Abstract
Purpose
There have been few reports on the risk factors for tracheostomy and the possibility of patients for decannulation. The purpose of this study was to identify factors necessitating tracheostomy after cervical spinal cord injury (SCI) and detect features predictive of successful decannulation in tracheostomy patients.
Methods
One hundred and sixty four patients with cervical fracture/dislocation were retrospectively reviewed. The patients comprised 142 men and 22 women with a mean age of 44.9 years. The clinical records were reviewed for patients’ demographic data, smoking history, level of cervical spine injury, injury patterns, neurological status, evidence of direct thoracic trauma and head injury, tracheostomy placement, and decannulation. Risk factors necessitating tracheostomy and factors predicting decannulation were statistically analysed.
Results
Twenty-five patients (15.2 %) required tracheostomy. Twenty-one patients were successfully decannulated. Smoking history (relative risk [RR], 3.05; p = 0.03) and complete SCI irrespective of injury level (C1–4 complete SCI: RR, 67.55; p < 0.001, C5–7 complete SCI: RR, 57.88; p < 0.001) were significant risk factors necessitating tracheostomy. C1–4 complete SCI was more frequent among those who could not be decannulated. However, even in patients with high cervical complete SCI at the time of injury, patients regaining sufficient movement to shrug their shoulders within 3 weeks after injury could later be decannulated.
Conclusions
The risk factors for tracheostomy after complete SCI were a history of smoking and complete paralysis irrespective of the level of injury. High cervical level complete SCI was found to be a risk factor for the failure of decannulation in patients without shoulder shrug within 3 weeks after injury.
Similar content being viewed by others
Introduction
Cervical spinal cord injuries (C-SCIs) are catastrophic injuries. Such injuries are often associated with neurological deficits, and respiratory dysfunction secondary to the injury can be a major for patients with C-SCI patients with them [7, 9]. Respiratory dysfunction is the biggest cause of death after C-SCI in such patients, and pneumonia or atelectasis often occurs after the injury [3, 7, 9].
Tracheostomy provides a secure airway, facilitates secretion control and decreases the risk of pulmonary complications in C-SCI patients [4, 5, 6, 11, 13, 15, 16, 20, 21]. It has been reported that 21–77 % of patients with C-SCI require tracheostomy [6, 11, 13, 15, 21]. Early tracheostomy has been advocated from the viewpoint of medical economics and the patient’s prognosis because it decreases the length of the hospital/intensive care unit stay and the rate of infectious complications, and increases the patient’s ventilation tolerance [4, 5, 13, 16, 20, 21]. However, quick identification of the risk factors associated with tracheostomy for each patient is necessary for early tracheostomy, but the identification process is difficult. Several risk factors frequently associated with tracheostomy after C-SCI, such as the severity and the level of neurological damage, age and other traumas, have been reported; however, the question of risk factors is still a controversial one [6, 13, 15].
A major problem related to tracheostomy after C-SCI is that there is a paucity of data regarding the category of patients who can successfully undergo decannulation in future and the time they can be decannulated. The invasiveness secondary to tracheostomy is both physical and mental. It has been reported that there is a decline in a patient’s mental health after tracheostomy, attributable to worsening self-esteem [12, 14]. Therefore, it is important for patients to be aware about the possibility of decannulation, because this helps them to accept subsequent therapy and the resulting situation. However, as far as we know, there have been few reports regarding the suitability of patients for decannulation. As a result, surgeons have not yet been able to either provide sufficient information to patients about their tracheostomy prognosis or decrease patients’ anxiety.
For addressing the above issues, we conducted a study involving a review of the clinical and radiological findings indicating a need for tracheostomy after C-SCI, and identification of features that would help to predict patients suitable for decannulation.
Materials and methods
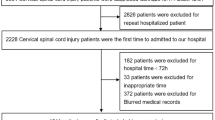
Patient population
This study involved 164 consecutive patients who experienced C-SCI between 1995 and 2009 who were treated at a single institute (CR hospital). All patients had received surgical treatment within 2 months of injury. The mean follow-up period was 59.9 months. Minimum follow-up was 3 days because of renal failure, and maximum follow-up was 165 months. The patients comprised 142 men and 22 women with a mean age of 44.9 years (range 14–90 years).
The clinical records were reviewed for patients’ demographic data, smoking history, level of cervical spine injury, injury patterns, neurological status, evidence of direct thoracic trauma and head injury, tracheostomy placement, and decannulation. Patients who underwent tracheostomy for specific anatomic injuries such as facial injuries were not included in this study. The decision to proceed to tracheostomy was made at the discretion of the attending surgeon or emergency doctor. The decision to perform decannulation was made when two criteria were met: the patient (1) was not dependent on ventilatory assistance and (2) did not require frequent suctioning for tracheal secretions. We tested the swallowing ability and gag reflexes before proceeding to decannulation.
Cervical injury patterns were classified according to Allen’s classification for middle and lower cervical spine injuries [1]. Allen’s classification was established to classify the fractures/dislocations of the low cervical spine according to the mechanism of injury. It has two unique features. First, there are six categories of cervical injuries, and each category name indicates the state of the cervical spine at injury and the dominant force vector. Second, each category is divided into stages according to the severity of spinal column injury, with the neurological damage at injury being more severe with each advance in stage.
The American Spinal Injury Association (ASIA) impairment scale was used to assess neurological status [19]. Neurological outcomes were evaluated and tracheotomy status was confirmed during outpatient appointments or by telephone interviews. Patients were neurologically evaluated weekly during their hospitalization.
Neurological impairment level
Neurological impairment level was determined by the strengths of the key muscles [10, 19]: shoulder shrug (C4), elbow flexion (C5), wrist extension (C6) and elbow extension (C7).
Operative procedure
Posterior spinal arthrodesis was performed in all cases. This involved short segmental fixation using a pedicle screw system [23]. In addition to the posterior arthrodesis, posterior laminoplasty was performed in 17 patients and posterior laminectomy was performed in 3 patients with a multilevel narrow spinal canal. Supplemental anterior surgery involved anterior corpectomy and placement of an iliac strut bone graft in five patients with marked destruction of the vertebral body.
Postoperative treatment
The patients started ambulation and rehabilitation soon after removal of the suction drain. They were placed in a rigid cervical collar for approximately 1 month after surgery. However, no external fixation was used for patients with ASIA grade A or B because their activity levels were relatively low.
Statistical analysis
Statistical analyses were performed using SPSS version 17 software (SPSS Inc, Chicago, IL, USA). An unpaired t test, the Mann–Whitney U test or Fisher’s exact test was used to compare the groups. Logistic regression analysis was used to determine the risk factors indicating the need for tracheostomy. The significance of parameters was evaluated by univariate analysis. Factors with a p value of <0.20 in the univariate analysis were included in a multivariate analysis. Differences were considered significant at a p value of <0.05.
Results
Preoperative ASIA grade was A: 57, B: 8, C: 23, D: 36, E: 20. Postoperative ASIA grade was A: 55, C: 8, D: 39, E: 42. There were four reoperations because of deep wound infection. The postoperative deep infection was successfully managed by surgical debridement, continuous irrigation and intravenous administration of antibiotics without the need to remove the hardware.
A total of 25 patients (15.2 %) underwent tracheostomy. All 25 patients were treated by the posterior approach; no additional anterior surgeries were performed. Tables 1 and 2 summarize the demographic data of the 25 patients (23 men and 2 women with a mean age of 44.2 years). The mean time interval from spine or spinal cord injury to tracheostomy was 5.0 days (range 1–18 days). Two patents died during the follow-up period because of respiratory dysfunction (one at 51 days after surgery, the other at 134 days after surgery). Tracheostomy tubes could not be removed in two patients during the follow-up period; the other 21 patients were successfully decannulated. The two patients without decannulation were in failure of mechanical ventilator weaning. Both patients had spontaneous breathing difficulty at night. The four patients (two patients who died and two patients who could not be decannulated for a long period after spinal cord injury) comprised a decannulation-failure group. The two patients who died soon after surgery were not able to shrug their shoulders within 3 weeks. There were no cases where the tracheostomy was removed but was deemed necessary again after some period of time.
The mean time interval from tracheostomy to decannulation was 45.9 days (range 9–148 days). There were no cases of deep wound infection around the tracheostomy tube nor any other complications related to the tracheostomy.
Comparison of patients with and without tracheostomy
The number of patients with a history of smoking and C1–4 and C5–7 ASIA A was significantly higher in the tracheostomy group, whereas the number of patients with C5–7 ASIA B–E was significantly higher in the non-tracheostomy group (Table 2).
Risk factor analysis of the need for tracheostomy
Multivariate logistic analysis revealed smoking history and complete cervical spinal cord injury at either level C1–C4 or level C5–C7 to be significant risk factors for tracheostomy after cervical spinal fracture/dislocation injury. Smoking history: relative risk (RR), 3.05; 95 % CI, 1.09–8.51; p = 0.03. Complete spinal cord injury (C1–4): RR, 67.55; 95 % CI, 6.65–686.29; p < 0.001. Complete spinal cord injury (C5–7): RR, 57.88; 95 % CI, 6.97–480.90; p < 0.001 (Table 3).
Comparison of patients with and without decannulation
Patients with C1–4 ASIA A were significantly more common in the non-decannulation group, whereas all patients with C5–7 ASIA A could be decannulated. The ability to perform a shoulder shrug was identified as a factor more clearly indicative of the possibility of decannulation; every patient who could perform a shoulder shrug within 3 weeks of injury was successfully decannulated (Table 4).
Discussion
Patients with C-SCI are at increased risk of respiratory failure that may lead to the need for tracheostomy [6, 11, 13, 15, 21]. Pulmonary complications are the most common complications in patients with C-SCI [7, 9]. Eighty percent of deaths among patients with C-SCI are secondary to pulmonary dysfunction, with pneumonia being the aetiology in 50 % cases [3]. Patients with respiratory failure after C-SCI will require intubation and mechanical ventilation, leading to tracheostomy. It has been reported that 21–77 % of patients with C-SCI have undergone tracheostomy [6, 11, 13, 15, 21].
When patients with C-SCI are taken to hospital, doctors must judge those requiring tracheostomy and then perform the tracheostomy as soon as possible [4, 5, 13, 16, 20, 21]. The benefits of tracheostomy have been discussed previously: improved secretion control, lower rates of pulmonary infection and laryngeal injury, the ability to be given oral nutrition, and shorter hospital/intensive care unit stays [4, 13, 16, 20]. An early tracheostomy maximizes these benefits, makes increased patient mobilization possible and minimizes the cost of hospitalization [4, 21].
The ability to predict the patients who will require tracheostomy makes it possible to perform the procedure earlier. For this reason, identifying these patients has been the focus of numerous studies. Thus far, such studies have identified several risk factors for post-injury tracheostomy: rostral ASIA A level (especially in C2–C4 injury), age (>45 years), comorbid lung diseases, smoking history, pre-existing comorbid illness, the severity of impaired consciousness, high level injury severity score and active pneumonia [6, 13, 15].
In the present study, ASIA A level (irrespective of level of injury) and smoking history were found to be the significant risk factors for tracheostomy after C-SCI. It has previously been reported that smoking is associated with mucous overproduction and airway inflammation [22]. A history of smoking may contribute to intensifying hypersecretion of bronchial mucous after C-SCI and may even lead to pneumonia.
Interestingly, the tracheostomy rate was also high if complete neurological impairment was present, irrespective of the level of injury. Branco et al. [6] reported the same results and concluded that the severity of paralysis was an independent risk factor. On the basis of these results, tracheostomy has to be prepared even in patients with lower level C-SCI if the paralysis is complete.
Whereas prompt tracheostomy is vital, it is also important to inform patients about the possibility and the timing of decannulation, although there have been few reports that address this issue. This is because there have been reports showing that tracheostomy has the potential to cause a significant decline in a patient’s mental health, attributable to worsening self-esteem [12, 14]. Therefore, if spine surgeons can present the possibility of later decannulation, patients would be more likely to accept subsequent therapy and the resulting situation.
Regarding decannulation, as far as the authors know, there have been no reports published on post-SCI tracheostomy patients who were successfully decannulated. There have, however, been some reports regarding the possibility of weaning patients off mechanical ventilation. The reasons proposed in these reports for failure to achieve this included high cervical spinal cord injury, age >50 years and medical comorbidities [2, 8]. In the present study, high cervical spinal cord injury (C1–4 ASIA A) was a significant risk factor for the failure of decannulation. In particular, patients with injuries above C4 level who could not perform a shoulder shrug within 3 weeks after injury had a significantly higher risk of failure. In general, the diaphragm receives primary innervation at the C4 level, with contributions commonly seen from C3 and C5. In patients with a C4 complete spinal cord injury, diaphragm dysfunction continues for a long period, and failure to decannulate is common, as is death due to respiratory dysfunction.
There is an extremely high possibility of decannulation in C5–7 paralysis patients who can perform a shoulder shrug shortly after injury. Even in patients without this ability at that time, if their condition improves enough to allow them to perform a shoulder shrug within 3 weeks after injury, there is still a high possibility of successful decannulation. We chose 3 weeks after surgery because there were no patients who became able to shrug their shoulders after 3 weeks. Two of the seven patients, who could not shrug their shoulders at the initial hospitalization, had gained the ability to perform the shoulder shrug at 3 weeks after spinal cord injury. Because of the small number of cases in this study, we should further study the characteristics of the patients with decannulation prospectively in a larger number of cases.
Several limitations need to be considered with respect to our study. First, this study was a single-center design and involved only a limited number of patients. The incidence of a co-existing notable head injury was low. If the severity of the head injury was great, there was the possibility that brain injury influenced the outcome. Second, this retrospective study design might influence our results. Third, there is a possibility that shoulder shrug by itself does not necessarily indicate a lower level of neurological function with intact C4 phrenicus function. There is variability of nerve root and nerve level. Fourth, the results could have been affected by the method of surgery. All patients were treated using posterior approaches employing the pedicle screw system. A benefit of cervical pedicle screw fixation is that it has been shown to utilize the most stable cervical fixation instrumentation [17, 18]. Earlier ambulation and rehabilitation (including the respiratory system) without a cervical collar soon after the removal of the suction drain could be possible as a result of the greater stability. Rehabilitation without a cervical collar provides great merits for patients with tracheal tubes. This positive respiratory rehabilitation might be one of the positive factors for decannulation. On the other hand, the cervical pedicle screw system is also considered a serious risk to the surrounding structure: vertebral artery, spinal cord, and nerve root [24]. Among the patients in this study, there were no spinal cord injuries, one transient root injury and one vertebral artery penetration; while these complications were thus not catastrophic in this study, experienced surgeons should nevertheless use the cervical pedicle screw system with the utmost of caution.
In conclusion, (1) in this study, the risk factors for tracheostomy after cervical spinal cord injury were found to be a history of smoking and complete paralysis irrespective of the level of injury. (2) High cervical level complete spinal cord injury (C1–4 ASIA A) was found to be a risk factor for the failure of decannulation. (3) Among patients with high cervical spinal cord injury, those who experienced sufficient improvement in their paralysis to allow them to perform a shoulder shrug within 3 weeks after injury were highly likely to undergo successful decannulation.
References
Allen BL, Ferguson RL, Lehmann TR, Thomas R, O’Brien RP (1982) A mechanistic classification of closed indirect fractures and dislocations of the lower cervical spine. Spine 7:1–27
Ball PA (2001) Critical care management of the patient with acute spinal cord injury. Spine 26:S27–S30
Berlly M, Shem K (2007) Respiratory management during the first five days after spinal cord injury. J Spinal Cord Med 30:309–318
Berney S, Stockton K, Berlowitz D, Denehy L (2006) Can early extubation and intensive physiotherapy decrease length of stay of acute quadriplegic patients in intensive care? A retrospective case control study. Physiother Res Int 7:14–22
Brook AD, Sherman G, Malen J, Kollef MH (2000) Early versus late tracheostomy in patients who require prolonged mechanical ventilation. Am J Crit Care 9:352–359
Branco BC, Plurad D, Green DJ, Inaba K, Lam L, Cestero R, Marko B, Demetrios D (2011) Incidence and clinical predictors for tracheostomy after cervical spinal cord injury: a National Trauma Databank review. J Trauma 70:111–115
Cheshire DJE (1964) Respiratory management in acute tetraplegia. Paraplegia 1:252–261
Chiodo AE, Scelza W, Forchheimer M (2008) Predictors of ventilator weaning in individuals with high cervical spinal cord injury. J Spinal Cord Med 31:72–77
Claxton AR, Wong DT, Chung F, Fehlings MG (1998) Predictors of hospital mortality and mechanical ventilation in patients with cervical spinal cord injury. Can J Anaesth 5:144–149
Como JJ, Sutton ER, McCunn M et al (2005) Characterizing the need for mechanical ventilation following cervical spinal cord injury with neurologic deficit. J Trauma 59:912–916
Fishburn MJ, Marino RJ, Ditunno JFJ (1990) Atelectasis and pneumonia in acute spinal cord injury. Arch Phys Med Rehabil 71:197–200
Gilony D, Gilboa D, Bulmstein T, Murad H, Talmi YP, Kronenberg J, Wolf M (2005) Effects of tracheostomy on well-being and body-image perceptions. Otolaryngol Head Neck Surg 133:366–371
Goettler CE, Fugo JR, Bard MR, Newell MA, Sagraves SG, Toschlog EA, Schenarts PJ, Rotondo MF (2006) Predicting the need for early tracheostomy: a multifactorial analysis of 992 intubated trauma patients. J Trauma 60:991–996
Hahimi NK, Ransom E, Nardone H, Redding N, Mirza N (2010) Quality of life and self-image in patients undergoing tracheostomy. Laryngoscope 120(Suppl 4):S196
Harrop JS, Sharan AD, Scheid EH Jr, Vaccaro AR, Przybylski GJ (2004) Tracheostomy placement in patients with complete cervical spinal cord injuries: American Spinal Injury Association Grade A. J Neurosurg 100(1 Suppl Spine):20–23
Kluger Y, Paul DB, Lucke J, Cox P, Colella JJ, Townsend RN, Raves JJ, Diamond DL (1996) Early tracheostomy in trauma patients. Eur J Emerg Med 3:95–101
Kotani Y, Cunningham BW, Abumi K et al (1994) Biomechanical analysis of cervical stabilization systems: an assessment of transpedicular screw fixation in the cervical spine. Spine 19:2529–2539
Kothe R, Ruther W, Schneider E et al (2004) Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine 29:1869–1875
Marino RJ, Barros T, Biering-Sorensen F et al (2003) International standards for neurological classification of spinal cord injury. J Spinal Cord Med 26(Suppl 1):S50–S56
Palmieri TL, Jackson W, Greenhalgh DG (2002) Benefits of early tracheostomy in severely burned children. Crit Care Med 30:922–924
Rodriguez JL, Steinberg SM, Luchetti FA, Gibbons KJ, Taheri PA, Flint LM (1990) Early tracheostomy for primary airway management in the surgical critical care setting. Surgery 108:655–659
Rogers DF, Barnes PJ (2006) Treatment of airway mucus hypersecretion. Ann Med 38:116–125
Yukawa Y, Kato F, Yoshihara H, Yanase M, Ito K (2006) Cervical pedicle screw fixation in 100 cases of unstable cervical injuries: pedicle axis views obtained using fluoroscopy. J Neurosurg Spine 5:488–493
Yukawa T, Kato F, Ito K et al (2009) Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J 18:1293–1299
Acknowledgments
The authors wish to thank Ms M Fujimoto for assistance with data collection.
Conflict of interest
The authors report no conflict of interest regarding the materials or methods used in this study or the findings specified in this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakashima, H., Yukawa, Y., Imagama, S. et al. Characterizing the need for tracheostomy placement and decannulation after cervical spinal cord injury. Eur Spine J 22, 1526–1532 (2013). https://doi.org/10.1007/s00586-013-2762-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2762-0