Abstract
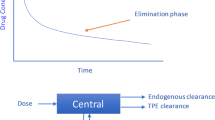
Extracorporeal circulation for the purpose of cardiopulmonary bypass (CPB) is used extensively for repair of cardiac defects. Complex mechanisms, many of which involve the generation of thrombin, are initiated by the institution of CPB. Thrombin is generated during CPB in spite of high doses of heparin. The tissue factor/factor VII pathway is also activated and is probably responsible for generation of most of the thrombin seen during CPB. Plasma proteins (humoral phase) along with platelets, endothelium and white cells (cellular phase) are also activated by contact of blood with synthetic surfaces. Small amounts of thrombin activate endothelial cells which then generate tissue plasminogen activator (t-PA). Plasmin is generated by the action of t-PA and fibrinolysis ensues. The blood becomes a mix of vasoactive substances that alter vascular smooth muscle tone and endothelial cell contraction. The sum of these reactions is called the ‘whole body inflammatory response’ and is responsible for postoperative morbidity including bleeding and organ system dysfunction.
Attempts to control the morbidity of CPB have focused on reversible inhibitors of some of the reactions described above. Potentially helpful new strategies may include: 1) enhanced production of thrombin-activatable fibrinolysis inhibitor (TAFI) to limit fibrinolysis, 2) synthesis of thrombin receptor blockers to limit platelet and endothelial activation, 3) protection of endothelial cell receptors during CPB, 4) control of CPB-induced platelet-PMN and endothelial-PMN adhesion in order to limit postoperative organ system dysfunction, and 5) limitation of tissue factor pathway activation in order to minimize thrombin production during CPB. This review highlights recent developments in the understanding of the molecular mechanisms of the action of thrombin induced by CPB.






Similar content being viewed by others
References
Abendschein DR, Recchia D, Meng YY, Oltrona L, Wickline SA, Eisenberg PR (1996) Inhibition of thrombin attenuates stenosis after arterial injury in minipigs. J Am Coll Cardiol 28:1849–1855
Abildgaard U, Lindahl AK, Sandset PM (1991) Heparin requires both antithrombin and extrinsic pathway inhibitor for its anticoagulant effect in human blood. Haemostasis 21:254–257
Adams MJ, Cardigan RA, Marchant WA, Grocott MP, Mythen MG, Mutch M, Purdy G, Mackie IJ, Machin SJ (2002) Tissue factor pathway inhibitor antigen and activity in 96 patients receiving heparin for cardiopulmonary bypass. J Cardiothorac Vasc Anesth 16:59–63
Aoki M, Jonas RA, Nomura F, Kawata H, Hickey PR (1995) Anti-CD18 attenuates deleterious effects of cardiopulmonary bypass and hypothermic circulatory arrest in piglets. J Card Surg 10:407–417
Asimakopoulos G, Lidington EA, Mason J, Haskard DO, Taylor KM, Landis RC (2001) Effect of aprotinin on endothelial cell activation. J Thorac Cardiovasc Surg 122:123–128
Bajzar L, Jain N, Wang P, Walker JB (2004) Thrombin activatable fibrinolysis inhibitor: not just an inhibitor of fibrinolysis. Crit Care Med 32:S320–324
Bajzar L, Manuel R, Nesheim ME (1995) Purification and characterization of TAFI, a thrombin-activable fibrinolysis inhibitor. J Biol Chem 270:14477–14484
Bajzar L, Morser J, Nesheim M (1996) TAFI, or plasma procarboxypeptidase B, couples the coagulation and fibrinolytic cascades through the thrombin-thrombomodulin complex. J Biol Chem 271:16603–16608
Bajzar L, Nesheim ME, Tracy PB (1996) The profibrinolytic effect of activated protein C in clots formed from plasma is TAFI-dependent. Blood 88:2093–2100
Bar-Shavit R, Kahn A, Fenton JW 2nd, Wilner GD (1983) Receptor-mediated chemotactic response of a macrophage cell line (J774) to thrombin. Lab Invest 49:702–707
Bernabei A, Gikakis N, Kowalska MA, Niewiarowski S, Edmunds LH Jr. (1995) Iloprost and echistatin protect platelets during simulated extracorporeal circulation. Ann Thorac Surg 59:149–153
Bertolino G, Locatelli A, Noris P, Maurelli M, Ceriana P, Mazzini G, Spedini P, Belletti S, Balduini CL (1996) Platelet composition and function in patients undergoing cardiopulmonary bypass for heart surgery. Haematologica 81:116–120
Bidstrup BP, Royston D, Sapsford RN, Taylor KM (1989) Reduction in blood loss and blood use after cardiopulmonary bypass with high dose aprotinin (Trasylol). J Thorac Cardiovasc Surg 97:364–372
Blauhut B, Gross C, Necek S, Doran JE, Spath P, Lundsgaard-Hansen P (1991) Effects of high-dose aprotinin on blood loss, platelet function, fibrinolysis, complement, and renal function after cardiopulmonary bypass. J Thorac Cardiovasc Surg 101:958–967
Blauhut B, Harringer W, Bettelheim P, Doran JE, Spath P, Lundsgaard-Hansen P (1994) Comparison of the effects of aprotinin and tranexamic acid on blood loss and related variables after cardiopulmonary bypass. J Thorac Cardiovasc Surg 108:1083–1091
Boisclair MD, Lane DA, Philippou H, Esnouf MP, Sheikh S, Hunt B, Smith KJ (1993) Mechanisms of thrombin generation during surgery and cardiopulmonary bypass. Blood 82:3350–3357
Boisclair MD, Lane DA, Philippou H, Sheikh S, Hunt B (1993) Thrombin production, inactivation and expression during open heart surgery measured by assays for activation fragments including a new ELISA for prothrombin fragment F1 + 2. Thromb Haemost 70:253–258
Boldt J (1998) Endothelial-related coagulation in pediatric surgery. Ann Thorac Surg 65:S56–59; discussion S74–56
Boldt J, Knothe C, Welters I, Dapper FL, Hempelmann G (1996) Normothermic versus hypothermic cardiopulmonary bypass: do changes in coagulation differ? Ann Thorac Surg 62:130–135
Boldt J, Schindler E, Knothe C, Welters I, Stertmann WA, Hempelmann G (1995) Endothelial-related coagulation in cardiac surgery. Br J Anaesth 74:174–179
Boldt J, Schindler E, Welters I, Wittstock M, Stertmann WA, Hempelmann G (1995) The effect of the anticoagulation regimen on endothelial-related coagulation in cardiac surgery patients. Anaesthesia 50:954–960
Borowiec J, Bagge L, Saldeen T, Thelin S (1997) Biocompatibility reflected by haemostasis variables during cardiopulmonary bypass using heparin-coated circuits. Thorac Cardiovasc Surg 45:163–167
Bouma BN, Meijers JC (2003) Thrombin-activatable fibrinolysis inhibitor (TAFI, plasma procarboxypeptidase B, procarboxypeptidase R, procarboxypeptidase U). J Thromb Haemost 1:1566–1574
Boyle EM Jr., Morgan EN, Kovacich JC, Canty TG Jr., Verrier ED (1999) Microvascular responses to cardiopulmonary bypass. J Cardiothorac Vasc Anesth 13:30–35; discussion 36–37
Braaten JV, Handt S, Jerome WG, Kirkpatrick J, Lewis JC, Hantgan RR (1993) Regulation of fibrinolysis by platelet-released plasminogen activator inhibitor 1: light scattering and ultrastructural examination of lysis of a model platelet-fibrin thrombus. Blood 81:1290–1299
Braaten JV, Jerome WG, Hantgan RR (1994) Uncoupling fibrin from integrin receptors hastens fibrinolysis at the platelet-fibrin interface. Blood 83:982–993
Brass LF, Molino M (1997) Protease-activated G protein-coupled receptors on human platelets and endothelial cells. Thromb Haemost 78:234–241
Brass LF, Pizarro S, Ahuja M, Belmonte E, Blanchard N, Stadel JM, Hoxie JA (1994) Changes in the structure and function of the human thrombin receptor during receptor activation, internalization, and recycling. J Biol Chem 269:2943–2952
Brister SJ, Ofosu FA, Buchanan MR (1993) Thrombin generation during cardiac surgery: is heparin the ideal anticoagulant? Thromb Haemost 70:259–262
Broze GJ Jr. (1995) Tissue factor pathway inhibitor and the current concept of blood coagulation. Blood Coagul Fibrinolysis 6(Suppl 1):S7–13
Broze GJ Jr. (1995) Tissue factor pathway inhibitor and the revised theory of coagulation. Annu Rev Med 46:103–112
Burman JF, Chung HI, Lane DA, Philippou H, Adami A, Lincoln JC (1994) Role of factor XII in thrombin generation and fibrinolysis during cardiopulmonary bypass. Lancet 344:1192–1193
Chandler WL, Fitch JC, Wall MH, Verrier ED, Cochran RP, Soltow LO, Spiess D (1995) Individual variations in the fibrinolytic response during and after cardiopulmonary bypass. Thromb Haemost 74:1293–1297
Chandler WL, Velan T (2003) Secretion of tissue plasminogen activator and plasminogen activator inhibitor 1 during cardiopulmonary bypass. Thromb Res 112:185–192
Chenoweth DE, Cooper SW, Hugli TE, Stewart RW, Blackstone EH, Kirklin JW (1981) Complement activation during cardiopulmonary bypass: evidence for generation of C3a and C5a anaphylatoxins. N Engl J Med 304:497–503
Chomiak PN, Walenga JM, Koza MJ, Reilly TM, Turlapathy P, Pifarre R (1993) Investigation of a thrombin inhibitor peptide as an alternative to heparin in cardiopulmonary bypass surgery. Circulation 88:II407–412
Chung JH, Gikakis N, Rao AK, Drake TA, Colman RW, Edmunds LH Jr. (1996) Pericardial blood activates the extrinsic coagulation pathway during clinical cardiopulmonary bypass. Circulation 93:2014–2018
Claeson G (1994) Synthetic peptides and peptidomimetics as substrates and inhibitors of thrombin and other proteases in the blood coagulation system. Blood Coagul Fibrinolysis 5:411–436
Cockell KA, Ren S, Sun J, Angel A, Shen GX (1995) Effect of thrombin on release of plasminogen activator inhibitor-1 from cultured primate arterial smooth muscle cells. Thromb Res 77:119–131
Cohen WM, Wu HF, Featherstone GL, Jenzano JW, Lundblad RL (1991) Linkage between blood coagulation and inflammation: stimulation of neutrophil tissue kallikrein by thrombin. Biochem Biophys Res Commun 176:315–320
Colotta F, Sciacca FL, Sironi M, Luini W, Rabiet MJ, Mantovani A (1994) Expression of monocyte chemotactic protein-1 by monocytes and endothelial cells exposed to thrombin. Am J Pathol 144:975–985
Connolly AJ, Ishihara H, Kahn ML, Farese RV, Jr., Coughlin SR (1996) Role of the thrombin receptor in development and evidence for a second receptor. Nature 381:516–519
Coughlin SR (1994) Molecular mechanisms of thrombin signaling. Semin Hematol 31:270–277
Coughlin SR (1993) Thrombin receptor structure and function. Thromb Haemost 70:184–187
Darrow AL, Fung-Leung WP, Ye RD, Santulli RJ, Cheung WM, Derian CK, Burns CL, Damiano BP, Zhou L, Keenan CM, Peterson PA, Andrade-Gordon P (1996) Biological consequences of thrombin receptor deficiency in mice. Thromb Haemost 76:860–866
Day JR, Punjabi PP, Randi AM, Haskard DO, Landis RC, Taylor KM (2004) Clinical inhibition of the seven-transmembrane thrombin receptor (PAR1) by intravenous aprotinin during cardiothoracic surgery. Circulation 110:2597–2600
De Marco L, Mazzucato M, Masotti A, Ruggeri ZM (1994) Localization and characterization of an alpha-thrombin-binding site on platelet glycoprotein Ib alpha. J Biol Chem 269:6478–6484
De SF, Van BY, Caes F, Francois K, Arnout J, Bossuyt X, Taeymans Y, Van NG (2002) Phosphorylcholine coating offers natural platelet preservation during cardiopulmonary bypass. Perfusion 17:39–44
de Smet AA, Joen MC, van Oeveren W, Roozendaal KJ, Harder MP, Eijsman L, Wildevuur CR (1990) Increased anticoagulation during cardiopulmonary bypass by aprotinin. J Thorac Cardiovasc Surg 100:520–527
DeAnda A Jr., Coutre SE, Moon MR, Vial CM, Griffin LC, Law VS, Komeda M, Leung LL, Miller DC (1994) Pilot study of the efficacy of a thrombin inhibitor for use during cardiopulmonary bypass. Ann Thorac Surg 58:344–350
Dietrich W, Barankay A, Dilthey G, Henze R, Niekau E, Sebening F, Richter JA (1989) Reduction of homologous blood requirement in cardiac surgery by intraoperative aprotinin application--clinical experience in 152 cardiac surgical patients. Thorac Cardiovasc Surg 37:92–98
Dietrich W, Dilthey G, Spannagl M, Jochum M, Braun SL, Richter JA (1995) Influence of high-dose aprotinin on anticoagulation, heparin requirement, and celite- and kaolin-activated clotting time in heparin-pretreated patients undergoing open-heart surgery. A double-blind, placebo-controlled study. Anesthesiology 83:679–689; discussion 629A–630A
Dietrich W, Spannagl M, Jochum M, Wendt P, Schramm W, Barankay A, Sebening F, Richter JA (1990) Influence of high-dose aprotinin treatment on blood loss and coagulation patterns in patients undergoing myocardial revascularization. Anesthesiology 73:1119–1126
Dietrich W, Spannagl M, Schramm W, Vogt W, Barankay A, Richter JA (1991) The influence of preoperative anticoagulation on heparin response during cardiopulmonary bypass. J Thorac Cardiovasc Surg 102:505–514
Duckro PN, Margolis RB, Tait RC, Korytnyk N (1985) Long-term follow-up of chronic pain patients: a preliminary study. Int J Psychiatry Med 15:283–292
Dumanian GA, Heil BV, Khouri RK, Hong C, Labadie K, Wun TC, Johnson PC (1996) Tissue factor and its inhibition at the human microvascular anastomosis. J Surg Res 60:263–269
Edmunds LH Jr., Niewiarowski S, Colman RW (1991) Invited letter concerning: aprotinin. J Thorac Cardiovasc Surg 101:1103–1104
Edwards JT, Hamby JK, Worrall NK (2003) Successful use of Argatroban as a heparin substitute during cardiopulmonary bypass: heparin-induced thrombocytopenia in a high-risk cardiac surgical patient. Ann Thorac Surg 75:1622–1624
Egeberg O (1965) On the natural blood coagulation inhibitor system. Investigations of inhibitor factors based on antithrombin deficient blood. Thromb Diath Haemorrh 14:473–489
Ehringer WD, Edwards MJ, Miller FN (1996) Mechanisms of alpha-thrombin, histamine, and bradykinin induced endothelial permeability. J Cell Physiol 167:562–569
Ehrlich HJ, Gebbink RK, Preissner KT, Keijer J, Esmon NL, Mertens K, Pannekoek H (1991) Thrombin neutralizes plasminogen activator inhibitor 1 (PAI-1) that is complexed with vitronectin in the endothelial cell matrix. J Cell Biol 115:1773–1781
Eichinger S, Schonauer V, Weltermann A, Minar E, Bialonczyk C, Hirschl M, Schneider B, Quehenberger P, Kyrle PA (2004) Thrombin-activatable fibrinolysis inhibitor and the risk for recurrent venous thromboembolism. Blood 103:3773–3776
Eisses MJ, Seidel K, Aldea GS, Chandler WL (2004) Reducing hemostatic activation during cardiopulmonary bypass: a combined approach. Anesth Analg 98:1208–1216, table of contents
Esmon CT (1995) Thrombomodulin as a model of molecular mechanisms that modulate protease specificity and function at the vessel surface. Faseb J 9:946–955
Evora PR, Pearson PJ, Schaff HV (1994) Impaired endothelium-dependent relaxation after coronary reperfusion injury: evidence for G-protein dysfunction. Ann Thorac Surg 57:1550–1556
Fagiano G, Parodi F, Brignolo C, Cordero G, Fabris E, Pagani L (1989) Prophylactic use of antithrombin III for protection of haemostatic balance in patients undergoing cardiopulmonary bypass. J Cardiothorac Anesth 3:87
Faint RW (1992) Platelet-neutrophil interactions: their significance. Blood Rev 6:83–91
Fareed J, Jeske W, Hoppensteadt D, Walenga JM, Pifarre R (1995) Drug interactions with aprotinin. In: Pifarre R (ed) Blood Conservation with Aprotinin. Hanley & Belfus, Inc., Philadelphia, PA, p 215–226
Ferraris VA, Ferraris SP (1995) Limiting excessive postoperative blood transfusion after cardiac procedures. A review. Tex Heart Inst J 22:216–230
Ferraris VA, Ferraris SP, Reich H, Rodriguez E, Huang M, Gupta A, Bennett JA, Andersen TT, Fenton JW 2nd (1996) Thrombin receptor-related hemostatic defect after cardiopulmonary bypass. Semin Thromb Hemost 22:351–356
Ferraris VA, Ferraris SP, Singh A, Fuhr W, Koppel D, McKenna D, Rodriguez E, Reich H (1998) The platelet thrombin receptor and postoperative bleeding. Ann Thorac Surg 65:352–358
Ferraris VA, Rodriguez E, Ferraris SP, Huang M, Gupta A, Bennett JA, Andersen TT, Dunn H, Fenton JW 2nd, Smith JB (1994) Platelet aggregation abnormalities after cardiopulmonary bypass. Blood 83:299–301
Friedman M, Wang SY, Sellke FW, Cohn WE, Weintraub RM, Johnson RG (1996) Neutrophil adhesion blockade with NPC 15669 decreases pulmonary injury after total cardiopulmonary bypass. J Thorac Cardiovasc Surg 111:460–468
Gabazza EC, Taguchi O, Kamada H, Hayashi T, Adachi Y, Suzuki K (2004) Progress in the understanding of protease-activated receptors. Int J Hematol 79:117–122
Garcia JG, Pavalko FM, Patterson CE (1995) Vascular endothelial cell activation and permeability responses to thrombin. Blood Coagul Fibrinolysis 6:609–626
Gerola LR, Buffolo E, Jasbik W, Botelho B, Bosco J, Brasil LA, Branco JN (2004) Off-pump versus on-pump myocardial revascularization in low-risk patients with one or two vessel disease: perioperative results in a multicenter randomized controlled trial. Ann Thorac Surg 77:569–573
Gikakis N, Khan MM, Hiramatsu Y, Gorman JH 3rd, Hack CE, Sun L, Rao AK, Niewiarowski S, Colman RW, Edmunds LH Jr. (1996) Effect of factor Xa inhibitors on thrombin formation and complement and neutrophil activation during in vitro extracorporeal circulation. Circulation 94:II341–346
Gillinov AM, Redmond JM, Winkelstein JA, Zehr KJ, Herskowitz A, Baumgartner WA, Cameron DE (1994) Complement and neutrophil activation during cardiopulmonary bypass: a study in the complement-deficient dog. Ann Thorac Surg 57:345–352
Gorman RC, Ziats N, Rao AK, Gikakis N, Sun L, Khan MM, Stenach N, Sapatnekar S, Chouhan V, Gorman JH 3rd, Niewiarowski S, Colman RW, Anderson JM, Edmunds LH Jr. (1996) Surface-bound heparin fails to reduce thrombin formation during clinical cardiopulmonary bypass. J Thorac Cardiovasc Surg 111:1–11; discussion 11–12
Gravlee GP (1995) Dermatan sulfate anticoagulation: future replacement for heparin? J Cardiothorac Vasc Anesth 9:237–239
Gravlee GP (1994) Heparin-coated cardiopulmonary bypass circuits. J Cardiothorac Vasc Anesth 8:213–222
Greco NJ, Jones GD, Tandon NN, Kornhauser R, Jackson B, Jamieson GA (1996) Differentiation of the two forms of GPIb functioning as receptors for alpha-thrombin and von Willebrand factor: Ca2+ responses of protease-treated human platelets activated with alpha-thrombin and the tethered ligand peptide. Biochemistry 35:915–921
Greco NJ, Tandon NN, Jones GD, Kornhauser R, Jackson B, Yamamoto N, Tanoue K, Jamieson GA (1996) Contributions of glycoprotein Ib and the seven transmembrane domain receptor to increases in platelet cytoplasmic [Ca2+] induced by alpha-thrombin. Biochemistry 35:906–914
Griffin CT, Srinivasan Y, Zheng YW, Huang W, Coughlin SR (2001) A role for thrombin receptor signaling in endothelial cells during embryonic development. Science 293:1666–1670
Harder MP, Eijsman L, Roozendaal KJ, van Oeveren W, Wildevuur CR (1991) Aprotinin reduces intraoperative and postoperative blood loss in membrane oxygenator cardiopulmonary bypass. Ann Thorac Surg 51:936–941
Harker LA, Malpass TW, Branson HE, Hessel EA 2nd, Slichter SJ (1980) Mechanism of abnormal bleeding in patients undergoing cardiopulmonary bypass: acquired transient platelet dysfunction associated with selective alpha-granule release. Blood 56:824–834
Hashimoto K, Yamagishi M, Sasaki T, Nakano M, Kurosawa H (1994) Heparin and antithrombin III levels during cardiopulmonary bypass: correlation with subclinical plasma coagulation. Ann Thorac Surg 58:799–804; discussion 804–795
Heller W, Wendel HP (1993) Clivarin and other LMWHs in an ex vivo cardiopulmonary bypass model. Studies on contact activation. Blood Coagul Fibrinolysis 4(Suppl 1):S45–54
Hirano K, Kanaide H (2003) Role of protease-activated receptors in the vascular system. J Atheroscler Thromb 10:211–225
Hoffman M, Monroe DM, Oliver JA, Roberts HR (1995) Factors IXa and Xa play distinct roles in tissue factor-dependent initiation of coagulation. Blood 86:1794–1801
Hollenberg MD (2003) Proteinase-mediated signaling: proteinase-activated receptors (PARs) and much more. Life Sci 74:237–246
Hravnak M, Hoffman LA, Saul MI, Zullo TG, Cuneo JF, Pellegrini RV (2004) Short-term complications and resource utilization in matched subjects after on-pump or off-pump primary isolated coronary artery bypass. Am J Crit Care 13:499–507; discussion 508
Inada E, Iwahashi K, Aoki K, Takanashi S, Kohama M, Aoki Y (1990) Changes of antithrombin III and antithrombin III-heparin complex levels, and ACT in cardiac surgery. Can J Anaesth 37:S75
Jang Y, Guzman LA, Lincoff AM, Gottsauner-Wolf M, Forudi F, Hart CE, Courtman DW, Ezban M, Ellis SG, Topol EJ (1995) Influence of blockade at specific levels of the coagulation cascade on restenosis in a rabbit atherosclerotic femoral artery injury model. Circulation 92:3041–3050
Jansen PG, te Velthuis H, Bulder ER, Paulus R, Scheltinga MR, Eijsman L, Wildevuur CR (1995) Reduction in prime volume attenuates the hyperdynamic response after cardiopulmonary bypass. Ann Thorac Surg 60:544–549; discussion 549–550
John LC, Rees GM, Kovacs IB (1993) Different anticoagulants and platelet reactivity in cardiac surgical patients. Ann Thorac Surg 56:899–902
Jordan RE, Oosta GM, Gardner WT, Rosenberg RD (1980) The kinetics of hemostatic enzyme-antithrombin interactions in the presence of low molecular weight heparin. J Biol Chem 255:10081–10090
Jung G, Razafindranaibe F, Elkouby A, Durasnel P, Panes F, Monassier JP (1995) Modifications of platelet shape change and ATP release during cardiopulmonary bypass. Haemostasis 25:149–157
Kaminishi Y, Hiramatsu Y, Watanabe Y, Yoshimura Y, Sakakibara Y (2004) Effects of nafamostat mesilate and minimal-dose aprotinin on blood-foreign surface interactions in cardiopulmonary bypass. Ann Thorac Surg 77:644–650
Kawasuji M, Ueyama K, Sakakibara N, Tedoriya T, Matsunaga Y, Misaki T, Watanabe Y (1993) Effect of low-dose aprotinin on coagulation and fibrinolysis in cardiopulmonary bypass. Ann Thorac Surg 55:1205–1209
Kestin AS, Valeri CR, Khuri SF, Loscalzo J, Ellis PA, MacGregor H, Birjiniuk V, Ouimet H, Pasche B, Nelson MJ, et al. (1993) The platelet function defect of cardiopulmonary bypass. Blood 82:107–117
Khuri SF, Valeri CR, Loscalzo J, Weinstein MJ, Birjiniuk V, Healey NA, MacGregor H, Doursounian M, Zolkewitz MA (1995) Heparin causes platelet dysfunction and induces fibrinolysis before cardiopulmonary bypass. Ann Thorac Surg 60:1008–1014
Kirklin JK, Blackstone EH, Kirklin JW (1987) Cardiopulmonary bypass: studies on its damaging effects. Blood Purif 5:168–178
Kirklin JK, Chenoweth DE, Naftel DC, Blackstone EH, Kirklin JW, Bitran DD, Curd JG, Reves JG, Samuelson PN (1986) Effects of protamine administration after cardiopulmonary bypass on complement, blood elements, and the hemodynamic state. Ann Thorac Surg 41:193–199
Kirklin JK, Westaby S, Blackstone EH, Kirklin JW, Chenoweth DE, Pacifico AD (1983) Complement and the damaging effects of cardiopulmonary bypass. J Thorac Cardiovasc Surg 86:845–857
Kojima T, Gando S, Kemmotsu O, Mashio H, Goda Y, Kawahigashi H, Watanabe N (2001) Another point of view on the mechanism of thrombin generation during cardiopulmonary bypass: role of tissue factor pathway inhibitor. J Cardiothorac Vasc Anesth 15:60–64
Komai H, Haworth SG (1996) Thrombomodulin and angiotensin-converting enzyme activity during pediatric open heart operations. Ann Thorac Surg 62:553–558
Korthuis RJ, Anderson DC, Granger DN (1994) Role of neutrophil-endothelial cell adhesion in inflammatory disorders. J Crit Care 9:47–71
Koster A, Chew D, Grundel M, Hausmann H, Grauhan O, Kuppe H, Spiess BD (2003) An assessment of different filter systems for extracorporeal elimination of bivalirudin: an in vitro study. Anesth Analg 96:1316–1319, table of contents
Koster A, Fischer T, Gruendel M, Mappes A, Kuebler WM, Bauer M, Kuppe H (2003) Management of heparin resistance during cardiopulmonary bypass: the effect of five different anticoagulation strategies on hemostatic activation. J Cardiothorac Vasc Anesth 17:171–175
Koster A, Spiess B, Chew DP, Krabatsch T, Tambeur L, DeAnda A, Hetzer R, Kuppe H, Smedira NG, Lincoff AM (2004) Effectiveness of bivalirudin as a replacement for heparin during cardiopulmonary bypass in patients undergoing coronary artery bypass grafting. Am J Cardiol 93:356–359
Ku DD, Zaleski JK (1993) Receptor mechanism of thrombin-induced endothelium-dependent and endothelium-independent coronary vascular effects in dogs. J Cardiovasc Pharmacol 22:609–616
Landis RC, Haskard DO, Taylor KM (2001) New antiinflammatory and platelet-preserving effects of aprotinin. Ann Thorac Surg 72:S1808–1813
Lane DA, Ireland H, Olds RJ, Thein SL, Perry DJ, Aiach M (1991) Antithrombin III: a database of mutations. Thromb Haemost 66:657–661
Lefkovits J, Malycky JL, Rao JS, Hart CE, Plow EF, Topol EJ, Nicolini FA (1996) Selective inhibition of factor Xa is more efficient than factor VIIa-tissue factor complex blockade at facilitating coronary thrombolysis in the canine model. J Am Coll Cardiol 28:1858–1865
Lemmer JH Jr., Despotis GJ (2002) Antithrombin III concentrate to treat heparin resistance in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg 123:213–217
Lerner DJ, Chen M, Tram T, Coughlin SR (1996) Agonist recognition by proteinase-activated receptor 2 and thrombin receptor. Importance of extracellular loop interactions for receptor function. J Biol Chem 271:13943–13947
Levy JH (2004) Heparin resistance and antithrombin: should it still be called heparin resistance? J Cardiothorac Vasc Anesth 18:129–130
Lin PJ, Chang CH, Lee YS, Chou YY, Chu JJ, Chang JP, Hsieh MJ (1994) Acute endothelial reperfusion injury after coronary artery bypass grafting. Ann Thorac Surg 58:782–788
Linden MD, Schneider M, Baker S, Erber WN (2004) Decreased concentration of antithrombin after preoperative therapeutic heparin does not cause heparin resistance during cardiopulmonary bypass. J Cardiothorac Vasc Anesth 18:131–135
Lindholm L, Westerberg M, Bengtsson A, Ekroth R, Jensen E, Jeppsson A (2004) A closed perfusion system with heparin coating and centrifugal pump improves cardiopulmonary bypass biocompatibility in elderly patients. Ann Thorac Surg 78:2131–2138; discussion 2138
Liu B, Belboul A, Radberg G, Tengborn L, Dernevik L, Roberts D, William-Olsson G (1993) Effect of reduced aprotinin dosage on blood loss and use of blood products in patients undergoing cardiopulmonary bypass. Scand J Thorac Cardiovasc Surg 27:149–155
Lo B, Fijnheer R, Castigliego D, Borst C, Kalkman CJ, Nierich AP (2004) Activation of hemostasis after coronary artery bypass grafting with or without cardiopulmonary bypass. Anesth Analg 99:634–640, table of contents
Lundgren CH, Sawa H, Sobel BE, Fujii S (1994) Modulation of expression of monocyte/macrophage plasminogen activator activity and its implications for attenuation of vasculopathy. Circulation 90:1927–1934
Mack MJ, Brown P, Houser F, Katz M, Kugelmass A, Simon A, Battaglia S, Tarkington L, Culler S, Becker E (2004) On-pump versus off-pump coronary artery bypass surgery in a matched sample of women: a comparison of outcomes. Circulation 110:II1–6
Macnaughton PD, Braude S, Hunter DN, Denison DM, Evans TW (1992) Changes in lung function and pulmonary capillary permeability after cardiopulmonary bypass. Crit Care Med 20:1289–1294
Magazine HI, Butt O, Yaghoutiel HR (1996) Endothelin and nitric oxide release modulate aortic contraction to selected thrombin receptor agonists. Am J Physiol 270:C1815–1818
Magazine HI, King JM, Srivastava KD (1996) Protease activated receptors modulate aortic vascular tone. Int J Cardiol 53(Suppl):S75–80
Magazine HI, Srivastava KD (1996) Thrombin-induced vascular reactivity is modulated by ETB receptor-coupled nitric oxide release in rat aorta. Am J Physiol 271:C923–928
Maruyama Y, Maruyama I, Soejima Y (1994) Thrombin receptor agonist peptide decreases thrombomodulin activity in cultured human umbilical vein endothelial cells. Biochem Biophys Res Commun 199:1262–1269
Mathew JP, Rinder CS, Tracey JB, Auszura LA, O’Connor T, Davis E, Smith BR (1995) Acadesine inhibits neutrophil CD11b up-regulation in vitro and during in vivo cardiopulmonary bypass. J Thorac Cardiovasc Surg 109:448–456
McVey JH (1994) Tissue factor pathway. Baillieres Clin Haematol 7:469–484
Menasche P (1995) The inflammatory response to cardiopulmonary bypass and its impact on postoperative myocardial function. Curr Opin Cardiol 10:597–604
Morariu AM, Gu YJ, Huet RC, Siemons WA, Rakhorst G, Oeveren WV (2004) Red blood cell aggregation during cardiopulmonary bypass: a pathogenic cofactor in endothelial cell activation? Eur J Cardiothorac Surg 26:939–946
Morin A, Arvier MM, Doutremepuich F, Vigneron C (1990) Localization of the structural domain responsible for the chemotactic properties of thrombin on polymorphonuclear leukocytes. Thromb Res 60:33–42
Morita K, Ihnken K, Buckberg GD, Sherman MP, Ignarro LJ (1996) Pulmonary vasoconstriction due to impaired nitric oxide production after cardiopulmonary bypass. Ann Thorac Surg 61:1775–1780
Murohara T, Buerke M, Margiotta J, Ruan F, Igarashi Y, Hakomori S, Lefer AM (1995) Myocardial and endothelial protection by TMS in ischemia-reperfusion injury. Am J Physiol 269:H504–514
Murohara T, Margiotta J, Phillips LM, Paulson JC, DeFrees S, Zalipsky S, Guo LS, Lefer AM (1995) Cardioprotection by liposome-conjugated sialyl Lewisx-oligosaccharide in myocardial ischaemia and reperfusion injury. Cardiovasc Res 30:965–974
Neaud V, Duplantier JG, Mazzocco C, Kisiel W, Rosenbaum J (2004) Thrombin up-regulates tissue factor pathway inhibitor-2 synthesis through a cyclooxygenase-2-dependent, epidermal growth factor receptor-independent mechanism. J Biol Chem 279:5200–5206
Nilsen DW, Almdahl SM, Svensson B, Vaage J, Rasmussen K, Osterud B (1993) Lipopolysaccharide induced monocyte thromboplastin synthesis and coagulation responses in patients undergoing coronary bypass surgery after preoperative supplementation with n-3 fatty acids. Thromb Haemost 70:900–902
Novotny WF, Brown SG, Miletich JP, Rader DJ, Broze GJ Jr. (1991) Plasma antigen levels of the lipoprotein-associated coagulation inhibitor in patient samples. Blood 78:387–393
Novotny WF, Girard TJ, Miletich JP, Broze GJ Jr. (1988) Platelets secrete a coagulation inhibitor functionally and antigenically similar to the lipoprotein associated coagulation inhibitor. Blood 72:2020–2025
Nystedt S, Emilsson K, Wahlestedt C, Sundelin J (1994) Molecular cloning of a potential proteinase activated receptor. Proc Natl Acad Sci U S A 91:9208–9212
Nystedt S, Larsson AK, Aberg H, Sundelin J (1995) The mouse proteinase-activated receptor-2 cDNA and gene. Molecular cloning and functional expression. J Biol Chem 270:5950–5955
Ofosu FA (2003) Protease activated receptors 1 and 4 govern the responses of human platelets to thrombin. Transfus Apheresis Sci 28:265–268
Ohri SK, Paratt R, Becket JM, Brannan J, Hunt BJ, Taylor KM (1996) Genetically engineered serine protease inhibitor for hemostasis after cardiac operations. Ann Thorac Surg 61:1223–1230
Palatianos GM, Dewanjee MK, Smith W, Novak S, Hsu LC, Kapadvanjwala M, Sfakianakis GN, Kaiser GA (1991) Platelet preservation during cardiopulmonary bypass with iloprost and Duraflo-II heparin-coated surfaces. ASAIO Trans 37:620–622
Paramo JA, Rifon J, Llorens R, Casares J, Paloma MJ, Rocha E (1991) Intra- and postoperative fibrinolysis in patients undergoing cardiopulmonary bypass surgery. Haemostasis 21:58–64
Parratt R, Hunt BJ (1998) Direct activation of factor X by monocytes occurs during cardiopulmonary bypass. Br J Haematol 101:40–46
Petaja J, Peltola K, Sairanen H, Leijala M, Kekomaki R, Vahtera E, Siimes MA (1996) Fibrinolysis, antithrombin III, and protein C in neonates during cardiac operations. J Thorac Cardiovasc Surg 112:665–671
Philippou H, Davidson SJ, Mole MT, Pepper JR, Burman JF, Lane DA (1999) Two-chain factor VIIa generated in the pericardium during surgery with cardiopulmonary bypass : relationship to increased thrombin generation and heparin concentration. Arterioscler Thromb Vasc Biol 19:248–254
Piccardoni P, Evangelista V, Piccoli A, de Gaetano G, Walz A, Cerletti C (1996) Thrombin-activated human platelets release two NAP-2 variants that stimulate polymorphonuclear leukocytes. Thromb Haemost 76:780–785
Prager NA, Abendschein DR, McKenzie CR, Eisenberg PR (1995) Role of thrombin compared with factor Xa in the procoagulant activity of whole blood clots. Circulation 92:962–967
Rabiet MJ, Plantier JL, Rival Y, Genoux Y, Lampugnani MG, Dejana E (1996) Thrombin-induced increase in endothelial permeability is associated with changes in cell-to-cell junction organization. Arterioscler Thromb Vasc Biol 16:488–496
Racz MJ, Hannan EL, Isom OW, Subramanian VA, Jones RH, Gold JP, Ryan TJ, Hartman A, Culliford AT, Bennett E, Lancey RA, Rose EA (2004) A comparison of short- and long-term outcomes after off-pump and on-pump coronary artery bypass graft surgery with sternotomy. J Am Coll Cardiol 43:557–564
Ranucci M (2004) Gabexate mesilate and heparin responsiveness in coronary patients. Med Sci Monit 10:PI40–43
Ranucci M, Ditta A, Boncilli A, Cotza M, Carboni G, Brozzi S, Bonifazi C, Tiezzi A (2004) Determinants of antithrombin consumption in cardiac operations requiring cardiopulmonary bypass. Perfusion 19:47–52
Rapp JH, Pan XM, Ghermay A, Gazetas P, Brady SE, Reilly LM (1997) A blinded trial of local recombinant tissue factor pathway inhibitor versus either local or systemic heparin in a vein bypass model. J Vasc Surg 25:726–729
Ray MJ, Marsh NA, Hawson GA (1994) Relationship of fibrinolysis and platelet function to bleeding after cardiopulmonary bypass. Blood Coagul Fibrinolysis 5:679–685
Raza SL, Nehring LC, Shapiro SD, Cornelius LA (2000) Proteinase-activated receptor-1 regulation of macrophage elastase (MMP-12) secretion by serine proteinases. J Biol Chem 275:41243–41250
Regan LM, Stearns-Kurosawa DJ, Kurosawa S, Mollica J, Fukudome K, Esmon CT (1996) The endothelial cell protein C receptor. Inhibition of activated protein C anticoagulant function without modulation of reaction with proteinase inhibitors. J Biol Chem 271:17499–17503
Reston JT, Tregear SJ, Turkelson CM (2003) Meta-analysis of short-term and mid-term outcomes following off-pump coronary artery bypass grafting. Ann Thorac Surg 76:1510–1515
Rikitake K, Okazaki Y, Naito K, Ohtsubo S, Natsuaki M, Itoh T (2004) Heparinless cardiopulmonary bypass with argatroban in dogs. Eur J Cardiothorac Surg 25:819–824
Rinder CS, Fitch JC (1996) Amplification of the inflammatory response: adhesion molecules associated with platelet/white cell responses. J Cardiovasc Pharmacol 27:S6–S12
Rinder CS, Fontes M, Mathew JP, Rinder HM, Smith BR (2003) Neutrophil CD11b upregulation during cardiopulmonary bypass is associated with postoperative renal injury. Ann Thorac Surg 75:899–905
Rinder CS, Gaal D, Student LA, Smith BR (1994) Platelet-leukocyte activation and modulation of adhesion receptors in pediatric patients with congenital heart disease undergoing cardiopulmonary bypass. J Thorac Cardiovasc Surg 107:280–288
Rinder CS, Rinder HM, Smith BR, Fitch JC, Smith MJ, Tracey JB, Matis LA, Squinto SP, Rollins SA (1995) Blockade of C5a and C5b-9 generation inhibits leukocyte and platelet activation during extracorporeal circulation. J Clin Invest 96:1564–1572
Rinder HM, Tracey JL, Rinder CS, Leitenberg D, Smith BR (1994) Neutrophil but not monocyte activation inhibits P-selectin-mediated platelet adhesion. Thromb Haemost 72:750–756
Rosnoblet C, Vischer UM, Gerard RD, Irminger JC, Halban PA, Kruithof EK (1999) Storage of tissue-type plasminogen activator in Weibel-Palade bodies of human endothelial cells. Arterioscler Thromb Vasc Biol 19:1796–1803
Ruf W, Dorfleutner A, Riewald M (2003) Specificity of coagulation factor signaling. J Thromb Haemost 1:1495–1503
Rydholm H, Bostrom S, Eriksson E, Risberg B (1995) Complex intracellular signal transduction regulates tissue plasminogen activator (t-PA) and plasminogen activator inhibitor type-1 (PAI-1) synthesis in cultured human umbilical vein endothelium. Scand J Clin Lab Invest 55:323–330
Rydholm HE, Falk P, Eriksson E, Risberg B (1998) Thrombin signal transduction of the fibrinolytic system in human adult venous endothelium in vitro. Scand J Clin Lab Invest 58:347–352
Salvemini D, de Nucci G, Gryglewski RJ, Vane JR (1989) Human neutrophils and mononuclear cells inhibit platelet aggregation by releasing a nitric oxide-like factor. Proc Natl Acad Sci U S A 86:6328–6332
Sambrano GR, Weiss EJ, Zheng YW, Huang W, Coughlin SR (2001) Role of thrombin signalling in platelets in haemostasis and thrombosis. Nature 413:74–78
Sandset PM, Abildgaard U, Larsen ML (1988) Heparin induces release of extrinsic coagulation pathway inhibitor (EPI). Thromb Res 50:803–813
Santamaria A, Borrell M, Oliver A, Ortin R, Forner R, Coll I, Mateo J, Souto JC, Fontcuberta J (2004) Association of functional thrombin-activatable fibrinolysis inhibitor (TAFI) with conventional cardiovascular risk factors and its correlation with other hemostatic factors in a Spanish population. Am J Hematol 76:348–352
Seghaye MC, Grabitz RG, Duchateau J, Busse S, Dabritz S, Koch D, Alzen G, Hornchen H, Messmer BJ, Von Bernuth G (1996) Inflammatory reaction and capillary leak syndrome related to cardiopulmonary bypass in neonates undergoing cardiac operations. J Thorac Cardiovasc Surg 112:687–697
Sevinsky JR, Rao LV, Ruf W (1996) Ligand-induced protease receptor translocation into caveolae: a mechanism for regulating cell surface proteolysis of the tissue factor-dependent coagulation pathway. J Cell Biol 133:293–304
Shibamiya A, Tabuchi N, Chung J, Sunamori M, Koyama T (2004) Formation of tissue factor-bearing leukocytes during and after cardiopulmonary bypass. Thromb Haemost 92:124–131
Sinclair DG, Haslam PL, Quinlan GJ, Pepper JR, Evans TW (1995) The effect of cardiopulmonary bypass on intestinal and pulmonary endothelial permeability. Chest 108:718–724
Singh A, Doris J, Ferraris VA, Ferraris SP (1996) The cost of excessive postoperative blood transfusion after cardiac operations. Surg Forum 60:544–549
Slaughter TF, Mark JB, El-Moalem H, Hayward KA, Hilton AK, Hodgins LP, Greenberg CS (2001) Hemostatic effects of antithrombin III supplementation during cardiac surgery: results of a prospective randomized investigation. Blood Coagul Fibrinolysis 12:25–31
Soslau G, Class R, Morgan DA, Foster C, Lord ST, Marchese P, Ruggeri ZM (2001) Unique pathway of thrombin-induced platelet aggregation mediated by glycoprotein Ib. J Biol Chem 276:21173–21183
Speekenbrink RG, Wildevuur CR, Sturk A, Eijsman L (1996) Low-dose and high-dose aprotinin improve hemostasis in coronary operations. J Thorac Cardiovasc Surg 112:523–530
Spiess BD, Vocelka C, Cochran RP, Soltow L, Chandler WL (1998) Heparin-coated bypass circuits (Carmeda) suppress the release of tissue plasminogen activator during normothermic coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 12:299–304
Springer TA (1990) Adhesion receptors of the immune system. Nature 346:425–434
Straka Z, Widimsky P, Jirasek K, Stros P, Votava J, Vanek T, Brucek P, Kolesar M, Spacek R (2004) Off-pump versus on-pump coronary surgery: final results from a prospective randomized study PRAGUE-4. Ann Thorac Surg 77:789–793
Strukova SM (2001) Thrombin as a regulator of inflammation and reparative processes in tissues. Biochemistry (Mosc) 66:8–18
Sturk-Maquelin KN, Nieuwland R, Romijn FP, Eijsman L, Hack CE, Sturk A (2003) Pro- and non-coagulant forms of non-cell-bound tissue factor in vivo. J Thromb Haemost 1:1920–1926
Tait RC, Walker ID, Perry DJ, Islam SI, Daly ME, McCall F, Conkie JA, Carrell RW (1994) Prevalence of antithrombin deficiency in the healthy population. Br J Haematol 87:106–112
Tanaka K, Takao M, Yada I, Yuasa H, Kusagawa M, Deguchi K (1989) Alterations in coagulation and fibrinolysis associated with cardiopulmonary bypass during open heart surgery. J Cardiothorac Anesth 3:181–188
Tanaka K, Wada K, Morimoto T, Shomura S, Satoh T, Yada I, Yuasa H, Kusagawa M, Deguchi K (1989) The role of the protein C-thrombomodulin system in physiologic anticoagulation during cardiopulmonary bypass. ASAIO Trans 35:373–375
Tennenberg SD, Clardy CW, Bailey WW, Solomkin JS (1990) Complement activation and lung permeability during cardiopulmonary bypass. Ann Thorac Surg 50:597–601
Terrell MR, Walenga JM, Koza MJ, Pifarre R (1996) Efficacy of aprotinin with various anticoagulant agents in cardiopulmonary bypass. Ann Thorac Surg 62:506–511
Tesfamariam B, Allen GT, Normandin D, Antonaccio MJ (1993) Involvement of the "tethered ligand" receptor in thrombin-induced endothelium-mediated relaxations. Am J Physiol 265:H1744–1749
Teufelsbauer H, Proidl S, Havel M, Vukovich T (1992) Early activation of hemostasis during cardiopulmonary bypass: evidence for thrombin mediated hyperfibrinolysis. Thromb Haemost 68:250–252
Tobu M, Iqbal O, Fareed D, Chatha M, Hoppensteadt D, Bansal V, Fareed J (2004) Erythropoietin-induced thrombosis as a result of increased inflammation and thrombin activatable fibrinolytic inhibitor. Clin Appl Thromb Hemost 10:225–232
Turner-Gomes SO, Mitchell L, Williams WG, Andrew M (1994) Thrombin regulation in congenital heart disease after cardiopulmonary bypass operations. J Thorac Cardiovasc Surg 107:562–568
Ueno A, Murakami K, Yamanouchi K, Watanabe M, Kondo T (1996) Thrombin stimulates production of interleukin-8 in human umbilical vein endothelial cells. Immunology 88:76–81
Valen G, Eriksson E, Risberg B, Vaage J (1994) Fibrinolysis during cardiac surgery. Release of tissue plasminogen activator in arterial and coronary sinus blood. Eur J Cardiothorac Surg 8:324–330
Valen G, Owall A, Eriksson E, Kallner A, Risberg B, Vaage J (1997) Release of creatine kinase, troponin-T, and tissue plasminogen activator in arterial and coronary venous blood during coronary artery bypass surgery. Scand J Clin Lab Invest 57:85–93
Valles J, Santos MT, Marcus AJ, Safier LB, Broekman MJ, Islam N, Ullman HL, Aznar J (1993) Downregulation of human platelet reactivity by neutrophils. Participation of lipoxygenase derivatives and adhesive proteins. J Clin Invest 92:1357–1365
Vergnolle N, Ferazzini M, D’Andrea MR, Buddenkotte J, Steinhoff M (2003) Proteinase-activated receptors: novel signals for peripheral nerves. Trends Neurosci 26:496–500
Verrier ED, Shernan SK, Taylor KM, Van de Werf F, Newman MF, Chen JC, Carrier M, Haverich A, Malloy KJ, Adams PX, Todaro TG, Mojcik CF, Rollins SA, Levy JH (2004) Terminal complement blockade with pexelizumab during coronary artery bypass graft surgery requiring cardiopulmonary bypass: a randomized trial. Jama 291:2319–2327
von Segesser LK, Mueller X, Marty B, Horisberger J, Corno A (2001) Alternatives to unfractionated heparin for anticoagulation in cardiopulmonary bypass. Perfusion 16:411–416
Vu TK, Hung DT, Wheaton VI, Coughlin SR (1991) Molecular cloning of a functional thrombin receptor reveals a novel proteolytic mechanism of receptor activation. Cell 64:1057–1068
Wachtfogel YT, Harpel PC, Edmunds LH Jr., Colman RW (1989) Formation of C1s-C1-inhibitor, kallikrein-C1-inhibitor, and plasmin-alpha 2-plasmin-inhibitor complexes during cardiopulmonary bypass. Blood 73:468–471
Wachtfogel YT, Kucich U, Hack CE, Gluszko P, Niewiarowski S, Colman RW, Edmunds LH Jr. (1993) Aprotinin inhibits the contact, neutrophil, and platelet activation systems during simulated extracorporeal perfusion. J Thorac Cardiovasc Surg 106:1–9; discussion 9–10
Wang H, Reiser G (2003) Thrombin signaling in the brain: the role of protease-activated receptors. Biol Chem 384:193–202
Weiler H, Isermann BH (2003) Thrombomodulin. J Thromb Haemost 1:1515–1524
Welch M, Douglas JT, Smyth JV, Walker MG (1995) Systemic endotoxaemia and fibrinolysis during aortic surgery. Eur J Vasc Endovasc Surg 9:228–232
Welters I, Menges T, Ballesteros M, Knothe C, Ruwoldt R, Gorlach G, Hempelmann G (1998) Thrombin generation and activation of the thrombomodulin protein C system in open heart surgery depend on the underlying cardiac disease. Thromb Res 92:1–9
Winn MJ, Jain K, Ku DD (1993) Argatroban and inhibition of the vasomotor actions of thrombin. J Cardiovasc Pharmacol 22:754–760
Woolkalis MJ, DeMelfi TM J, Blanchard N, Hoxie JA, Brass LF (1995) Regulation of thrombin receptors on human umbilical vein endothelial cells. J Biol Chem 270:9868–9875
Wrighton CJ, Hofer-Warbinek R, Moll T, Eytner R, Bach FH, de Martin R (1996) Inhibition of endothelial cell activation by adenovirus-mediated expression of I kappa B alpha, an inhibitor of the transcription factor NF-kappa B. J Exp Med 183:1013–1022
Yamamoto N, Greco NJ, Barnard MR, Tanoue K, Yamazaki H, Jamieson GA, Michelson AD (1991) Glycoprotein Ib (GPIb)-dependent and GPIb-independent pathways of thrombin-induced platelet activation. Blood 77:1740–1748
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ferraris, V.A., Ferraris, S.P. Thrombin and Cardiopulmonary Bypass – A Paradigm for Evaluation of the Regulation of Hemostasis. Int J Angiol 14, 193–210 (2005). https://doi.org/10.1007/s00547-005-2016-z
Issue Date:
DOI: https://doi.org/10.1007/s00547-005-2016-z