Abstract
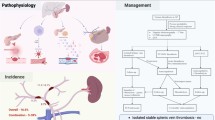
Deep venous thrombosis is a frequent, multifactorial disease and a leading cause of morbidity and mortality. Most of the time deep venous thrombosis is triggered by the interaction between acquired risk factors, such as hip fracture, pregnancy, and immobility, and hereditary risk factors such as thrombophilias. The mechanisms underlying deep venous thrombosis are not fully elucidated; however, in recent years, important advances have shed light on the role of venous flow, endothelium, platelets, leukocytes, and the interaction between inflammation and hemostasis. It has been described that the alteration of venous blood flow produces endothelial activation, favoring the adhesion of platelets and leukocytes, which, through tissue factor expression and neutrophil extracellular traps formation, contribute to the activation of coagulation, trapping more cells, such as red blood cells. Thus, the concerted interaction of these phenomena allows the formation and growth of the thrombus. In this work, the main mechanisms involved in the pathophysiology of deep vein thrombosis will be described.

Similar content being viewed by others
References
Jerjes-Sanchez C, Martinez-Sanchez C, Borrayo-Sanchez G, Carrillo-Calvillo J, Juarez-Herrera U, Quintanilla-Gutierrez J. Third national registry of acute coronary syndromes (RENASICA III). Archivos de Cardiologia de Mexico. 2015;85(3):207–14.
Wolberg AS, Rosendaal FR, Weitz JI, et al. Venous thrombosis. Nat Rev Disease Primers. 2015;1:15006.
Bruni-Fitzgerald KR. Venous thromboembolism: an overview. J Vascular Nurs Official Publ Soc Peripheral Vascular Nurs. 2015;33(3):95–9.
Nicolaides AN, Kakkar VV, Field ES, Renney JT. The origin of deep vein thrombosis: a venographic study. Br J Radiol. 1971;44(525):653–63.
Aird WC. Vascular bed-specific thrombosis. J Thrombosis Haemostasis: JTH. 2007;5(Suppl 1):283–91.
Raffini L, Huang YS, Witmer C, Feudtner C. Dramatic increase in venous thromboembolism in children’s hospitals in the United States from 2001 to 2007. Pediatrics. 2009;124(4):1001–8.
Centre-Acute N. Venous Thromboembolism: Reducing the Risk of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Patients Admitted to Hospital. London: Royal College of Physicians; 2010.
Cushman M. Epidemiology and risk factors for venous thrombosis. Semin Hematol. 2007;44(2):62–9.
Lindqvist P, Dahlback B, Marsal K. Thrombotic risk during pregnancy: a population study. Obstet Gynecol. 1999;94(4):595–9.
Jaffray J, Young G. Deep vein thrombosis in pediatric patients. Pediatric Blood Cancer. 2018; 65(3).
Koupenova M, Kehrel BE, Corkrey HA, Freedman JE. Thrombosis and platelets: an update. Eur Heart J. 2017;38(11):785–91.
Silverstein MD, Heit JA, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ 3rd. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158(6):585–93.
Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I9-16.
Pomp ER, Lenselink AM, Rosendaal FR, Doggen CJ. Pregnancy, the postpartum period and prothrombotic defects: risk of venous thrombosis in the MEGA study. J Thrombosis Haemostasis JTH. 2008;6(4):632–7.
Rosendaal FR, Reitsma PH. Genetics of venous thrombosis. J Thrombosis Haemostasis: JTH. 2009;7(Suppl 1):301–4.
Pomp ER, Doggen CJ, Vos HL, Reitsma PH, Rosendaal FR. Polymorphisms in the protein C gene as risk factor for venous thrombosis. Thromb Haemost. 2009;101(1):62–7.
Lindstrom S, Wang L, Smith EN, et al. Genomic and transcriptomic association studies identify 16 novel susceptibility loci for venous thromboembolism. Blood. 2019;134(19):1645–57.
Kushner A, West DW, Pillarisetty LS. Virchow Triad. StatPearls. Treasure Island (FL) 2020.
Panova-Noeva M, Wagner B, Nagler M, et al. Comprehensive platelet phenotyping supports the role of platelets in the pathogenesis of acute venous thromboembolism—results from clinical observation studies. EBioMedicine. 2020;60:102978.
Mackman N. New insights into the mechanisms of venous thrombosis. J Clin Investig. 2012;122(7):2331–6.
Brill A, Fuchs TA, Chauhan AK, et al. von Willebrand factor-mediated platelet adhesion is critical for deep vein thrombosis in mouse models. Blood. 2011;117(4):1400–7.
von Bruhl ML, Stark K, Steinhart A, et al. Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J Exp Med. 2012;209(4):819–35.
Pinsky DJ, Naka Y, Liao H, et al. Hypoxia-induced exocytosis of endothelial cell Weibel-Palade bodies. A mechanism for rapid neutrophil recruitment after cardiac preservation. J Clin Investig. 1996;97(2):493–500.
Sparkenbaugh EM, Chantrathammachart P, Wang S, et al. Excess of heme induces tissue factor-dependent activation of coagulation in mice. Haematologica. 2015;100(3):308–14.
Bergan JJ, Schmid-Schonbein GW, Smith PD, Nicolaides AN, Boisseau MR, Eklof B. Chronic venous disease. N Engl J Med. 2006;355(5):488–98.
Chiu JJ, Chien S. Effects of disturbed flow on vascular endothelium: pathophysiological basis and clinical perspectives. Physiol Rev. 2011;91(1):327–87.
Lurie F, Kistner RL, Eklof B, Kessler D. Mechanism of venous valve closure and role of the valve in circulation: a new concept. J Vasc Surg. 2003;38(5):955–61.
Traub O, Berk BC. Laminar shear stress: mechanisms by which endothelial cells transduce an atheroprotective force. Arterioscler Thromb Vasc Biol. 1998;18(5):677–85.
Yoshizumi M, Abe J, Tsuchiya K, Berk BC, Tamaki T. Stress and vascular responses: atheroprotective effect of laminar fluid shear stress in endothelial cells: possible role of mitogen-activated protein kinases. J Pharmacol Sci. 2003;91(3):172–6.
Chappell DC, Varner SE, Nerem RM, Medford RM, Alexander RW. Oscillatory shear stress stimulates adhesion molecule expression in cultured human endothelium. Circ Res. 1998;82(5):532–9.
Methe H, Balcells M, Alegret MdelC, et al. Vascular bed origin dictates flow pattern regulation of endothelial adhesion molecule expression. Am J Physiol Heart Circulatory Physiol. 2007;292(5):H2167–75.
Ono T, Bergan JJ, Schmid-Schonbein GW, Takase S. Monocyte infiltration into venous valves. J Vasc Surg. 1998;27(1):158–66.
Takase S, Pascarella L, Lerond L, Bergan JJ, Schmid-Schonbein GW. Venous hypertension, inflammation and valve remodeling. Eur J Vascular Endovascular Surg Official J Eur Soc Vascular Surg. 2004;28(5):484–93.
Bergan JJ. Chronic venous insufficiency and the therapeutic effects of Daflon 500 mg. Angiology. 2005;56(Suppl 1):S21–4.
Hamer JD, Malone PC, Silver IA. The PO2 in venous valve pockets: its possible bearing on thrombogenesis. Br J Surg. 1981;68(3):166–70.
Wolin MS, Ahmad M, Gupte SA. Oxidant and redox signaling in vascular oxygen sensing mechanisms: basic concepts, current controversies, and potential importance of cytosolic NADPH. Am J Physiol Lung Cell Mol Physiol. 2005;289(2):L159–73.
Chandel NS. Mitochondrial regulation of oxygen sensing. Adv Exp Med Biol. 2010;661:339–54.
Yan SF, Lu J, Zou YS, et al. Hypoxia-associated induction of early growth response-1 gene expression. J Biol Chem. 1999;274(21):15030–40.
Khachigian LM. Early growth response-1 in cardiovascular pathobiology. Circ Res. 2006;98(2):186–91.
Bovill EG, van der Vliet A. Venous valvular stasis-associated hypoxia and thrombosis: What is the link? Annu Rev Physiol. 2011;73:527–45.
Schindler U, Baichwal VR. Three NF-kappa B binding sites in the human E-selectin gene required for maximal tumor necrosis factor alpha-induced expression. Mol Cell Biol. 1994;14(9):5820–31.
Yan SF, Fujita T, Lu J, et al. Egr-1, a master switch coordinating upregulation of divergent gene families underlying ischemic stress. Nat Med. 2000;6(12):1355–61.
Chelombitko MA, Fedorov AV, Ilyinskaya OP, Zinovkin RA, Chernyak BV. Role of Reactive Oxygen Species in Mast Cell Degranulation. Biochemistry Biokhimiia. 2016;81(12):1564–77.
Ponomaryov T, Payne H, Fabritz L, Wagner DD, Brill A. Mast cells granular contents are crucial for deep vein thrombosis in mice. Circ Res. 2017;121(8):941–50.
Miki I, Kusano A, Ohta S, et al. Histamine enhanced the TNF-alpha-induced expression of E-selectin and ICAM-1 on vascular endothelial cells. Cell Immunol. 1996;171(2):285–8.
Erent M, Meli A, Moisoi N, et al. Rate, extent and concentration dependence of histamine-evoked Weibel-Palade body exocytosis determined from individual fusion events in human endothelial cells. J Physiol. 2007;583(Pt 1):195–212.
Steffel J, Akhmedov A, Greutert H, Luscher TF, Tanner FC. Histamine induces tissue factor expression: implications for acute coronary syndromes. Circulation. 2005;112(3):341–9.
Gross PL, Aird WC. The endothelium and thrombosis. Semin Thromb Hemost. 2000;26(5):463–78.
Bochenek ML, Schafer K. Role of endothelial cells in acute and chronic thrombosis. Hamostaseologie. 2019;39(2):128–39.
Rajendran P, Rengarajan T, Thangavel J, et al. The vascular endothelium and human diseases. Int J Biol Sci. 2013;9(10):1057–69.
Poredos P, Jezovnik MK. Endothelial dysfunction and venous thrombosis. Angiology. 2018;69(7):564–7.
Ramacciotti E, Myers DD Jr, Wrobleski SK, et al. P-selectin/ PSGL-1 inhibitors versus enoxaparin in the resolution of venous thrombosis: a meta-analysis. Thromb Res. 2010;125(4):e138–42.
Jezovnik MK, Fareed J, Poredos P. Patients With a History of Idiopathic Deep Venous Thrombosis Have Long-Term Increased Levels of Inflammatory Markers and Markers of Endothelial Damage. Clin Appl Thrombosis/Hemostasis Official J Int Acad Clin Appl Thrombosis/Hemostasis. 2017;23(2):124–31.
Poredos P, Jezovnik MK. In patients with idiopathic venous thrombosis, interleukin-10 is decreased and related to endothelial dysfunction. Heart Vessels. 2011;26(6):596–602.
Myers DD Jr. Pathophysiology of venous thrombosis. Phlebology. 2015;30(1 Suppl):7–13.
Bochenek ML, Schutz E, Schafer K. Endothelial cell senescence and thrombosis: ageing clots. Thromb Res. 2016;147:36–45.
Comi P, Chiaramonte R, Maier JA. Senescence-dependent regulation of type 1 plasminogen activator inhibitor in human vascular endothelial cells. Exp Cell Res. 1995;219(1):304–8.
Sato I, Kaji K, Morita I, Nagao M, Murota S. Augmentation of endothelin-1, prostacyclin and thromboxane A2 secretion associated with in vitro ageing in cultured human umbilical vein endothelial cells. Mech Ageing Dev. 1993;71(1–2):73–84.
Yanaka M, Honma T, Sato K, et al. Increased monocytic adhesion by senescence in human umbilical vein endothelial cells. Biosci Biotechnol Biochem. 2011;75(6):1098–103.
Hemmeryckx B, Emmerechts J, Bovill EG, Hoylaerts MF, Lijnen HR. Effect of ageing on the murine venous circulation. Histochem Cell Biol. 2012;137(4):537–46.
Budnik I, Brill A. Immune factors in deep vein thrombosis initiation. Trends Immunol. 2018;39(8):610–23.
Li WD, Li XQ. Endothelial progenitor cells accelerate the resolution of deep vein thrombosis. Vascul Pharmacol. 2016;83:10–6.
Dai B, Li L, Li Q, et al. Novel microspheres reduce the formation of deep venous thrombosis and repair the vascular wall in a rat model. Blood Coagulation Fibrinolysis Int J Haemostasis Thrombosis. 2017;28(5):398–406.
Wakefield TW, Myers DD, Henke PK. Role of selectins and fibrinolysis in VTE. Thromb Res. 2009;123(Suppl 4):S35-40.
Schulz C, Engelmann B, Massberg S. Crossroads of coagulation and innate immunity: the case of deep vein thrombosis. J Thrombosis Haemostasis: JTH. 2013;11(Suppl 1):233–41.
Palomo I, Pereira J, Palma J. HEMATOLOGÍA. Fisiopatología y Diagnóstico. 1st ed. Talca: Editorial Universidad de Talca; 2005.
Gremmel T, Frelinger AL 3rd, Michelson AD. Platelet Physiology. Semin Thromb Hemost. 2016;42(3):191–204.
Sorrentino S, Studt JD, Horev MB, Medalia O, Sapra KT. Toward correlating structure and mechanics of platelets. Cell Adh Migr. 2016;10(5):568–75.
Stone J, Hangge P, Albadawi H, et al. Deep vein thrombosis: pathogenesis, diagnosis, and medical management. Cardiovascular Diagnosis Therapy. 2017;7(Suppl 3):S276–84.
Takahashi M, Yamashita A, Moriguchi-Goto S, et al. Critical role of von Willebrand factor and platelet interaction in venous thromboembolism. Histol Histopathol. 2009;24(11):1391–8.
Kang C, Bonneau M, Brouland JP, Bal dit Sollier C, Drouet L. In vivo pig models of venous thrombosis mimicking human disease. Thrombosis and haemostasis. 2003;89(2):256–63.
Lehmann M, Schoeman RM, Krohl PJ, et al. Platelets Drive Thrombus Propagation in a Hematocrit and Glycoprotein VI-Dependent Manner in an In Vitro Venous Thrombosis Model. Arterioscler Thromb Vasc Biol. 2018;38(5):1052–62.
Heestermans M, Salloum-Asfar S, Streef T, et al. Mouse venous thrombosis upon silencing of anticoagulants depends on tissue factor and platelets, not FXII or neutrophils. Blood. 2019;133(19):2090–9.
Payne H, Ponomaryov T, Watson SP, Brill A. Mice with a deficiency in CLEC-2 are protected against deep vein thrombosis. Blood. 2017;129(14):2013–20.
Riedl J, Preusser M, Nazari PM, et al. Podoplanin expression in primary brain tumors induces platelet aggregation and increases risk of venous thromboembolism. Blood. 2017;129(13):1831–9.
Ding P, Zhang S, Yu M, et al. IL-17A promotes the formation of deep vein thrombosis in a mouse model. Int Immunopharmacol. 2018;57:132–8.
Subramaniam S, Jurk K, Hobohm L, et al. Distinct contributions of complement factors to platelet activation and fibrin formation in venous thrombus development. Blood. 2017;129(16):2291–302.
Reimers RC, Sutera SP, Joist JH. Potentiation by red blood cells of shear-induced platelet aggregation: relative importance of chemical and physical mechanisms. Blood. 1984;64(6):1200–6.
Goel MS, Diamond SL. Adhesion of normal erythrocytes at depressed venous shear rates to activated neutrophils, activated platelets, and fibrin polymerized from plasma. Blood. 2002;100(10):3797–803.
Muller F, Mutch NJ, Schenk WA, et al. Platelet polyphosphates are proinflammatory and procoagulant mediators in vivo. Cell. 2009;139(6):1143–56.
Reinhardt C, von Bruhl ML, Manukyan D, et al. Protein disulfide isomerase acts as an injury response signal that enhances fibrin generation via tissue factor activation. J Clin Investig. 2008;118(3):1110–22.
Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol. 2013;13(1):34–45.
Setiadi H, Yago T, Liu Z, McEver RP. Endothelial signaling by neutrophil-released oncostatin M enhances P-selectin-dependent inflammation and thrombosis. Blood Adv. 2019;3(2):168–83.
Brinkmann V, Reichard U, Goosmann C, et al. Neutrophil extracellular traps kill bacteria. Science. 2004;303(5663):1532–5.
Papayannopoulos V, Zychlinsky A. NETs: a new strategy for using old weapons. Trends Immunol. 2009;30(11):513–21.
Wang Y, Gao H, Shi C, et al. Leukocyte integrin Mac-1 regulates thrombosis via interaction with platelet GPIbalpha. Nat Commun. 2017;8:15559.
Dyer MR, Chen Q, Haldeman S, et al. Deep vein thrombosis in mice is regulated by platelet HMGB1 through release of neutrophil-extracellular traps and DNA. Sci Rep. 2018;8(1):2068.
Fuchs TA, Brill A, Duerschmied D, et al. Extracellular DNA traps promote thrombosis. Proc Natl Acad Sci USA. 2010;107(36):15880–5.
Martinod K, Wagner DD. Thrombosis: tangled up in NETs. Blood. 2014;123(18):2768–76.
Brill A, Fuchs TA, Savchenko AS, et al. Neutrophil extracellular traps promote deep vein thrombosis in mice. J Thrombosis Haemostasis: JTH. 2012;10(1):136–44.
Semeraro F, Ammollo CT, Morrissey JH, et al. Extracellular histones promote thrombin generation through platelet-dependent mechanisms: involvement of platelet TLR2 and TLR4. Blood. 2011;118(7):1952–61.
Massberg S, Grahl L, von Bruehl ML, et al. Reciprocal coupling of coagulation and innate immunity via neutrophil serine proteases. Nat Med. 2010;16(8):887–96.
Ramacciotti E, Hawley AE, Farris DM, et al. Leukocyte- and platelet-derived microparticles correlate with thrombus weight and tissue factor activity in an experimental mouse model of venous thrombosis. Thromb Haemost. 2009;101(4):748–54.
Pfeiler S, Stark K, Massberg S, Engelmann B. Propagation of thrombosis by neutrophils and extracellular nucleosome networks. Haematologica. 2017;102(2):206–13.
Weitz JI. Factor XI and factor XII as targets for new anticoagulants. Thromb Res. 2016;141(Suppl 2):S40–5.
Salomon O, Steinberg DM, Zucker M, Varon D, Zivelin A, Seligsohn U. Patients with severe factor XI deficiency have a reduced incidence of deep-vein thrombosis. Thromb Haemost. 2011;105(2):269–73.
Buller HR, Bethune C, Bhanot S, et al. Factor XI antisense oligonucleotide for prevention of venous thrombosis. N Engl J Med. 2015;372(3):232–40.
Verhamme P, Yi BA, Segers A, et al. Abelacimab for Prevention of Venous Thromboembolism. N Engl J Med. 2021;385(7):609–17.
Kool RO, Kohler HP, Coutinho JM, et al. Coagulation factor XIII-A subunit and activation peptide levels in individuals with established symptomatic acute deep vein thrombosis. Thromb Res. 2017;159:96–9.
Walton BL, Byrnes JR, Wolberg AS. Fibrinogen, red blood cells, and factor XIII in venous thrombosis. J Thrombosis Haemostasis: JTH. 2015;13(Suppl 1):S208–15.
Aleman MM, Walton BL, Byrnes JR, Wolberg AS. Fibrinogen and red blood cells in venous thrombosis. Thromb Res. 2014;133(Suppl 1):S38-40.
Whelihan MF, Lim MY, Mooberry MJ, et al. Thrombin generation and cell-dependent hypercoagulability in sickle cell disease. J Thrombosis Haemostasis: JTH. 2016;14(10):1941–52.
Saghazadeh A, Hafizi S, Rezaei N. Inflammation in venous thromboembolism: Cause or consequence? Int Immunopharmacol. 2015;28(1):655–65.
Bertin FR, Rys RN, Mathieu C, Laurance S, Lemarie CA, Blostein MD. Natural killer cells induce neutrophil extracellular trap formation in venous thrombosis. J Thrombosis Haemostasis JTH. 2019;17(2):403–14.
Nosaka M, Ishida Y, Kimura A, et al. Absence of IFN-gamma accelerates thrombus resolution through enhanced MMP-9 and VEGF expression in mice. J Clin Investig. 2011;121(7):2911–20.
Zhang Y, Zhang Z, Wei R, et al. IL (Interleukin)-6 Contributes to Deep Vein Thrombosis and Is Negatively Regulated by miR-338-5p. Arterioscler Thromb Vasc Biol. 2020;40(2):323–34.
Mo JW, Zhang DF, Ji GL, Liu XZ, Fan B. Detection of targets and their mechanisms for early diagnosis of traumatic deep vein thrombosis. Genetics Moler Research GMR. 2015;14(1):2413–21.
Gupta N, Sahu A, Prabhakar A, et al. Activation of NLRP3 inflammasome complex potentiates venous thrombosis in response to hypoxia. Proc Natl Acad Sci USA. 2017;114(18):4763–8.
Nosaka M, Ishida Y, Kimura A, et al. Contribution of the TNF-alpha (Tumor Necrosis Factor-alpha)-TNF-Rp55 (Tumor Necrosis Factor Receptor p55) Axis in the Resolution of Venous Thrombus. Arterioscler Thromb Vasc Biol. 2018;38(11):2638–50.
Mo JW, Zhang DF, Ji GL, Liu XZ, Fan B. TGF-beta1 and Serpine 1 expression changes in traumatic deep vein thrombosis. Genetics Mole Res GMR. 2015;14(4):13835–42.
Henke PK, Wakefield TW, Kadell AM, et al. Interleukin-8 administration enhances venous thrombosis resolution in a rat model. J Surg Res. 2001;99(1):84–91.
Yago T, Liu Z, Ahamed J, McEver RP. Cooperative PSGL-1 and CXCR2 signaling in neutrophils promotes deep vein thrombosis in mice. Blood. 2018;132(13):1426–37.
Laurance S, Bertin FR, Ebrahimian T, et al. Gas6 Promotes Inflammatory (CCR2(hi)CX3CR1(lo)) Monocyte Recruitment in Venous Thrombosis. Arterioscler Thromb Vasc Biol. 2017;37(7):1315–22.
Qin J, Liang H, Shi D, et al. A panel of microRNAs as a new biomarkers for the detection of deep vein thrombosis. J Thromb Thrombolysis. 2015;39(2):215–21.
Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116(2):281–97.
Soifer HS, Rossi JJ, Saetrom P. MicroRNAs in disease and potential therapeutic applications. Mole Therapy J Am Soc Gene Therapy. 2007;15(12):2070–9.
Latronico MV, Catalucci D, Condorelli G. Emerging role of microRNAs in cardiovascular biology. Circ Res. 2007;101(12):1225–36.
Jin J, Wang C, Ouyang Y, Zhang D. Elevated miR-195-5p expression in deep vein thrombosis and mechanism of action in the regulation of vascular endothelial cell physiology. Exp Ther Med. 2019;18(6):4617–24.
Kong L, Hu N, Du X, et al. Upregulation of miR-483-3p contributes to endothelial progenitor cells dysfunction in deep vein thrombosis patients via SRF. J Transl Med. 2016;14:23.
Zhang Y, Miao X, Zhang Z, et al. miR-374b-5p is increased in deep vein thrombosis and negatively targets IL-10. J Mol Cell Cardiol. 2020;144:97–108.
Kong L, Du X, Hu N, et al. Downregulation of let-7e-5p contributes to endothelial progenitor cell dysfunction in deep vein thrombosis via targeting FASLG. Thromb Res. 2016;138:30–6.
Li Z, Ni J. Role of microRNA-26a in the diagnosis of lower extremity deep vein thrombosis in patients with bone trauma. Exp Ther Med. 2017;14(5):5069–74.
Sun S, Chai S, Zhang F, Lu L. Overexpressed microRNA-103a-3p inhibits acute lower-extremity deep venous thrombosis via inhibition of CXCL12. IUBMB Life. 2020;72(3):492–504.
Zhang P, Zhao Q, Gong K, et al. Downregulation of miR-103a-3p contributes to endothelial progenitor cell dysfunction in deep vein thrombosis through PTEN targeting. Ann Vasc Surg. 2020;64:339–46.
Morelli VM, Braekkan SK, Hansen JB. Role of microRNAs in Venous Thromboembolism. Int J Mole Sci. 2020;21(7).
Hembrom AA, Srivastava S, Garg I, Kumar B. MicroRNAs in venous thrombo-embolism. Clinica chimica acta; Int J Clin Chem. 2020;504:66–72.
Funding
No specific financial support was used for the preparation of this article.
Author information
Authors and Affiliations
Contributions
IP and SN contributed to idea conception. SN and CS participated in writing the manuscript. RT, JP, EF, and IP contributed critical revision of the article. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Navarrete, S., Solar, C., Tapia, R. et al. Pathophysiology of deep vein thrombosis. Clin Exp Med 23, 645–654 (2023). https://doi.org/10.1007/s10238-022-00829-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-022-00829-w