Abstract
Purpose
Despite the rapid increase in instrumented spinal fusions for a variety of indications, most studies focus on short-term fusion rates. Long-term clinical outcomes are still scarce and inconclusive. This study investigated clinical outcomes > 10 years after single-level instrumented posterolateral spinal fusion for lumbar degenerative or isthmic spondylolisthesis with neurological symptoms.
Methods
Cross-sectional long-term follow-up among the Dutch participants of an international multicenter randomized controlled trial comparing osteogenic protein-1 with autograft. Clinical outcomes were assessed using the Oswestry Disability Index (ODI), EQ-5D-3L and visual analogue scale (VAS) for leg and back pain, as well as questions on satisfaction with treatment and additional surgery.
Results
The follow-up rate was 73% (41 patients). At mean 11.8 (range 10.1–13.7) years after surgery, a non-significant deterioration of clinical outcomes compared to 1-year follow-up was observed. The mean ODI was 20 ± 19, mean EQ-5D-3L index score 0.784 ± 0.251 and mean VAS for leg and back pain, respectively, 34 ± 33 and 31 ± 28. Multiple regression showed that diagnosis (degenerative vs. isthmic spondylolisthesis), graft type (OP-1 vs. autograft) and 1-year fusion status (fusion vs. no fusion) were not predictive for the ODI at long-term follow-up (p = 0.389). Satisfaction with treatment was excellent and over 70% of the patients reported lasting improvement in back and/or leg pain. No revision surgeries for non-union were reported.
Conclusion
This study showed favourable clinical outcomes > 10 years after instrumented posterolateral spinal fusion and supports spondylolisthesis with neurological symptoms as indication for fusion surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rates of instrumented spinal fusion surgery increased markedly over the past decades, succeeded by growing evidence of especially short- and mid-term treatment effects for specific indications including lumbar spondylolisthesis associated with spinal stenosis [1,2,3,4,5,6]. Long-term clinical outcomes of spinal fusion are however still scarce and inconclusive [7,8,9,10,11]. Both deterioration and preservation of achieved clinical outcomes are reported, which can be partly explained by the heterogeneity in study designs and populations.
Another area of controversy is the relationship between radiographic fusion and clinical outcomes [12,13,14]. Among patients with degenerative lumbar spondylolisthesis treated with decompression and uninstrumented posterolateral fusion, solid arthrodesis appeared only beneficial for long-term clinical outcomes [15, 16]. However, in the presence of rigid instrumentation the necessity of a solid fusion within the first years can be debated. This emphasizes the need for long-term evaluations.
The current study investigated the long-term clinical outcomes of patients that were included in a randomized controlled trial (RCT) and who received instrumented posterolateral spinal fusion with autologous bone graft or osteogenic protein-1 for lumbar spondylolisthesis with neurological manifestations [17]. The primary objective was to assess disability, as determined by the Oswestry Disability Index (ODI), at long-term follow-up compared to baseline and 1 year after surgery. In addition, the effect of diagnosis, graft type and fusion status at 1-year follow-up were investigated. Secondary outcomes included pain experience, quality of life, satisfaction with treatment and reoperation rate.
Materials and methods
Study design and population
We performed a cross-sectional long-term follow-up among the Dutch participants of the previously published international multicenter Osigraft RCT [17]. In this original study, 134 patients were randomized to osteogenic protein-1 (OP-1, also known as BMP-7) or autograft for posterolateral spinal fusion from 2004 to 2008; 113 patients were included in the primary analysis. All patients underwent single-level instrumented posterolateral fusion of the lumbar spine for degenerative or isthmic spondylolisthesis with symptoms of neurological compression. Patients in the OP-1 group received Osigraft (Stryker Biotech, Hopkinton, MA, USA) combined with local bone. Patients in the control group received autologous bone graft from the iliac crest combined with local bone (autograft group). The primary outcome was overall success at 1-year follow-up, based on a combination of clinical outcomes and evidence of posterolateral fusion on computed tomography (CT) scans.
For the current study, patients were recruited from the Dutch study population with complete 1-year follow-up that consisted of 61 patients (Fig. 1). In January 2018, available patients were invited to participate by mailing an information letter, informed consent form, set of questionnaires and return envelope. They were asked to return the blank questionnaires in case they declined to participate. Non-responders were sent a reminder after 4 weeks.
Clinical outcomes
To assess long-term clinical outcomes, a set of various disease specific and generic questionnaires as well as additional questions was compiled. In line with the assessments done at baseline and 1 year after surgery in the original study, patients received the following validated questionnaires: ODI, EQ-5D-3L and visual analogue scale (VAS) for leg pain. Back pain was only assessed at long-term follow-up. The sum score of the disease specific ODI, defined as primary outcome, ranges from 0% (no disability) to 100% (maximum disability possible) [18]. Responses to the EQ-5D-3L were converted into a single health state index score ranging from − 0.329 (worst health state) to 1.000 (best possible health) [19, 20]. The VAS for pain runs from 0 (no pain) to 100 (terrible pain) and a score of ≤ 30 was considered as mild pain [21, 22].
Satisfaction with treatment at long-term follow-up was measured with a numeric rating scale (NRS) ranging from 0 (very dissatisfied) to 10 (very satisfied). In addition, patients were asked 1) how their complaints of back pain and leg pain have changed since the index surgery, 2) for the main effect of surgery on their pain complaints and 3) if they would choose the same treatment if they had the same condition and complaints. Finally, patients were asked for any lumbar spine reoperations since the index surgery.
Statistics
Data were processed and analyzed in SPSS Statistics 24.0 (IBM Corp., Armonk, NY, USA). Patient characteristics and all patient reported outcome measures were evaluated using descriptive statistics. Differences in ODI over time (baseline, 1-year and long-term follow-up) and the effect of graft type (OP-1 vs. autograft) were analyzed using a mixed analysis of variance (ANOVA) model for repeated measures. In addition, a multiple regression (enter method) was run to predict the ODI score at long-term follow-up from graft type, diagnosis (degenerative vs. isthmic spondylolisthesis) and fusion status at 1-year follow-up (fusion vs. doubtful fusion/non-union). EQ-5D-3L index scores and VAS leg pain over time were analyzed with Friedman’s test. For all statistical tests the threshold for significance was set to p < 0.05.
Ethical considerations
The Medical Ethical Committee of the University Medical Center Utrecht, The Netherlands, confirmed that this follow-up study did not fall under the Medical Research Involving Human Subjects Act and ethical approval was not required. Each study participant provided written informed consent.
Results
Study population
Since the 1-year follow-up, 5 of the 61 Dutch patients had died from causes unrelated to the index surgery, leaving 56 patients available for long-term follow-up. A total of 41 (73%) patients was enrolled, with a mean follow-up of 11.8 (range 10.1–13.7) years. Twelve patients did not respond to the questionnaire, and 3 were not willing to participate. The distribution among treatment groups is shown in Fig. 1.
Demographics, surgical details and 1-year fusion status on group level and per treatment condition are outlined in Table 1. The mean age of the 17 males and 24 females assessed at long-term follow-up was 62 ± 11 (range 30–91) years. The majority of the patients underwent surgery for isthmic spondylolisthesis (71%) and the overall 1-year fusion rate was 66%.
Clinical outcomes
ODI, EQ-5D-3L index scores and VAS pain scores at each timepoint on group level are listed in Table 2. Both means ± standard deviation and medians along with their interquartile range (IQR) are reported, as not all data are normally distributed.
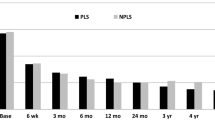
The mean ODI improved from 43 ± 15 at baseline to 13 ± 16 at 1 year and slightly regressed to 20 ± 19 at final follow-up. The mixed ANOVA model for repeated measures showed no significant interaction between timing of follow-up and graft type on ODI (F (2, 76) = 1.028, p = 0.363). Tests of within-subjects effects and between-subjects effects of the mixed ANOVA indicated, respectively, a main effect of time (F(2, 76) = 51.393, p < 0.001), but no main effect of graft type (F (1, 38) = 0.021, p = 0.884). Post-hoc analysis with Bonferroni correction confirmed a significant difference between baseline ODI and both post-operative time-points (p < 0.001), but not between 1-year and long-term follow-up (p = 0.075).
Multiple regression showed that the ODI at long-term follow-up could not be predicted based on the independent variables: diagnosis, graft type or 1-year fusion status (F (3, 37) = 1.033, p = 0.389). The overall model fit was R2 = 0.077. Based on these results and the sample size, all secondary outcomes are presented on group level.
As illustrated by Table 2, both the EQ-5D-3L index score and VAS leg pain regressed slightly between 1-year and long-term follow up. Friedman’s test confirmed that the EQ-5D-3L index and VAS leg pain scores differed between timepoints (Friedman’s Q(2) = 36, p < 0.001 and Friedman’s Q(2) = 28, p < 0.001 respectively). Post-hoc testing with Dunn-Bonferroni correction showed however that for both outcomes the regression during follow-up was not significant (EQ-5D-3L Z = 0.271, p = 0.769 and VAS leg pain Z = − 0.485, p = 0.147).
Satisfaction
Overall satisfaction with treatment was excellent, with a mean score of 8.0 ± 1.8 (range 3–10). The majority of the patients (76%) scored ≥ 8; only 5 patients scored < 6. Moreover, 78% would choose the same treatment again. The remaining patients answered this question with 'I don’t know'.
Figure 2 shows that 78% of the patients reported improvement in back pain and 71% improvement in leg pain. Of the 6 patients who reported much worsening of back and/or leg pain, only 1 patient underwent revision surgery at the same level (case 3 in Table 3). Three of these 6 patients were scored as fused at 1-year follow-up, including the revised case.
To the question 'On which complaint(s) had the surgery most effect?' 32% of the patients answered back pain, whereas 11% reported leg pain (Fig. 3). More than half of the patients (53%) reported a combined effect. According to 2 patients, the surgery was not effective at all. These patients scored consistently low on all satisfaction questions (satisfaction 4 and much worsening of both back and leg pain). Moreover, they reported severe disability based on the ODI at both 1-year and long-term follow-up (ranging between 40 and 47), but only at long-term follow-up a severe VAS leg pain score (> 80) and very low EQ-5D-3L index score (0.174). Their VAS back pain score at long-term follow-up was also > 80. One of these unsatisfied patients was scored as fused at 1-year follow-up.
Additional surgery
As outlined in Table 3, 4 patients underwent additional lumbar spine surgery since the final follow-up of the initial study, but none of these surgeries were related to non-union.
Discussion
This study showed excellent long-term (> 10 years) clinical outcomes of instrumented posterolateral spinal fusion for degenerative and isthmic spondylolisthesis. Although the clinical success of spinal fusions is often debated, the quality of life and satisfaction outcomes of the current study are comparable to the most successful orthopaedic procedures, such as hip and knee arthroplasty [23,24,25,26]. Interestingly, patients reported not only clinical improvement for neurological symptoms, but also at least as much for back pain. Only 11% indicated a main effect of surgery on leg pain. VAS back and leg pain scores at long-term follow-up were very similar. Apparently, back pain is an important contributor to discomfort in spondylolisthesis cases; also in patients with neurological symptoms, which were a prerequisite for inclusion in the original study.
Although the clinical outcomes remained satisfactory for 10 years, a slight but non-significant deterioration in ODI, EQ-5D-3L index and VAS leg pain score compared to 1-year follow-up was observed. Such diminishment of the treatment effect was also observed in a similar study by Ekman et al. and may be caused by adjacent segment degeneration or general effects of ageing [7]. These effects cannot be further quantified as no radiographic or clinical assessment was performed and information on concomitant diseases was lacking. On the other hand, the clinical relevance of adjacent segment degeneration seems to be limited [11, 27, 28]. In the current study, only 3 patients (7%) underwent additional surgery at an adjacent level. Another explanation could be the diminishing of the placebo effect of surgery over time or the psychological phenomenon known as response shift [29, 30].
Recognizing the difficulty to compare our results with previous long-term follow-up studies of spinal fusion for spondylolisthesis, due to differences in indication, type of surgery, follow-up period and/or outcome measures, our patients reported relatively low ODI and high EQ-5D-3L index scores at each timepoint [7, 8, 10, 31]. Satisfaction with treatment falls well within the range reported in the literature [7, 8, 10, 32, 33]. Contrary, the long-term VAS leg pain score was relatively high [8, 33]. Interestingly, none of these previous studies had neurological manifestations as strict inclusion criterion. We and many others believe that these symptoms are an important indication for spinal surgery, as illustrated by the less favourable treatment effect achieved for patients with chronic low back pain without nerve root compression [5, 6, 34]. A recent meta-analysis on surgical treatment for degenerative spinal conditions indicated that lumbar radiculopathy was associated with the greatest mean change in health related quality of life from baseline [35].
None of the participants underwent revision surgery for pseudoarthrosis, despite a substantial number of patients (34%) that were classified as ‘not fused’ on the CT-scan at 1-year follow-up. Also, based on the primary outcome measure ODI, no relationship was found between fusion status and long-term clinical outcome. Both patients classified as ‘fused’ and ‘not fused’ experienced a low level of disability at long-term follow-up (mean 21 ± 20 and 17 ± 16 respectively). Although a number of patients possibly developed further bony fusion in the course of the follow-up period, it is also possible that the combination of a fibrous union with pedicle screw instrumentation in situ offers sufficient stability in this patient population.
In line with the 1-year results of the original study, no difference in long-term ODI was seen between the patients who received OP-1 combined with local bone and solely autologous bone graft. This confirms the absence of a strong relationship between radiographic and clinical outcomes. Consecutive clinical trials failed to demonstrate non-inferiority of OP-1 versus autograft for spinal fusion and Osigraft was withdrawn from the market in 2015 [17, 36].
The findings of this study add to the scarce literature on long-term clinical outcomes of spinal fusion and endorse the importance of appropriate surgical patient selection. However, we do recognize some limitations. First, this long-term follow-up was confined to only the Dutch participants of the original international multicentre study. Despite the acceptable follow-up rate of 73%, this resulted in a relatively small sample size [37]. Participants were however equally distributed among the randomized treatment groups and their baseline and 1-year clinical outcomes were comparable with the outcomes of both the total study population and the entire Dutch sample, reducing the risk of selection bias. Third, the outcomes of this study were limited to patient reported outcome measures. Radiological fusion was only evaluated at 1-year follow-up. Finally, back pain was only assessed at long-term follow-up and in relation to that, patients’ pre-operative main complaint was unknown.
In conclusion, this study showed favourable long-term clinical outcomes in patients who underwent instrumented posterolateral spinal fusion for spondylolisthesis with neurological symptoms. Diagnosis (degenerative vs. isthmic spondylolisthesis), graft type (OP-1 vs. autograft) and 1-year fusion status (fusion vs. doubtful fusion/non-union) were not predictive for the ODI > 10 years after surgery. Comparison with available long-term follow-up studies stresses the necessity of established and strict indications for this procedure.
References
Deyo RA, Gray DT, Kreuter W et al (2005) United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 30:1441–1445. https://doi.org/10.1097/01.brs.0000166503.37969.8a
Deyo RA, Nachemson A, Mirza SK (2004) Spinal-fusion surgery - the case for restraint. N Engl J Med 350:722–726. https://doi.org/10.1056/NEJMsb031771
Herkowitz HN, Kurz LT (1991) Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am 73:802–808. https://doi.org/10.2106/00004623-199173060-00002
Möller H, Hedlund R (2000) Surgery versus conservative management in adult isthmic spondylolisthesis. Spine (Phila Pa 1976) 25:1711–1715. https://doi.org/10.1097/00007632-200007010-00016
Weinstein JN, Lurie JD, Tosteson TD et al (2007) Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 356:2257–2270. https://doi.org/10.1056/NEJMoa070302
Ghogawala Z, Dziura J, Butler WE et al (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374:1424–1434. https://doi.org/10.1056/nejmoa1508788
Ekman P, Möller H, Hedlund R (2005) The long-term effect of posterolateral fusion in adult isthmic spondylolisthesis: a randomized controlled study. Spine J 5:36–44. https://doi.org/10.1016/j.spinee.2004.05.249
Andersen T, Videbæk TS, Hansen ES et al (2008) The positive effect of posterolateral lumbar spinal fusion is preserved at long-term follow-up: a RCT with 11–13 year follow-up. Eur Spine J 17:272–280. https://doi.org/10.1007/s00586-007-0494-8
Abdu WA, Sacks OA, Tosteson ANA et al (2018) Long-Term results of surgery compared with nonoperative treatment for lumbar degenerative spondylolisthesis in the spine patient outcomes research trial (SPORT). Spine (Phila Pa 1976) 43:1619–1630. https://doi.org/10.1097/BRS.0000000000002682
Turunen V, Nyyssönen T, Miettinen H et al (2012) Lumbar instrumented posterolateral fusion in spondylolisthetic and failed back patients: a long-term follow-up study spanning 11–13 years. Eur Spine J 21:2140–2148. https://doi.org/10.1007/s00586-012-2320-1
Endler P, Ekman P, Ljungqvist H et al (2019) Long-term outcome after spinal fusion for isthmic spondylolisthesis in adults. Spine J 19:501–508. https://doi.org/10.1016/j.spinee.2018.08.008
Dhall SS, Choudhri TF, Eck JC et al (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 5: correlation between radiographic outcome and function. J Neurosurg Spine 21:31–36. https://doi.org/10.3171/2014.4.SPINE14269
Sengupta DK, Herkowitz HN (2005) Degenerative spondylolisthesis: review of current trends and controversies. Spine (Phila Pa 1976) 30:S71-81. https://doi.org/10.1097/01.brs.0000155579.88537.8e
Djurasovic M, Glassman SD, Dimar JR et al (2011) Does fusion status correlate with patient outcomes in lumbar spinal fusion? Spine (Phila Pa 1976) 36:404–409. https://doi.org/10.1097/BRS.0b013e3181fde2c4
Kornblum MB, Fischgrund JS, Herkowitz HN et al (2004) Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine (Phila Pa 1976) 29:726–733. https://doi.org/10.1097/01.BRS.0000119398.22620.92
Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H (2008) Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. Eur Spine J 17:1107–1112. https://doi.org/10.1007/s00586-008-0695-9
Delawi D, Jacobs W, van Susante JLC et al (2016) OP-1 compared with iliac crest autograft in instrumented posterolateral fusion: a randomized, multicenter non-inferiority trial. J Bone Joint Surg Am 98:441–448. https://doi.org/10.2106/JBJS.O.00209
Fairbank JC, Pynsent PB (2000) The oswestry disability index. Spine (Phila Pa 1976) 25:2940–52. https://doi.org/10.1097/00007632-200011150-00017
The EuroQol Group (1990) EuroQol - a new facility for the measurement of health-related quality of life. Health Policy (New York) 16:199–208. https://doi.org/10.1016/0168-8510(90)90421-9
Janssen B, Szende A (2014) Population norms for the EQ-5D. Springer, Netherlands
Carragee EJ, Cheng I (2010) Minimum acceptable outcomes after lumbar spinal fusion. Spine J 10:313–320. https://doi.org/10.1016/j.spinee.2010.02.001
Boonstra AM, Preuper HRS, Balk GA, Stewart RE (2014) Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 155:2545–2550. https://doi.org/10.1016/j.pain.2014.09.014
Hansson T, Hansson E, Malchau H (2008) Utility of spine surgery. Spine (Phila Pa 1976) 33:2819–2830. https://doi.org/10.1097/brs.0b013e31818e2914
Jansson KÅ, Granath F (2011) Health-related quality of life (EQ-5D) before and after orthopedic surgery. Acta Orthop 82:82–89. https://doi.org/10.3109/17453674.2010.548026
Lindgren JV, Wretenberg P, Kärrholm J et al (2014) Patient-reported outcome is influenced by surgical approach in total hip replacement: a study of the Swedish hip arthroplasty register including 42 233 patients. Bone Joint J 96:590–596. https://doi.org/10.1302/0301-620X.96B5.32341
Shan L, Shan B, Suzuki A et al (2015) Intermediate and long-term quality of life after total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Am 97:156–168. https://doi.org/10.2106/JBJS.M.00372
Park P, Garton HJ, Gala VC et al (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29:1938–1944. https://doi.org/10.1097/01.brs.0000137069.88904.03
Ekman P, Möller H, Shalabi A et al (2009) A prospective randomised study on the long-term effect of lumbar fusion on adjacent disc degeneration. Eur Spine J 18:1175–1186. https://doi.org/10.1007/s00586-009-0947-3
Schwartz CE, Sajobi TT, Lix LM et al (2013) Changing values, changing outcomes: the influence of reprioritization response shift on outcome assessment after spine surgery. Qual Life Res 22:2255–2264. https://doi.org/10.1007/s11136-013-0377-x
Finkelstein JA, Schwartz CE (2019) Patient-reported outcomes in spine surgery: past, current, and future directions. J Neurosurg Spine 31:155–164. https://doi.org/10.3171/2019.1.SPINE18770
Fritzell P, Hägg O, Gerdham P, et al (2018) Swespine 25 years. In 2017 annual report follow up of spine surgery performed in Sweden
Glaser J, Stanley M, Sayre H et al (2003) A 10-year follow-up evaluation of lumbar spine fusion with pedicle screw fixation. Spine (Phila Pa 1976) 28:1390–1395. https://doi.org/10.1097/01.BRS.0000067112.15753.AD
Wenger M, Sapio N, Markwalder TM (2005) Long-term outcome in 132 consecutive patients after posterior internal fixation and fusion for grade I and II isthmic spondylolisthesis. J Neurosurg Spine 2:289–297. https://doi.org/10.3171/spi.2005.2.3.0289
Hedlund R, Johansson C, Hägg O et al (2016) The long-term outcome of lumbar fusion in the Swedish lumbar spine study. Spine J 16:579–587. https://doi.org/10.1016/j.spinee.2015.08.065
Nayak NR, Stephen JH, Piazza MA et al (2019) Quality of life in patients undergoing spine surgery: systematic review and meta-analysis. Glob Spine J 9:67–76. https://doi.org/10.1177/2192568217701104
Vaccaro AR, Lawrence JP, Patel T et al (2008) The safety and efficacy of OP-1 (rhBMP-7) as a replacement for iliac crest autograft in posterolateral lumbar arthrodesis: a long-term (& gt 4 years) pivotal study. Spine (Phila Pa 1976) 33:2850–62. https://doi.org/10.1097/BRS.0b013e31818a314d
OME Cleveland Clinic Orthopaedics (2020) Value in research: achieving validated outcome measurements while mitigating follow-up cost. J Bone Joint Surg Am 102:419–427. https://doi.org/10.2106/JBJS.19.00531
Acknowledgements
The authors thank the local study coordinators A. Hol, MSc and B.C. van der Zwaard, PhD for their help with data collection and administrative matters, and medical student M.G.H. Vrijkorte for his contributions in data entry, analysis and reporting.
Funding
The authors received no financial support for the conduct or publication of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The Medical Ethical Committee of the University Medical Center Utrecht, The Netherlands, has confirmed that no ethical approval is required for this study.
Consent to participate
Written informed consent was obtained from all participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lehr, A.M., Delawi, D., van Susante, J.L.C. et al. Long-term (> 10 years) clinical outcomes of instrumented posterolateral fusion for spondylolisthesis. Eur Spine J 30, 1380–1386 (2021). https://doi.org/10.1007/s00586-020-06671-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06671-6