Abstract
Purpose
Although signal intensity on T2W axial images is sensitive in detection of fatty infiltration to assess paraspinal muscle degeneration, it is affected by inhomogeneities of magnetic fields and individual variabilities. The purpose of this study was to propose reference adjusted signal measures on T2W axial images and determine their capacities in reflecting age-related lumbar paraspinal muscle degeneration.
Methods
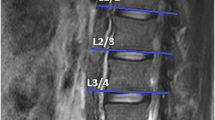
Lumbar MR images of 421 population-based subjects (177 men and 244 women, mean age 53.1 years, range 19.8–87.9 years) were studied. A custom software Spine Explore (Tulong 2.0) was used to automatically obtain paraspinal measurements of multifidus, erector spinae and psoas major. FCSA/TCSA was defined as functional cross-sectional area relative to total cross-sectional area of paraspinal muscle. Two new signal measures were canal-adjusted and cerebrospinal fluid (CSF)-adjusted signal, defined as the ratio between mean signal measurements and the mean signal of the canal and CSF.
Results
The raw signal measurements of the paraspinal muscles were weakly correlated to age (r = 0.28–0.39, P < 0.001). When the signal of canal (r = 0.43–0.59, P < 0.001) or CSF (r = 0.45–0.61, P < 0.001) was used as reference, the correlations substantially increased. Signal measurements of three paraspinal muscles, adjusted or not, were strongly associated with Goutallier score (ρ = 0.60–0.65, P < 0.001) and FCSA/TCSA (r = −0.64 to −0.82, P < 0.001). Greater Goutallier score was associated with greater age (r = 0.38–0.60, P < 0.001), while Lumbar indentation value (LIV) not.
Conclusion
On routine T2W axial MR images the adjusted signal measurements using an internal reference of CSF or canal can better reflect age-related degenerative changes in the paraspinal muscles.


Similar content being viewed by others
References
Rosenberg IH (2011) Sarcopenia: origins and clinical relevance. Clin Geriatr Med 27:337–339. https://doi.org/10.1016/j.cger.2011.03.003
Crawford RJ, Filli L, Elliott JM, Nanz D, Fischer MA, Marcon M, Ulbrich EJ (2016) Age- and level-dependence of fatty infiltration in lumbar paravertebral muscles of healthy volunteers. AJNR Am J Neuroradiol 37:742–748. https://doi.org/10.3174/ajnr.A4596
Kalichman L, Carmeli E, Been E (2017) The association between imaging parameters of the paraspinal muscles, spinal degeneration, and low back pain. Biomed Res Int 2017:2562957. https://doi.org/10.1155/2017/2562957
Ranger TA, Cicuttini FM, Jensen TS, Peiris WL, Hussain SM, Fairley J, Urquhart DM (2017) Are the size and composition of the paraspinal muscles associated with low back pain? A systematic review. Spine J 17:1729–1748. https://doi.org/10.1016/j.spinee.2017.07.002
Sasaki T, Yoshimura N, Hashizume H, Yamada H, Oka H, Matsudaira K, Iwahashi H, Shinto K, Ishimoto Y, Nagata K, Teraguchi M, Kagotani R, Muraki S, Akune T, Tanaka S, Kawaguchi H, Nakamura K, Minamide A, Nakagawa Y, Yoshida M (2017) MRI-defined paraspinal muscle morphology in Japanese population: the Wakayama spine study. PLoS ONE 12:e0187765. https://doi.org/10.1371/journal.pone.0187765
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clinical orthopaedics and related research 78–83
Tosato M, Marzetti E, Cesari M, Savera G, Miller RR, Bernabei R, Landi F, Calvani R (2017) Measurement of muscle mass in sarcopenia: from imaging to biochemical markers. Aging Clin Exp Res 29:19–27. https://doi.org/10.1007/s40520-016-0717-0
Fortin M, Battie MC (2012) Quantitative paraspinal muscle measurements: inter-software reliability and agreement using OsiriX and ImageJ. Phys Ther 92:853–864. https://doi.org/10.2522/ptj.20110380
D’Hooge R, Cagnie B, Crombez G, Vanderstraeten G, Dolphens M, Danneels L (2012) Increased intramuscular fatty infiltration without differences in lumbar muscle cross-sectional area during remission of unilateral recurrent low back pain. Man Ther 17:584–588. https://doi.org/10.1016/j.math.2012.06.007
Urrutia J, Besa P, Lobos D, Campos M, Arrieta C, Andia M, Uribe S (2018) Lumbar paraspinal muscle fat infiltration is independently associated with sex, age, and inter-vertebral disc degeneration in symptomatic patients. Skeletal Radiol 47:955–961. https://doi.org/10.1007/s00256-018-2880-1
Sether LA, Yu S, Haughton VM, Fischer ME (1990) Intervertebral disk: normal age-related changes in MR signal intensity. Radiology 177:385–388. https://doi.org/10.1148/radiology.177.2.2217773
Videman T, Nummi P, Battie MC, Gill K (1994) Digital assessment of MRI for lumbar disc desiccation. A comparison of digital versus subjective assessments and digital intensity profiles versus discogram and macroanatomic findings. Spine 19:192–198
Salamat S, Hutchings J, Kwong C, Magnussen J, Hancock MJ (2016) The relationship between quantitative measures of disc height and disc signal intensity with Pfirrmann score of disc degeneration. SpringerPlus 5:829. https://doi.org/10.1186/s40064-016-2542-5
Videman T, Gibbons LE, Battie MC (2008) Age- and pathology-specific measures of disc degeneration. Spine 33:2781–2788. https://doi.org/10.1097/BRS.0b013e31817e1d11
Hu X, Chen M, Pan J, Liang L, Wang Y (2018) Is it appropriate to measure age-related lumbar disc degeneration on the mid-sagittal MR image? A quantitative image study. Eur Spine J 27:1073–1081. https://doi.org/10.1007/s00586-017-5357-3
Hu XJ, Chen LH, Battie MC, Wang Y (2018) Methodology and cohort profile for the Hangzhou Lumbar Spine Study: a study focusing on back health in a Chinese population. J Zhejiang Univ Sci B 19:547–558. https://doi.org/10.1631/jzus.B1700484
Shen HT, Huang JW, Zheng QQ, Liu Y, Wang Y (2020) A deep learning based fully automated program to segment and quantify paraspinal muscles on axial lumbar spine MR images. The 46th ISSLS Annual Meeting combined with Spine week. Physical Therapy accepted
Fortin M, Lazary A, Varga PP, Battie MC (2017) Association between paraspinal muscle morphology, clinical symptoms and functional status in patients with lumbar spinal stenosis. Eur Spine J 26:2543–2551. https://doi.org/10.1007/s00586-017-5228-y
Takayama K, Kita T, Nakamura H, Kanematsu F, Yasunami T, Sakanaka H, Yamano Y (2016) New predictive index for lumbar paraspinal muscle degeneration associated with aging. Spine 41:E84-90. https://doi.org/10.1097/BRS.0000000000001154
Battaglia PJ, Maeda Y, Welk A, Hough B, Kettner N (2014) Reliability of the Goutallier classification in quantifying muscle fatty degeneration in the lumbar multifidus using magnetic resonance imaging. J Manipulative Physiol Ther 37:190–197. https://doi.org/10.1016/j.jmpt.2013.12.010
Betz M, Burgstaller JM, Held U, Andreisek G, Steurer J, Porchet F, Farshad M, Group LS (2017) Influence of paravertebral muscle quality on treatment efficacy of epidural steroid infiltration or surgical decompression in lumbar spinal stenosis-analysis of the Lumbar Spinal Outcome Study (LSOS) data: a Swiss prospective multicenter cohort study. Spine 42:1792–1798. https://doi.org/10.1097/BRS.0000000000002233
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127:990S-S991. https://doi.org/10.1093/jn/127.5.990S
Roubenoff R (2000) Sarcopenia and its implications for the elderly. Eur J Clin Nutr 54(Suppl 3):S40-47
Ali S, Garcia JM (2014) Sarcopenia, cachexia and aging: diagnosis, mechanisms and therapeutic options—a mini-review. Gerontology 60:294–305. https://doi.org/10.1159/000356760
Schiaffino S, Dyar KA, Ciciliot S, Blaauw B, Sandri M (2013) Mechanisms regulating skeletal muscle growth and atrophy. FEBS J 280:4294–4314. https://doi.org/10.1111/febs.12253
Hebert JJ, Kjaer P, Fritz JM, Walker BF (2014) The relationship of lumbar multifidus muscle morphology to previous, current, and future low back pain: a 9-year population-based prospective cohort study. Spine 39:1417–1425. https://doi.org/10.1097/BRS.0000000000000424
Simmons A, Tofts PS, Barker GJ, Arridge SR (1994) Sources of intensity nonuniformity in spin echo images at 1.5 T. Magn Reson Med 32:121–128. https://doi.org/10.1002/mrm.1910320117
Borhani AA, Hosseinzadeh K (2015) Quantitative versus qualitative methods in evaluation of T2 signal intensity to improve accuracy in diagnosis of pheochromocytoma. AJR Am J Roentgenol 205:302–310. https://doi.org/10.2214/AJR.14.13273
Luoma K, Raininko R, Nummi P, Luukkonen R (1993) Is the signal intensity of cerebrospinal fluid constant? Intensity measurements with high and low field magnetic resonance imagers. Magn Reson Imaging 11:549–555. https://doi.org/10.1016/0730-725x(93)90474-r
Acknowledgements
The authors thank Miss Ying Yuan for her continuous efforts in the establishment of the Hangzhou Lumbar Spine Study.
Funding
National Natural Science Foundation of China (No. 81772382), the Medicine and health science and technology plan in Zhejiang Province (2019RC171) and Program Science and Technology Department of Zhejiang Province (LGF20H060015) funds were received in support of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hu, X., Feng, Z., Shen, H. et al. New MR-based measures for the evaluation of age-related lumbar paraspinal muscle degeneration. Eur Spine J 30, 2577–2585 (2021). https://doi.org/10.1007/s00586-021-06811-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06811-6