatment.
Conclusion
Considerable agreement exists between surgeon preferences with regard to unilateral facet fracture management with few exceptions. F2N2 fracture subtypes and subtypes with radiculopathy (N2) appear to be the threshold for operative treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The AO Spine Knowledge Forum, a group of international academic surgeons with special interest in trauma classifications for international acceptance and reproducibility, developed a comprehensive classification system for subaxial cervical spine injuries [1,2,3,4,5]. The AO Spine Subaxial Cervical Spine Injury Classification System (AO Spine SCICS) utilizes a clear morphologic framework to guide and standardize patient management based on four major criteria: (1) fracture morphology, (2) facet injury, (3) neurologic status, and (4) case-specific modifiers (Supplementary Digital Content 1) [6]. Within the hierarchical classification system, facet injuries are categorized into four subtypes: F1—nondisplaced facet fractures, F2—facet fractures with potential for instability, F3—floating lateral mass fractures, and F4—subluxated or dislocated facet (Fig. 1). The neurologic status of the patient is defined by the N descriptor: N0—neurologically intact, N1—transient neurologic deficit, N2—radicular symptoms, N3—incomplete cord injury or cauda equina, and N4—complete cord injury. This classification scheme has demonstrated adequate interobserver agreement and intra-observer reproducibility in multiple studies [1, 5, 7,8,9]. Even with an ideal classification scheme, significant heterogeneity remains with regard to the work-up and treatment of subaxial unilateral facet fractures [10,11,12,13,14,15].
Management of isolated subaxial facet fractures currently lies at the discretion of the surgeon. This may be due in part to its rarity, given that unilateral facet fractures without associated compression, tension band, or translations injuries represent approximately 6% of all cervical injuries, and also due to the significant variation in the morphologic presentation of facet injuries [16, 17]. The facet joint and capsule play an important role in subaxial stability, limiting rotational and linear translation during physiologic motion to protect the underlying neural elements [18]. Despite unilateral facet fractures not meeting the conventional criteria for instability [12, 19], anywhere between 21 and 80% of these fractures fail nonoperative management leading to pain, deformity, and even secondary neurologic deficits [20, 21]. This disparity in outcomes has resulted in a lack of consensus-based algorithms for deciding between operative and nonoperative treatments. Within that, the type of immobilization and surgical approach used for nonoperative and operative management, respectively, is a matter of surgeon preference and experience [10, 14, 19, 21,22,23,24,25]. Computed tomography (CT)- and magnetic resonance imaging (MRI)-based criteria for classifying and predicting failure have also been investigated, but controversy ensues regarding the imaging necessary to appropriately work-up facet fractures [12, 20]. All these factors have contributed to the lack of standardization in the treatment for unilateral facet fractures.
Given the present uncertainty, it is important to understand the effects of regional bias on the treatment for facet fractures and elucidate what surgeon characteristics influence treatment preferences. For one, diversity among international practice patterns may result in a discrepancy between operative and nonoperative management [26]. Additionally, surgeon experience, practice setting, and subspecialty training all have implications on treatment decisions and serve as a potential source of heterogenicity in management [27]. The primary goal of this study is to determine the global management of facet fractures and variables that affect treatment.
Methods
A 22-question survey (Supplemental Digital Content 2) including surgeon demographics and treatment preferences for nine clinical vignettes consisting of unilateral facet fractures was sent to the members of the AO Spine Subaxial Injury Classification System Validation Group. Surgeon demographics included years of experience (< 5, 5–10, 11–20, > 20), surgical subspecialty (Orthopedic Spine, Neurosurgery Spine, Other), region (North/Latin/South America, Europe, Africa/Asia/Middle East), and practice setting (academic, hospital-employed, private practice). Academic practice setting is defined by significant time dedicated to patient care, research, and education of medical trainees while hospital-employment is defined by focus only on patient care. Both academicians and hospital-employed surgeons are employees of the hospital, in contrast to private practitioners. These spine surgeons represent six world regions: North America, Latin and South America, Europe, Africa, Asia, and the Middle East. Clinical vignettes consisted of fracture types F1–F3 with various associated neurologic injuries (N0–N2). Given F4 injuries are a sign of severe disruption of the posterior tension band, they were not included in the survey as they are an indicator of instability for which surgery is recommended. Questions surveyed surgeon preferences with regard to diagnostic work-up and treatment. Some questions allowed for the possibility of multiple answer choices from the respondent. Only surveys containing complete demographic information and at least one valid answer to the clinical vignettes were analyzed.
Descriptive statistical analysis was performed for categorical and continuous data. For categorical data, frequencies were calculated based on the number of nonmissing replies. Continuous data were analyzed using median and interquartile range (IQR). Regional variations were compared between surgeons from North/Latin/South America combined, Africa/Asia/Middle East combined, and Europe. Geographic regions were combined due to low number of participants from the designated region. Differences in the treatment algorithm were analyzed by Chi-square test or Fisher’s exact test. The significance level was defined at α = 0.05. All analysis was performed using the statistical software SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
A total of 272 surgeons were surveyed with 161 (59.2%) surgeons responding. A summary of surgeon demographics is presented in Table 1. The median number of spine trauma patients treated per year per surgeon was 50 (IQR 20-100). “Surgeon variation” will refer to the differences among surgeon respondents with regard to years of experience (< 5, 5–10, 11–20, > 20), surgical subspecialty (Orthopedic Spine, Neurosurgery Spine, Other), region (North/Latin/South America, Europe, Africa/Asia/Middle East), and practice setting (academic, hospital-employed, private practice). Academic practice setting includes significant time dedicated to patient care, research, and education of medical trainees, while hospital employment focuses mainly on patient care. Both academicians and hospital-employed surgeons are employees of the hospital, in contrast to private practitioners.
Preferred subaxial spine classification system
The preferred subaxial spine injury classification system for all respondents was as follows: AO Spine SCICS 71.9%, Subaxial Cervical Spine Injury Classification system (SLIC) 18.1%, and Magerl system 2.5%. Of respondents, 7.5% do not routinely use a classification system (Table 2). The AO Spine SCICS is used by the majority of respondents from all world regions except for North America, where it is used by 47.1% of surgeons and the SLIC system is used by 41.2% of surgeons (Supplemental Table 1). Academicians used the AO Spine SCICS less frequently (64.6%) compared to hospital-employed and private practice surgeons (75.4% and 87.5%, respectively) (p = 0.304). There were no statistically significant differences in the preferred subaxial cervical injury classification system based on surgeon variation.
Use of AO spine facet fracture classification system
Overall, 106 (71.6%) respondents regularly use the facet portion of the AO Spine SCICS. Significantly fewer academic respondents (61.6%) used this portion of the classification system than did hospital-employed and private practice surgeons (81.1% and 81.8%, respectively) (p = 0.029) (Table 2). There was no significant difference in the use of the facet portion of the AO Spine SCICS when grouping raters by years of experience, surgical subspecialty, or by region. Ungrouped summary of the preferred subaxial classification system and use of the facet portion of the AO Spine SCICS is presented in Supplemental Table 1.
Operative versus nonoperative management
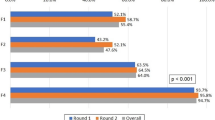
Respondent preferences for initial management strategy regarding facet fracture subtypes with various degrees of neurologic injury are presented in Table 3. For all clinical scenarios, there was no statistically significant difference in management choice based on surgeon experience or practice setting (Table 4). When evaluated by subspecialty, the only significant difference in treatment was for F1N1 fractures where neurosurgeons were more likely to recommend surgical treatment than orthopedic spine surgeons, 20.8% vs 7.0%, respectively (p = 0.012). When evaluated by region, there was only a significant difference in management of floating lateral mass fractures, specifically F3N0 and F3N1 fractures. For F3N0 fractures, 74.1%, 59.2%, and 49.0% of North/Latin/South America, Europe, and Africa/Asia/Middle East respondents chose operative treatment, respectively (p = 0.025). And while the majority agreed on operative treatment for F3N1 fractures, significantly less surgeons from Africa/Asia/Middle East (52.0%) and Europe (63.3%) recommended surgery than respondents from North/Latin/South America (84.5%) (p = 0.001). Ungrouped summary of operative versus nonoperative management preferences for facet fracture subtypes is presented in Supplemental Table 2.
Preferred type of operative/nonoperative management
For the preferred type of operative and nonoperative management, not all participants had the possibility of answering the question depending on their response to the overlying question of operative vs nonoperative management. As a result, no statistical comparisons could be performed due to conditional probability. Ungrouped summary of the preferred nonoperative and operative method of management for fracture subtypes is presented in Supplemental Tables 3 and 4, respectively.
Preferred imaging in work-up and treatment
Summary of imaging modalities used in the work-up of F1, F2, and F3 fractures is presented in Table 5. More than 95.7% of surgeons routinely use CT imaging regardless of facet fracture subtype. Comparison of the need for MRI in the decision between operative and nonoperative treatment is presented in Table 6. There was no statistically significant difference in the use of MRI for decision making for facet fracture subtypes based on surgeon variation, with a stepwise increase in the use of MRI for F1–F3 fractures (42.2–68.7%).
Discussion
The AO Spine SCICS remains the most widely used classification system among surgeons worldwide. The SLIC system remains the next most frequently used overall with a higher frequency of use by North American surgeons (41.2%). Due to the number of respondents, North American, Latin American, and South American surgeons were grouped together for statistical analysis. Because only 9.8% of Latin and South American surgeons use the SLIC system, this regional grouping attenuated any statistically significant differences in classification system preferences by region. Albeit not statistically significant, less experienced surgeons (< 5 years of training) were noted to use the AO Spine SCICS more frequently (82.1%) compared to the remainder of surgeons (69.7%). The newer AO Spine SCICS was published in 2015, meaning less experienced surgeons likely learned the AO Spine SCICS during their training [1]. Those surgeons with training > 5 years have likely adapted to the respective classification system learned during their training. The same can be said for the use of the facet portion of the AO Spine SCICS, with only 69.7% of surgeons with > 5 years of experience using the facet portion compared to 80.8% of surgeons with < 5 years of experience. Interestingly, academic surgeons used the facet portion of the AO Spine SCICS significantly less than hospital-employed or private practice surgeons. Given that the classification system is used to help reliably classify and communicate fractures for both research and clinical purposes, one would expect greater use among academicians. This could be explained by academic surgeons using the SLIC system more frequently as noted previously, which does not incorporate a facet scoring system.
The AO Spine SCICS is a hierarchical system in which each morphologic type is subdivided into increasing numerical subtypes based on the energy of injury, with higher numbers inferring increased injury severity. The benefits of such a hierarchical system tie into the development of treatment algorithms, in that there may be a line drawn after a particular subtype where fractures are deemed unanimously unsuitable for nonoperative management. When evaluating surgeon preferences for operative versus nonoperative management from around the world, F2N2 fractures appear to draw that threshold. The majority of surgeons surveyed agree that any fracture classified as F2N2 or above should be treated surgically. Additionally, all fractures with radiculopathy (N2), regardless of subtype, also indicate operative treatment for the majority of surgeons. Some regional exceptions exist, however, with surgeons from Africa/Asia/Middle East significantly less likely to recommend surgical treatment for F3N0 fractures than surgeons from the remainder of global regions. This may be secondary to limited resources and infrastructure—reserving surgery for more severe cases, patient socioeconomic factors, as well as cultural differences in patient expectations and outcomes in that particular region [28,29,30,31]. Interestingly, while the treatment for F2N0 fractures is highly controversial in the scientific literature, 73.4% of surgeons recommended nonoperative care, with no significant region or experiential variation [14, 20, 32].
The preferred nonoperative treatment by the majority of respondents is the placement of a hard cervical collar irrespective of fracture subtype. Less than 10% of all respondents, regardless of surgeon variation, preferred treatment without a collar or with a soft collar, underscoring the importance of immobilization. The preference for treatment of patients in a halo increased for F3N0 fractures and above (i.e., F3N1, F3N2); however, a hard collar is still preferred by the majority of surgeons surveyed. Both anterior and posterior approaches have been shown to be successful in the surgical management of facet fractures which explains the variation found in the preferred approach [14, 19, 22,23,24,25]. However, combined anterior and posterior treatment for facet fractures was the least preferred approach regardless of subtype.
Although multiple imaging modalities were allowed to be chosen by respondents, CT scans were the preferred option for over 95% of surgeons, whereas flexion/extension radiographs were preferred in less than 30% of all cases. CT remains the standard for the work-up of cervical spine trauma, providing significant detail of fracture morphology not seen in plain radiographs [33, 34]. Non-displaced unilateral facet fractures do not meet physiologic criteria for instability and therefore would not be detected on flexion/extension radiographs. Thus, it seems flexion/extension radiography may not provide additional information that would help guide management. The majority of surgeons felt that MRI was necessary to decide the treatment for F2 and F3 fractures. While 57.8% surgeons with > 20 years of experience also noted the need for MRI in F1 fractures, the majority of all lesser experienced surgeons felt it was unnecessary. This may highlight generational differences in training and more recent advancements in multidetector CT technology negating the need for MRI in lower energy injuries [35].
While it was demonstrated that the majority of surgeons from around the world agree in the management of unilateral facet fractures, this study is not without limitations. While the response rate of our survey is 59%, the demographic percentages of AO Spine membership are proportionate to our study’s respondent profiles underscoring low nonresponse bias. The study design, however, provides a small sample of surgeons with uneven numbers across geographic regions. Limited participation by some world regions required grouping by proximity for statistical analysis. The differences in preferences between operative and nonoperative treatment among North, South, and Latin America, for example, may have been muddled as a result of grouping them together. Moreover, the regional variability in available equipment and resources may confound management preferences [36, 37]. Furthermore, study participants were all members of AO Spine and may not represent a true cross section of surgeons globally. Surgeon practice setting for respondents suggests a participation bias toward academic and hospital-employed surgeons, which would be expected for members of an academic global community. Accordingly, use of the AO Subaxial Classification system may be overrepresented in this population. Additionally, it may also be suggested that surgeons of the same academic community may be more likely to agree with one another regarding treatment practices. Lastly, there were a higher proportion of orthopedic spine surgeon respondents compared to neurosurgery spine respondents, which is suboptimal in a surgical survey. With the exception of F1N1 fractures however, management practices were similar between both groups, as has been demonstrated in management of spinal trauma between orthopedic and neurosurgery spine surgeons [27, 38].
Conclusion
To our knowledge, this is the first study to evaluate global variation in the treatment for unilateral subaxial facet fractures. While not unanimous, our results find agreement between the majority of surgeons within most practice management clinical vignettes with few significant differences based on surgeon variation. Most notable was the observation that F2N2 fracture subtypes and subtypes with radiculopathy (N2) appear to be the threshold for operative management. Further research should focus on clinical outcomes assessments based upon treatment modality in order to develop international guidelines to reduce practice variety and offer patients the optimal care.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Vaccaro AR et al (2016) AOSpine subaxial cervical spine injury classification system. Eur Spine J 25:2173–2184
Schroeder GD et al (2015) A worldwide analysis of the reliability and perceived importance of an injury to the posterior ligamentous complex in AO type A fractures. Global Spine J 5:378–382
Aarabi B, Oner C, Vaccaro AR, Schroeder GD, Akhtar-Danesh N (2017) Application of AOSpine subaxial cervical spine injury classification in simple and complex cases. J Orthop Trauma 31(Suppl 4):S24–S32
Vaněk P (2018) New AOSpine subaxial cervical spine injury classification and its clinical usage. Rozhledy V Chir Mesicnik Ceskoslovenske Chir Spolecnosti 97:273–278
Schnake KJ, Schroeder GD, Vaccaro AR, Oner C (2017) AOSpine classification systems (Subaxial, Thoracolumbar). J Orthop Trauma 31:S14–S23
Divi SN et al (2019) AOSpine—spine trauma classification system: the value of modifiers: a narrative review with commentary on evolving descriptive principles. Global Spine J 9:77S-88S
Urrutia J et al (2016) A comparative agreement evaluation of two subaxial cervical spine injury classification systems: the AOSpine and the Allen and Ferguson schemes. Eur Spine J 25:2185–2192
da Silva OT et al (2016) Evaluation of the reliability and validity of the newer AOSpine subaxial cervical injury classification (C-3 to C-7). J Neurosurg Spine 25:303–308
Urrutia J et al (2017) An Independent Inter- and Intraobserver Agreement Evaluation of the AOSpine Subaxial Cervical Spine Injury Classification System. Spine 42:298–303
Pehler S et al (2018) Clinical outcomes of cervical facet fractures treated nonoperatively with hard collar or halo immobilization. Global Spine J 9:48–54
Vedantam A, Fridley JS, Navarro JC, Gopinath SP (2017) Management of acute unilateral nondisplaced subaxial cervical facet fractures. Oper Neurosurg 14:104–111
Halliday AL, Henderson BR, Hart BL, Benzel EC (1997) The management of unilateral lateral mass/facet fractures of the subaxial cervical spine. Spine 22:2614–2621
Khezri N, Ailon T, Kwon BK (2016) Treatment of facet injuries in the cervical spine. Neurosurg Clin N Am 28:125–137
Kepler CK et al (2016) Treatment of isolated cervical facet fractures: a systematic review. J Neurosurg Spine 24:347–354
Dvorak M, Vaccaro AR, Hermsmeyer J, Norvell DC (2010) Unilateral facet dislocations: Is surgery really the preferred option? Evidence-based Spine-care J 1:57–65
Hadley MN, Fitzpatrick BC, Sonntag VK, Browner CM (1992) Facet fracture-dislocation injuries of the cervical spine. Neurosurgery 30:661–666
Lowery DW et al (2001) Epidemiology of cervical spine injury victims. Ann Emerg Med 38:12–16
White AA et al (1975) Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop Relat R 109:85–96
Beyer CA, Cabanela ME (1992) Unilateral facet dislocations and fracture-dislocations of the cervical spine: a review. Orthopedics 15:311–315
Spector LR et al (2006) Use of computed tomography to predict failure of nonoperative treatment of unilateral facet fractures of the cervical spine. Spine 31:2827–2835
Lee S-H, Sung J-K (2009) Unilateral lateral mass-facet fractures with rotational instability: new classification and a review of 39 cases treated conservatively and with single segment anterior fusion. J Trauma Inj Infect Critical Care 66:758–767
Chaput C et al (2018) Anterior fixation of floating facet fractures in the cervical spine: a prospective case series and biomechanical analysis. Int J Spine Surg 12:85–91
Kotani Y, Abumi K, Ito M, Minami A (2004) Cervical spine injuries associated with lateral mass and facet joint fractures: new classification and surgical treatment with pedicle screw fixation. Eur Spine J 14:69–77
Koh YD, Lim T-H, You JW, Eck J, An HS (2001) A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine 26:15–21
Anderson PA, Henley MB, Grady MS, Montesano PX, Winn HR (1991) Posterior cervical arthrodesis with ao reconstruction plates and bone graft. Spine 16:S72–S79
Gadjradj PS et al (2017) Management of symptomatic lumbar disk herniation: an international perspective. Spine 42:1826–1834
Grauer JN et al (2004) Similarities and differences in the treatment of spine trauma between surgical specialties and location of practice. Spine 29:685–696
Magogo J et al (2020) Operative treatment of traumatic spinal injuries in tanzania: surgical management, neurologic outcomes, and time to surgery. Global Spine J. https://doi.org/10.1177/2192568219894956
Aleem IS et al (2017) The burden of spine fractures in India. Global Spine J 7:325–333
Leidinger A et al (2019) Spinal trauma in Tanzania: current management and outcomes. J Neurosurg Spine 31:103–111
Lessing NL et al (2020) Nonoperative treatment of traumatic spinal injuries in Tanzania: Who is not undergoing surgery and why? Spinal Cord. https://doi.org/10.1038/s41393-020-0474-y
Aarabi B et al (2014) Comparative effectiveness of surgical versus nonoperative management of unilateral, nondisplaced, subaxial cervical spine facet fractures without evidence of spinal cord injury: clinical article. J Neurosurg Spine 20:270–277
Munera F, Rivas LA, Nunez DB Jr, Quencer RM (2012) Imaging evaluation of adult spinal injuries: emphasis on multidetector CT in cervical spine trauma. Radiology 263(3):645–660
Platzer P et al (2006) Clearing the cervical spine in critically injured patients: a comprehensive C-spine protocol to avoid unnecessary delays in diagnosis. Eur Spine J 15:1801–1810
Ginat DT, Gupta R (2014) Advances in computed tomography imaging technology. Biomed Eng 16:431–453
Karekezi C et al (2020) The impact of African-trained neurosurgeons on sub-Saharan Africa. Neurosurg Focus 48:E4
Volpi G (2016) Radiography of diagnostic imaging in Latin America. Nucl Medicine Biomed Imaging 1:10–12
Canseco JA et al (2020) Regional and experiential differences in surgeon preference for the treatment of cervical facet injuries: a case study survey with the AO Spine Cervical Classification Validation Group. Eur Spine J. https://doi.org/10.1007/s00586-020-06535-z
Acknowledgements
This study was organized and funded by AO Spine through the AO Spine Knowledge Forum Trauma, a focused group of international trauma experts. AO Spine is a clinical division of the AO Foundation, which is an independent medically guided not-for-profit organization. Study support was provided directly through the AO Spine Research Department. The authors would like to thank Olesja Hazenbiller (AO Spine) for her editorial and administrative assistance and Christian Knoll (AO Innovation Translation Center, Clinical Evidence) for his support with statistical analysis.
Funding
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Author information
Authors and Affiliations
Consortia
Contributions
All authors significantly contributed to the document and have reviewed the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the Institutional Review Board at the Thomas Jefferson University Hospital. Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Karamian, B.A., Schroeder, G.D., Holas, M. et al. Variation in global treatment for subaxial cervical spine isolated unilateral facet fractures. Eur Spine J 30, 1635–1650 (2021). https://doi.org/10.1007/s00586-021-06818-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06818-z