Abstract
Purpose
Lumbar spinal stenosis (LSS) is a disabling condition associated with narrowing of the spinal canal or vertebral foramina. Paraspinal muscle atrophy and fatty infiltration have been reported in patients with chronic LBP and disc herniation. However, very few imaging studies have examined paraspinal muscle morphology and composition in patients with LSS. The purpose of this study was to investigate the association of paraspinal muscle size, composition and asymmetry with functional status in patients with LSS.
Methods
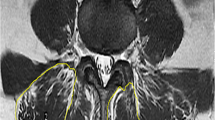
Thirty-six patients diagnosed with LSS at L4–L5 with neurogenic claudication were included. Paraspinal muscle measurements were obtained from axial T2-weighted MR images, bilaterally, at the level of the superior and inferior vertebral endplates of L5. Muscle measurements of interest included: total cross-sectional area (CSA), functional CSA (FCSA), the ratio of FCSA to CSA (FCSA/CSA) as an indicator of muscle composition, and relative % asymmetry in muscle CSA. The association between muscle parameters and other patient characteristics with function as indicated from Oswestry Disability Index (ODI) scores and pain interference status was investigated.
Results
Greater multifidus muscle fatty infiltration (e.g., lower FCSA/CSA) and lower psoas relative CSA were associated with lower function (higher ODI and pain interference scores) in univariable and multivariable analyses. There was no association between the different muscle parameters and stenosis severity or back or leg pain duration or severity.
Conclusions
Our findings suggest an association of multifidus muscle fatty infiltration and psoas muscle size with functional status in patients diagnosed with LSS. Future prospective studies are needed to evaluate whether such muscle parameters are associated with prognosis and functional recovery following surgical treatment.

Similar content being viewed by others
References
Deyo RA (1994) Magnetic resonance imaging of the lumbar spine—terrific test or tar baby? New Engl J Med 331(2):115–116
Backstrom KM, Whitman JM, Flynn TW (2011) Lumbar spinal stenosis-diagnosis and management of the aging spine. Man Ther 16(4):308–317
Ozcan-Eksi EE, Yagci I, Erkal H et al (2016) Paraspinal muscle denervation and balance impairment in lumbar spinal stenosis. Muscle Nerve 53(3):422–430
Yarjanian JA, Fetzer A, Yamakawa KS et al (2013) Correlation of paraspinal atrophy and denervation in back pain and spinal stenosis relative to asymptomatic controls. PM R 5(1):39–44
Leinonen V, Määttä S, Taimela S et al (2002) Impaired lumbar movement perception in association with postural stability and motor- and somatosensory-evoked potentials in lumbar spinal stenosis. Spine 27(9):975–983
Leinonen V, Määttä S, Taimela S et al (2003) Paraspinal muscle denervation, paradoxically good lumbar endurance, and an abnormal flexion-extension cycle in lumbar spinal stenosis. Spine 28(4):324–331
Kääriäinen T, Leinonen V, Taimela S et al (2013) Lumbar paraspinal and biceps brachii muscle function and movement perception in lumbar spinal stenosis. Eur Spine J 22(4):788–793
Tomkins-Lane CC, Battié MC (2013) Predictors of objectively measured walking capacity in people with degenerative lumbar spinal stenosis. J Back Musculoskelet Rehabil 26(4):345–352
Barker KL, Shamley DR, Jackson D (2004) Changes in the cross-sectional area of multifidus and psoas in patients with unilateral back pain: the relationship to pain and disability. Spine 29(22):E515–E519
Ploumis A, Michailidis N, Christodoulou P et al (2011) Ipsilateral atrophy of paraspinal and psoas muscle in unilateral back pain patients with monosegmental degenerative disc disease. Br J Radiol 84(1004):709–713
Hyun JK, Lee JY, Lee SJ et al (2007) Asymmetric atrophy of multifidus muscle in patients with unilateral lumbosacral radiculopathy. Spine 32(21):E598–E602
Kulig K, Scheid AR, Beauregard R et al (2009) Multifidus morphology in persons scheduled for single-level lumbar microdiscectomy: qualitative and quantitative assessment with anatomical correlates. Am J Phys Med Rehabil 88(5):355–361
Kim WH, Lee S, Lee DY (2011) Changes in the cross-sectional area of multifdus and psoas in unilateral sciatica caused by lumbar disc herniation. J Korean Neurosurg Soc 50(3):201–204
Battié MC, Niemelainen R, Gibbons LE et al (2012) Is level- and side-specific multifidus asymmetry a marker for lumbar disc pathology? Spine J 12(10):923–939
Chen YY, Pao JL, Liaw CK et al (2014) Image changes of paraspinal muscles and clinical correlations in patients with unilateral lumbar spinal stenosis. Eur Spine J 23(5):999–1006
Battié MC, Lazáry Á, Fairbank J et al (2014) Disc degeneration-related clinical phenotypes. Eur Spine J 23(Suppl 3):S305–S314
Ranson CA, Burnett AF, Kerslake R et al (2006) An investigation into the use of MR imaging to determine the functional cross sectional area of lumbar paraspinal muscles. Eur Spine J 15(6):764–773
Fortin M, Battié MC (2012) Quantitative paraspinal muscle measurements: inter-software reliability and agreement using OsiriX and ImageJ. Phys Ther 92(6):853–864
Fairbank J, Pynsent P (2000) The oswestry disability index. Spine 25(22):2940–2953
McGill S (2002) Low back disorders: evidence-based prevention and rehabilitation. Human Kinetics, Champaign, p 295
Wilke HJ, Wolf S, Claes LE et al (1995) Stability increase of the lumbar spine with different muscle groups: a biomechanical in vitro study. Spine 20(2):192–198
Kay AG (2001) An extensive literature review of the lumbar multifidus: biomechanics. J Man Manip Ther 9(1):17–39
Wilke HJ, Wolf S, Claes LE et al (1996) Influence of varying muscle forces on lumbar intradiscal pressure: an in vitro study. J Biomech 29(4):549–555
Hicks GE, Simonsick EM, Harris TB et al (2005) Trunk muscle composition as a predictor of reduced functional capacity in the health, aging and body composition study: the moderating role of back pain. J Gerontol Ser A Biol Sci Med Sci 60(11):1420–1424
Visser M, Kritchevsky SB, Goodpaster BH et al (2002) Leg muscle mass and composition in relation to lower extremity performance in men and women aged 70 to 79: the health, aging and body composition study. J Am Geriatr Soc 50(5):897–904
Prasarn M, Kostantinos V, Coyne E et al (2015) Does lumbar paraspinal muscle fatty degeneration correlate with aerobic index and oswestry disability index? Surg Neurol Intl 6(5):S240–S243
Hodges P, Holm AK, Hansson T et al (2006) Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine 31(25):2926–2933
Manini TM, Clark BC, Nalls MA et al (2007) Reduced physical activity increases intermuscular adipose tissue in healthy young adults. Am J Clin Nutr 85(2):377–384
Mooney V, Gulick J, Perlman M et al (1997) Relationships between myoelectric activity, strength, and MRI of lumbar extensor muscles in back pain patients and normal subjects. J Spinal Disord 10(4):348–356
Willemink MJ, Van Es HW, Helmhout PH et al (2012) The effects of dynamic isolated lumbar extensor training on lumbar multifidus functional cross-sectional area and functional status of patients with chronic nonspecific low back pain. Spine 37(26):E1651–E1658
Fortin M, Videman T, Gibbons LE et al (2014) Paraspinal muscle morphology and composition: a 15-yr longitudinal magnetic resonance imaging study. Med Sci Sports Exerc 46(5):893–901
Crawford RJ, Filli L, Elliott JM et al (2016) Age- and level-dependence of fatty infiltration in lumbar paravertebral muscles of healthy volunteers. AJNR Am J Neuroradiol 37(4):742–748
Lee SH, Park SW, Kim YB et al (2017) The fatty degeneration of lumbar paraspinal muscles on computed tomography scan according to age and disc level. Spine J 17(1):81–87
Kim YU, Kong YG, Lee J et al (2015) Clinical symptoms of lumbar spinal stenosis associated with morphological parameters on magnetic resonance images. Eur Spine J 24(10):2236–2243
Penning L (2000) Psoas muscle and lumbar spine stability: a concept uniting existing controversies. Critical review and hypothesis. Eur Spine J 9(6):577–585
Andersson GBJ, Ortengren R, Herberts P (1977) Quantitative electromyographic studies of back muscle activity related to posture and loading. Orthop Clin North Am 8(1):85–96
Nachemson A (1966) Electromyographic studies on the vertebral portion of the psoas muscle; with special reference to its stabilizing function of the lumbar spine. Acta Orthop Scand 37(2):177–190
Dangaria TR, Naesh O (1998) Changes in cross-sectional area of psoas major muscle in unilateral sciatica caused by disc herniation. Spine 23(8):928–931
Fischer MA, Nanz D, Reiner CS et al (2010) Diagnostic performance and accuracy of 3-D spoiled gradient-dual-echo MRI with water- and fat-signal separation in liver-fat quantification: comparison to liver biopsy. Invest Radiol 45:465–470
Hayashi N, Miyati T, Minami T et al (2013) Quantitative analysis of hepatic fat fraction by singlebreath-holding MR spectroscopy with T2 correction: phantom and clinical study with histologic assessment. Radiol Phys Technol 6:219–225
Yoo YH, Kim HS, Lee YH et al (2015) Comparison of multi-echo dixon methods with volume interpolated breath-hold gradient echo magnetic resonance imaging in fat-signal fraction quantification of paravertebral muscle. Korean J Radiol 16(5):1086–1095
Fisher MA, Nanz D, Shimakawa A et al (2013) Quantification of muscle fat in patients with low back pain: comparison of multi-echo MR imaging with single-voxel MR spectroscopy. Radiology 266(2):555–563
Gaeta M, Scribano E, Mileto A et al (2011) Muscle fat fraction in neuromuscular disorders: dual-echo dual-flip-angle spoiled gradient-recalled MR imaging technique for quantification: a feasibility study. Radiology 259(2):487–494
Acknowledgements
We thank Laura Gibbons for her help with data requests. Support was received from the Seventh Framework Programme (Health-2007-2013, Grant agreement no: 201626; GENODISC) and the Canada Research Chairs Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Fortin, M., Lazáry, À., Varga, P.P. et al. Association between paraspinal muscle morphology, clinical symptoms and functional status in patients with lumbar spinal stenosis. Eur Spine J 26, 2543–2551 (2017). https://doi.org/10.1007/s00586-017-5228-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5228-y