Abstract
Purpose
No clinical CT-based classification system is currently in use for lumbar foraminal stenosis. MRI scanners are not easily available, are expensive and may be contraindicated in an increasing number of patients. This study aimed to propose and evaluate the reproducibility of a novel CT-based classification for lumbar foraminal stenosis.
Materials and methods
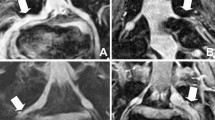
The grading was developed as four grades: normal foramen—Grade 0, anteroposterior (AP)/superoinferior (SI) (single plane) fat compression—Grade 1, both AP/SI compression (two planes) without distortion of nerve root—Grade 2 and Grade 2 with distortion of nerve root—Grade 3.
A total of 800 lumbar foramen of a cohort of 100 random patients over the age of 60 who had undergone both CT and MRI scans were reviewed by two radiologists independently to assess agreement of the novel CT classification against the MRI-based grading system of Lee et al. Interobserver(n = 400) and intraobserver agreement(n = 160) was also evaluated. Agreement analysis was performed using the weighted kappa statistic.
Results
A total of 100 patients (M:F = 45:55) with a mean age of 68.5 years (range 60–83 years were included in the study. The duration between CT and MRI scans was 98 days (range 0–540, SD—108). There was good correlation between CT and MRI with kappa scores (k = 0.81) and intraobserver kappa of 0.89 and 0.98 for the two readers.
Conclusion
The novel CT-based classification correlates well with the MRI grading system and can safely and accurately replace it where required.




Similar content being viewed by others
References
Orita S, Inage K, Eguchi Y et al (2016) Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur J OrthopSurgTraumatol 26:685–693. https://doi.org/10.1007/s00590-016-1806-7
Porter RW, Hibbert CEC (1984) The natural history of root entrapment syndrome. Spine 9:418–421 ((Phila Pa 1976))
Kunogi JHM (1991) Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine 16:1312–1320 ((Phila Pa 1976))
Jenis LG, An HS (2000) Spine update: lumbar foraminal stenosis. Spine 25:389–394 ((Phila Pa 1976))
Putti V (1927) New conceptions in the pathogenesis of sciatic pain. Lancet 210:53–60. https://doi.org/10.1016/S0140-6736(01)30667-0
Mitchell C (1934) Lumbosacral facetectomy for relief of sciatic pain. J Bone JtSurg Br 36-B:230–237
Burton CV, Kirkaldy-Willis WH, Yong-Hing KHK (1981) Causes of failure of surgery on the lumbar spine. ClinOrthopRelat Res 157:183–187
Jenis LG, An HSGR (2001) Foraminal stenosis of the lumbar spine: a review of 65 surgical cases. Am J Orthop (Belle Mead NJ) 30:205–211
Wildermuth S, Zanetti M, Duewell S, Schmid MR, Romanowski B, Benini A, Böni T, Hodler J (1998) Lumbar spine: quantitive and qualitative assessment of positional (upright flexion and extension) MR imaging and myelography. Radiology 207:391–398
Lee S, Lee JW, Yeom JS, Kim K-J, Kim H-J, SooKyo Chung HSK (2010) A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol 194:1095–1098
Park HJ, Kim SS, Lee SY, Park NH, Rho MH, Hong HP, Kwag HJ, Kook SH, Choi SH (2012) Clinical correlation of a new MR imaging method for assessing lumbar foraminal stenosis. Am J Neuroradiol 33:818–822
No authors listed (2017) Geographical distribution of MRI—Figure 5: distribution of MRI units across Canada in 2017. In: Can. Med. Imaging Invent. 2017. https://www.cadth.ca/canadian-medical-imaging-inventory-2017. Accessed 20 Oct 2020
Matsumoto KS, Kashima S, Awai K (2015) Geographic distribution of CT, MRI and PET devices in Japan: a longitudinal analysis based on national census data. PLoS ONE 10:e0126036. https://doi.org/10.1371/journal.pone.0126036
Khaliq AA, Deyo D, Duszak R Jr (2015) The impact of hospital characteristics on the availability of radiology services at critical access hospitals. J Am CollRadiol 12:1351–1356. https://doi.org/10.1016/j.jacr.2015.09.008
Ginde AA, Foianini A, Renner DM et al (2008) Availability and quality of computed tomography and magnetic resonance imaging equipment in U.S. emergency departments. AcadEmerg Med 15:780–783. https://doi.org/10.1111/j.1553-2712.2008.00192.x
No Authors Listed (2011) Pakistan country report. In: RAD-AID-Pakistan-health-care-radiology-report
Moser JW (2008) 2007 Survey of radiologists: practice characteristics, ownership, and affiliation with imaging centers. J Am CollRadiol 5:965–971. https://doi.org/10.1016/j.jacr.2008.03.011
No authors listed (2014) Medical equipment: magnetic resonance imaging (MRI) units per million population. In: World Heal. Organ. https://www.who.int/diagnostic_imaging/collaboration/mripermill_14.jpg?ua=1. Accessed 20 Oct 2020
No authors listed (2016) Global health observatory data repository—Medical equipment—Data by country. In: World Heal. Organ. https://apps.who.int/gho/data/node.main.510. Accessed 20 Oct 2020
Rinck PA (2020) 21–02 How many MRI machines are there?—MR imaging: facts and figures. In: Rinck PA (ed) Magnetic resonance in medicine a critical introduction, 12th edn. BoD, Germany, p 432
Dill T (2008) Contraindications to magnetic resonance imaging. Heart 94:943–948. https://doi.org/10.1136/hrt.2007.125039
Shellock FG, Crues JV (2004) MR procedures: biologic effects, safety, and patient care. Radiology 232:635–652
Cohen J (1968) Weighted kappa: nominal scale agreement provision for scaled disagreement or partial credit. Psychol Bull 70:213–220. https://doi.org/10.1037/h0026256
McHugh ML (2012) Lessons in biostatistics Interrater reliability: the kappa statistic. BiochemMedica 22:276–282
SPSS version 24, SPSS Inc, Chicago, Illinois U SPSS version 24
Stephens M, Evans J, O’Brien J (1991) Lumbar intervertebral foramens: an in vitro study of their shape in relation to intervertebral disc pathology. Spine 16:525–529 ((Phila Pa 1976))
Macnab I (1971) Negative disc exploration: an analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone JtSurg Am 53:891–903
Mandell JC, Czuczman GJ, Gaviola GC et al (2017) The lumbar neural foramen and transforaminal epidural steroid injections: an anatomic review with key safety considerations in planning the percutaneous approach. Am J Roentgenol 209:W26–W35. https://doi.org/10.2214/AJR.16.17471
Arnoldi CC, Brodsky AE, Cauchoix J et al (1976) Lumbar spinal stenosis and nerve root entrapment syndromes. Definition and classification. ClinOrthopRelat Res 115:4–5. https://doi.org/10.1097/00003086-197603000-00002
Hasegawa T, An HS, Haughton VM (1993) Imaging anatomy of the lateral lumbar spinal canal. Semin Ultrasound, CT, MRI 14:404–413. https://doi.org/10.1016/S0887-2171(05)80034-4
Aota Y, Niwa T, Yoshikawa K et al (2007) Magnetic resonance imaging and magnetic resonance myelography in the presurgical diagnosis of lumbar foraminal stenosis. Spine 32:896–903. https://doi.org/10.1097/01.brs.0000259809.75760.d5 ((Phila Pa 1976))
Eguchi Y, Ohtori S, Suzuki M et al (2016) Diagnosis of lumbar foraminal stenosis using diffusion tensor imaging. Asian Spine J 10:164–169. https://doi.org/10.4184/asj.2016.10.1.164
Ogbole GI, Adeyomoye AO, Badu-Peprah A et al (2018) Survey of magnetic resonance imaging availability in West Africa. Pan Afr Med J 30:240
Adejoh T, Onwujekwe EC, Abba M et al (2018) Computed tomography scanner census and adult head dose in Nigeria. Egypt J RadiolNucl Med 49:66–70. https://doi.org/10.1016/j.ejrnm.2017.09.001
Hricak H, Amparo EG (1984) Body MRI: alleviation of claustrophobia by prone positioning. Radiology 152:819. https://doi.org/10.1148/radiology.152.3.6463267
Quirk ME, Letendre AJ, Ciottone RA, Lingley JF (1989) Anxiety in patients undergoing MR imaging. Med Dosim 14:294. https://doi.org/10.1016/0958-3947(89)90021-6
Meléndez JC, Mccrank E (1993) Anxiety-related reactions associated with magnetic resonance imaging examinations. JAMA J Am Med Assoc 270:745–747. https://doi.org/10.1001/jama.1993.03510060091039
Katznelson R, Djaiani GN, Minkovich L et al (2008) Prevalence of claustrophobia and magnetic resonance imaging after coronary artery bypass graft surgery. Neuropsychiatr Dis Treat 4:487–493. https://doi.org/10.2147/ndt.s2699
Koh SAS, Lee W, Rahmat R et al (2017) Interethnic variation in the prevalence of claustrophobia during MRI at Singapore general hospital: does a wider bore MR scanner help? ProcSingapHealthc 26:1–5. https://doi.org/10.1177/2010105817695819
Beers GJ, Carter AP, Leiter BE et al (1985) Interobserver discrepancies in distance measurements from lumbar spine CT scans. Am J Roentgenol 144:395–398. https://doi.org/10.2214/ajr.144.2.395
Mayoux-Benhamou MA, Revel M, Aaron C et al (1989) A morphometric study of the lumbar foramen—Influence of flexion-extension movements and of isolated disc collapse. SurgRadiolAnat 11:97–102. https://doi.org/10.1007/BF02096463
No authors listed (2019) Radiation dose in X-ray and CT exams. In: RadiologyInfo.org. https://www.radiologyinfo.org/en/info.cfm?pg=safety-xray. Accessed 20 Oct 2020
de Gonzalez AB, Mahesh M, Kim K-P et al (2009) Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med 169:2071–2077. https://doi.org/10.1016/j.physbeh.2017.03.040
Smith-Bindman R, Lipson J, Marcus R et al (2009) Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med 169:2078–2086. https://doi.org/10.1001/archinternmed.2009.427.Radiation
Pearce MS, Salotti JA, Little MP et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380:499–505. https://doi.org/10.1016/S0140-6736(12)60815-0
Lin EC (2010) Radiation risk from medical imaging. Mayo ClinProc 85:1142–1146. https://doi.org/10.4065/mcp.2010.0260
Sagerman RH (1993) Radiation-induced cataracts: simple but difficultto quantify. Int J RadiatOncolBiolPhys 26:713–714
Takeda A, Shigematsu N, Suzuki S et al (1999) Late retinal complications of radiation therapy for nasal and paranasal malignancies: relationship between irradiated-dose area and severity. Int J RadiatOncolBiolPhys 44:599–605
Funding
No funding was received in relation to this article.
Author information
Authors and Affiliations
Contributions
SH contributed to original concept, discussed framework, analysed data, wrote and critically reviewed article for final acceptance. MM discussed framework, analysed data, critically reviewed article for final acceptance. VG discussed framework and critically reviewed article for final acceptance. CA analysed scans and data and critically reviewed article for final acceptance. SJ analysed scans and data, critically reviewed article for final acceptance. RB discussed framework, analysed data, wrote and critically reviewed article for final acceptance.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in relation to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Haleem, S., Malik, M., Guduri, V. et al. The Haleem–Botchu classification: a novel CT-based classification for lumbar foraminal stenosis. Eur Spine J 30, 865–869 (2021). https://doi.org/10.1007/s00586-020-06656-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06656-5