Abstract
Purpose
This study was performed to evaluate the changes in oxygen supply–demand balance during induction of general anesthesia using an indirect calorimeter capable of measuring oxygen consumption (VO2) and carbon dioxide production (VCO2).
Methods
This study included patients scheduled for surgery in whom remimazolam was administered as a general anesthetic. VO2 and VCO2 were measured at different intervals: upon awakening (T1), 15 min after tracheal intubation (T2), and 1 h after T2 (T3). Oxygen delivery (DO2) was calculated simultaneously with these measurements. VO2 was ascertained using an indirect calorimeter and further calculated using vital signs, among other factors. DO2 was derived from cardiac output and arterial blood gas analysis performed with an arterial pressure-based cardiac output measurement system.
Results
VO2, VCO2, and DO2 decreased significantly from T1 to T2 and T3 [VO2/body surface area (BSA) (ml/min/m2): T1, 130 (122–146); T2, 107 (83–139); T3, 97 (93–121); p = 0.011], [VCO2/BSA (ml/min/m2): T1, 115 (105–129); T2, 90 (71–107); T3, 81 (69–101); p = 0.011], [DO2/BSA (ml/min/m2): T1, 467 (395–582); T2, 347 (286–392); T3, 382 (238–414); p = 0.0020]. Among the study subjects, a subset exhibited minimal reduction in VCO2. Although the respiratory frequency was titrated on the basis of end-tidal CO2 levels, there was no significant difference between the groups.
Conclusion
General anesthetic induction with remimazolam decreased VO2, VCO2, and DO2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A key objective in anesthesia and intensive care is preservation of oxygen homeostasis [1]. Administration of general anesthesia transfers homeostasis regulation from the patient’s innate physiological regulatory mechanisms to the anesthesiologist. Therefore, careful control of anesthetic procedures, particularly systemic management of general anesthetics, is necessary. When oxygen delivery (DO2) to tissues decreases, in vivo mechanisms that regulate the oxygen-carrying capacity [2] and shut down unneeded cellular operations are activated [3]. However, when tissue oxygen levels fall below a particular threshold, malfunction of intracellular metabolic processes may result in life-threatening shock [4, 5].
DO2 to tissues is proportional to the product of arterial blood oxygen content and cardiac output [6]. Critical DO2 levels [DO2(crit)] are those that cause cellular and organ malfunction and irreversible alterations that can lead to cell death [7, 8]. There is no definitive standard for DO2(crit). Oxygen consumption (VO2) in vivo is independent of DO2 over a broad range of values because the oxygen extraction rate (ERO2), representing the ratio of VO2 to DO2, can accommodate changes in DO2 [9]. However, when oxygen supply falls below DO2(crit), cellular oxygen utilization becomes dependent on the oxygen supply [10, 11].
The balance of oxygen supply is not solely dependent on the amount of oxygen delivered. The effect of carbon dioxide produced by tissue metabolism (VCO2) also plays a role. Further increases in VCO2 can lead to greater increases in the partial pressure of carbon dioxide, potentially resulting in acidosis. The carbon dioxide dissociation curve changes with alterations in base excess, hemoglobin concentration, and oxygen saturation (Haldane effect), as outlined in a previous report [12]. These factors can alter the venoarterial difference in carbon dioxide tension, even without changes in the R/Q (VCO2/VO2) or tissue oxygenation [13].
During induction of general anesthesia, rapid changes occur in the patient’s hemodynamic and respiratory condition [14]. Anesthetic-induced circulatory depression decreases cardiac output and DO2, whereas sedative medications [15], muscle relaxants [16], and changes in body temperature influence VO2 [17]. Consequently, both DO2 and VO2 drop during general anesthesia, but their effects and associations are unknown [18].
Selection of medications is a crucial aspect of anesthetic management. Remimazolam is an ultrashort-acting sedative/anesthetic benzodiazepine agonist with high affinity for the benzodiazepine-binding site on the gamma-aminobutyric acid receptor. This drug is characterized by the safety of benzodiazepines (hemodynamic stability) and excellent controllability (quick induction of anesthesia and recovery of cognitive functions) [19,20,21].
Hypotensive episodes requiring vasoconstrictor treatment during general anesthesia can influence the oxygen supply–demand balance [22,23,24]. DO2 and VO2 during general anesthesia may have been exaggerated in prior studies that reported the balance between oxygen supply and demand, as the use of drugs that increase blood pressure may have increased oxygen supply and oxygen consumption, which could have been overestimated. Therefore, we expected that using remimazolam, which is more hemodynamically stable than typical general anesthetics [25], would facilitate analysis of alterations in the oxygen supply–demand balance generated by general anesthesia without vasoconstrictor treatment.
We conducted an exploratory investigation to determine the effects of remimazolam on the balance between oxygen supply and demand during general anesthetic induction by monitoring VO2, VCO2, and DO2. Our objective was twofold: first, to determine the impact of remimazolam on the balance between DO2 and VO2 during general anesthetic induction; and second, to explore the in vivo changes associated with changes in the oxygen supply–demand balance during arousal and after the induction of general anesthesia.
Methods
This research was approved by Yamagata University School of Medicine Ethics Review Board (Approval No. 2020–375; Approval Date: April 7, 2021). All participants provided written informed consent. Before study commencement, registration in the University Hospital Medical Information Network was completed (Study ID: UMIN000043879; Reception Number: R000050079; Publication Date: April 10, 2021).
The participants were surgical patients who underwent general anesthesia with intubation in our institution. The eligibility requirement was an age of 18–85 years. The exclusion criteria were allergy to any component of remimazolam; history of central nervous system disease (e.g., cerebral infarction or hemorrhage), neuromuscular disease (e.g., myasthenia gravis), uncontrolled heart or respiratory failure, renal failure (serum creatinine ≥ 2 mg/dl), or liver failure (aspartate transaminase/alanine transaminase ratio 2.5 × the upper limit of normal); and inability to provide informed consent. Patients requiring postural adjustment or isolated lung ventilation, those undergoing head-and-neck surgery and emergency procedures, and those with hemorrhage that might influence cardiac performance were also excluded. Patients receiving epidural anesthesia were not excluded.
Anesthetic management and monitoring
A transcutaneous oxygen saturation monitor, electrocardiogram device, noninvasive arterial pressure monitor, bispectral index (BIS) monitor (BIS XP; Aspect Medical Systems, Newton, MA, USA), and peripheral venous and arterial lines were applied upon entering the operating room. Before general anesthetic induction, the supraorbital forehead temperature was recorded using a zero-heat-flux (ZHF) thermometer (SpotOn; 3 M, Saint Paul, MN, USA). After general anesthetic induction, a urethral catheter with a bladder temperature sensor (BARD Silver TSC Tray; Becton, Dickinson and Company, Franklin Lakes, NJ, USA) was placed.
Before anesthetic induction, VO2 and VCO2 were measured with an indirect calorimeter (CCM Express; MGC Diagnostics, Saint Paul, MN, USA), and oxygen supply was simultaneously estimated (T1). Following preoxygenation, remifentanil (0.2–0.5 μg/kg/min) and remimazolam (Anerem 50 mg; Mundipharma K.K., Tokyo, Japan) (12 mg/kg/h) were administered. Upon confirming loss of consciousness, the remimazolam dose was lowered to 1.0 mg/kg/h and subsequently adjusted to maintain a BIS of 40–60. Rocuronium was administered at 0.8 mg/kg, followed by intubation 2–3 min later. Post-intubation, the remifentanil dosage was decreased to 0.1 μg/kg/min and maintained. In addition, the dose of remifentanil was increased to 0.2–0.4 μg/kg/min after T2 and maintained until surgery. The body surface heating system was set to 38 °C in areas not covered by the surgical field. The heating device was not applied above the patient’s neck. The crystalloid solution administration speed was not changed from T1–T3.
Systolic arterial pressure of < 80 mmHg was defined as hypotension. For hypotension, 0.1 mg of phenylephrine and 4 mg of ephedrine were administered when the pulse rate was ≥ 80 and ≤ 79 beats/min, respectively. These participants were excluded from the study.
Inspiratory oxygenation was set to 45%, the tidal volume for ventilation was 8 ml/kg [male body weight (kg): 50 + 0.91(height (cm) − 152.4); female body weight (kg): 45.5 + 0.91(height (cm) − 152.4)] [26], the end-expiratory positive-pressure ventilation was 5 cmH2O, and the respiratory rate was adjusted to an end-tidal carbon dioxide concentration of 35–40 mmHg. A Perseus A500 ventilator (Dräger, Lübeck, Germany) was used.
Using an indirect calorimeter, the metabolic rate was assessed 15 min after tracheal intubation and stabilization of the hemodynamic and respiratory state (T2), and again 1 h after T2 (T3).
The oxygen supply–demand balance was determined using the indirect calorimeter measurements of VO2 and VCO2. The indirect calorimeter measured VO2 and VCO2 based on the oxygen or carbon dioxide concentration and the breathing rate for inspiratory and expiratory air [27].
Cardiac output was measured with a FloTrac (Edwards Lifesciences, Irvine, CA, USA) and combined with the arterial blood gas measurements to calculate DO2 as follows [7]:
DO2 = [1.34 × Hb × SaO2 + (0.003 × PaO2)] × cardiac output × 10,
where Hb is hemoglobin (g/dl), SaO2 is arterial oxyhemoglobin saturation (%), and PaO2 is arterial oxygen tension (mmHg). The cardiac output measured by the FloTrac was calculated as the product of stroke volume and heart rate.
When the respiratory and circulatory dynamics were steady, measurements were collected once, and the 3 min mean of the measurements was used. The variables are displayed as median (interquartile range).
Outcomes
The primary endpoint was the changes in VO2 and VCO2 evaluated by indirect calorimetry before and after general anesthetic induction, as well as DO2 derived from cardiac output.
The secondary endpoints included various vital signs, such as blood pressure, heart rate, cardiac output, and BIS. We also studied indices of the oxygen supply–demand balance before and after general anesthetic induction, namely ERO2, R/Q, double product (heart rate × systemic blood pressure) [28], and VO2 using the LaFarge–Miettinen prediction equation (LMVO2) for men and women [men: LMVO2/body surface area (BSA) = 138.1 − (11.19 × log age) + (0.378 × heart rate), women: LMVO2/BSA = 138.1 − (17.04 × log age) + (0.378 × heart rate)] [29].
Patients were divided into two cohorts on the basis of VCO2 values at T2, which is a metabolic byproduct and indicator of respiratory function [30]. VCO2 per body surface area of 96.3 ml/min/m2 was defined as the boundary value, with patients exceeding this value comprising the high VCO2 group and those below this value comprising the low VCO2 group. This boundary value was determined from the resting VO2 value [31], the predicted decrease in VO2 under general anesthesia [23], and a respiratory quotient of 1. The cohort division aimed to elucidate differences in oxygen metabolic parameters, such as VO2 and VCO2, between wakefulness and after induction of anesthesia.
Sample size and statistical analyses.
The sample size was determined based on the standardized mean difference of 1.31 and standardized difference of 25 as previously described [32]. A sample size of 11 was needed to detect a > 30% change in VO2 with a significance level of 0.05 (two-tailed) and a power of 0.80, as previously reported [23]. Because indirect calorimetry measurement involves skill, the target number of patients was set at 22, assuming that measurement errors would occur in approximately 50% of cases.
The Friedman test for comparing measurement data at three sites and the Wilcoxon rank-sum test for comparing two groups were used for statistical analyses. Two-tailed tests were conducted, and p < 0.05 was considered significant.
All statistical analyses were conducted using GraphPad Prism version 5.00 (GraphPad Software, San Diego, CA, USA).
On the consent form, the participants were informed that they would receive remimazolam for general anesthesia. The anesthesiologist in charge of each case also performed the measurements and analyzed the results. One anesthesiologist performed the measurements with the assistance of one anesthesia assistant.
The figures were created using GraphPad Prism version 5.00 (GraphPad Software Inc., San Diego, CA, USA) and Microsoft PowerPoint (Microsoft Corporation, Redmond, WA, USA).
Results
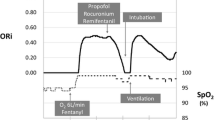
Twenty-two patients were enrolled from April 2021 to August 2021; of these, 11 patients were included (Fig. 1). The patients’ demographics were characterized by a median age of 67 years and no sex bias (Table 1). Heart rate, blood pressure, and hemoglobin decreased markedly from T1–T2 and T3 (Table 2).
In a cohort of 10 patients, we observed a statistically significant decrease over three time points in three key metrics: VO2/BSA, VCO2/BSA, and DO2/BSA. Specifically, the median VO2/BSA dropped from 130 (122–137) ml/min/m2 at T1 to 107 (81–133) ml/min/m2 at T2, and then further declined to 97 (93–121) ml/min/m2 at T3. This decline was statistically significant (p = 0.011). Similarly, the median VCO2/BSA decreased from 115 (105–129) ml/min/m2 at T1 to 90 (71–107) ml/min/m2 at T2, and decreased further to 81 (69–101) ml/min/m2 at T3. This trend was also statistically significant (p = 0.0020).
DO2/BSA followed a slightly different pattern. It decreased from a median of 467 (395–582) ml/min/m2 at T1 to 347 (286–392) ml/min/m2 at T2, but then increased slightly to 382 (238–414) ml/min/m2 at T3. This overall change was statistically significant (p = 0.0011). These results are visually represented in Fig. 2 and numerically detailed in Table 3.
Results of VO2, VCO2, DO2, and ERO2. Before and after induction of general anesthesia, VO2, VCO2, and DO2 dropped, but there was considerable variation among the patients. ERO2 did not change appreciably. *p < 0.05, T1 vs. T3. **p < 0.05, T1 vs. T2. VO2, oxygen consumption; VCO2, carbon dioxide production; DO2, oxygen delivery; ERO2, oxygen extraction rate; T1, first time point; T2, second time point; T3, third time point; BSA body surface area
The analysis revealed a characteristic trend in the change in oxygen metabolism between the two groups divided by the VCO2 at T2. There were no significant differences in the patients’ backgrounds, such as age and sex, between these two groups (Online Resource 1). There were also no significant differences at T1 for hemodynamics (e.g., heart rate, blood pressure, cardiac coefficient), respiratory status (minute ventilation rate, respiratory rate), oxygen supply–demand balance indices (VO2, VCO2, DO2), and acid–base equilibrium (pH, bicarbonate) (Online Resources 2 and 3). In contrast, no significant differences were found at T2 for the circulatory dynamics; however, differences were found for respiratory status (tidal volume and minute ventilation volume) and acid–base equilibrium (bicarbonate). Regarding the oxygen supply–demand balance index, VO2 showed similar highs and lows as those for VCO2, but DO2 showed no difference between the two groups.
Discussion
The key findings in this study were as follows:
-
1.
Remimazolam for induction of general anesthesia led to significant reductions in VO2 and VCO2, and an initial drop in DO2, indicating suppressed metabolic activity and oxygen demand.
-
2.
Patients stratified by VCO2 levels exhibited divergent patterns in respiratory parameters and acid–base status post-induction, despite comparable baseline characteristics.
-
3.
While changes in VO2 paralleled those for VCO2, DO2 remained similar between the groups, implying remimazolam’s metabolic effects may depend on the patient’s underlying metabolic state.
These findings provide important insights into the metabolic alterations and compensatory oxygen supply–demand dynamics during induction of general anesthesia with remimazolam. These findings highlight the need for individualized anesthetic management strategies that account for the patient’s specific metabolic profile and oxygen demands.
Most of the previously published reports we collected examined oxygen supply–demand balance using inhaled anesthetics. Jakobsson et al. [32] reported a 33 ml/min/m2 (95% confidence interval, 28–38 ml/min/m2) reduction in VO2 in a systematic review. Crozier et al. [33] reported a 102 ml/min (32.1%) reduction in VO2 after induction of general anesthesia with midazolam. In this study, as in a previous study [18], both oxygen supply and VO2 decreased. However, in contrast to the previous study, in which both oxygen supply and VO2 decreased simultaneously, the decrease in VO2 was smaller than previously reported in this study, with decreases in VO2, VCO2, and DO2 of 23 ml/min/m2 (17.7%), 25 ml/min/m2 (21.8%), and 120 ml/min/m2 (25.7%), respectively. Consequently, the ERO2 ranged from 26.1% during wakefulness to 36.8% during general anesthesia.
DO2 dependence on VO2 occurs when DO2(crit) is below the established range [9, 22, 34]. During anesthesia and cardiac resuscitation, DO2(crit) in healthy awake patients ranges from 270 to 330 ml/min/m2 [7, 35, 36]. The mechanism by which ERO2 is modified and corrected operates when DO2 is maintained above the critical value [7,8,9]. DO2(crit) thresholds are also elevated by mitochondrial dysfunction in patients with sepsis and hyperlactatemia [37, 38]. In this study, we observed some cases in which DO2/BSA fell below 330 ml/min/m2 at T2, but we encountered no cases with an increased R/Q. However, we observed cases with an R/Q of > 1 at T1. This suggests that the effect of sympathetic dominance during arousal on the tissue oxygen supply–demand balance is greater than the effect of parasympathetic dominance due to general anesthesia [39].
The most important difference between the present study and previous studies is in the use of general anesthesia. Because of concerns that inhalation anesthetics would compromise the accuracy of the indirect calorimetry data, only intravenous anesthetics were used in the present study. To exclude the impact of changes in hemodynamics and oxygen supply caused by vasoconstrictor treatment, we also excluded patients who received vasoconstrictor treatment. Inhaled anesthetics have ischemia preconditioning effects [40], and the changes in VO2 and VCO2 likely differ between inhaled and intravenous anesthetics, including remimazolam, in terms of the DO2 decrease.
At the cellular and tissue levels, biological reactions to variations in DO2 are distinct. Hypoxic cells respond with a self-imposed program to cut energy consumption by directly sensing a fall in oxygen levels long before the adenosine triphosphate (ATP) pool is depleted and by shutting down non-essential cellular processes [3]. Therefore, VO2 may have declined in a DO2-dependent manner. Because R/Q did not differ between the two groups, the low VO2 and VCO2 levels in the low VCO2 group were within the range of physiological alterations and above the DO2(crit) level.
When comparing differences in the variables between the two groups, no differences were found in the awake group (Online Resource 1). Under general anesthesia, differences were observed in VO2 as well as high and low VCO2 values, but there were no significant differences in the hemodynamic parameters, such as blood pressure, heart rate, cardiac output, stroke volume, peripheral vascular resistance, or DO2. The partial pressure of end-tidal CO2 values did not differ between the two groups because minute ventilation changed in parallel with changes in VCO2; however, differences were observed in acid–base equilibrium. Therefore, the effect on acid–base equilibrium was thought to have been caused by the change in cellular CO2 production.
The reason for dividing the patients into two groups (high and low VCO2) stems from a clinical question. The clinical question is whether changes in oxygen supply may cause fluctuations in VCO2 during induction of general anesthesia (as inferred from the minute ventilation rate and end-tidal CO2), which will require adjustments in respiratory management. Because VCO2 should correlate with VO2 in all but extreme oxygen metabolic situations, we thought that the relationship between oxygen supply and VO2 was relevant. We considered this an important topic because the maintenance of homeostasis, including oxygen metabolism, is the anesthesiologist’s responsibility during general anesthesia. Although the patients in this study were scheduled for surgery and were in a stable general condition, the discovery that only some patients tended to have decreased VCO2 values was considered a new finding.
The body composition variables influencing VO2, such as circulating blood volume, body temperature and its distribution, and lean body mass, may have varied among the patients. Changes in body temperature are related to alterations in tissue heat content (i.e., VO2 changes) [41]. The induction of general anesthesia may have decreased the deep body temperature and raised the peripheral heat content in the extremities [42], thereby altering the oxygen supply–demand balance.
In one patient in this study, DO2 and VO2 increased during the induction of general anesthesia. The data analysis revealed a drop in blood pressure and pulse rate from T1 to T2. However, cardiac output rose while peripheral vascular resistance fell. The ZHF temperature at T1 was as low as 35.1 °C, whereas the ZHF temperature was 36.5 °C, and the bladder temperature was 34.2 °C, at T2. The ZHF temperature did not vary by more than 1.4 °C in any other patients. The rapid redistribution of temperature brought on by general anesthesia may have contributed to the increases in DO2 and VO2 at T2.
The limitations of our study are that the characteristics of the patient groups and research methods affected the results. First, regarding the uncertainty of the measurement method, only a single measurement was taken each time. Given that each measurement took approximately 20 min to complete, the time required for many measurements would have been clinically inappropriate. Second, the third measurement was taken after the commencement of surgery. The results might have been influenced by factors, such as epidural anesthesia, bleeding, and surgical invasion. However, no patients developed massive bleeding that required transfusion and vasoconstrictor treatment. Despite our utmost efforts to eliminate as many factors as possible that could impact the balance of oxygen supply and demand, this remains an important limitation of our study and may have affected the consistency of the measurement results. Third, the indirect calorimetry measurements during the waking state may have contained errors due to the omission of respiration-related leakage from the device gap.
The findings of this study have important implications for intensivists and anesthesiologists who administer general anesthesia. It is often challenging to determine the appropriate amount of oxygen required for each patient in clinical practice, and the respiratory and cardiovascular systems are typically managed based on the established safe zone. Importantly, further developments in the methodology of this study may facilitate predictions of future changes in VO2 after the induction of general anesthesia.
In conclusion, general anesthetic induction with remimazolam decreased VO2, VCO2, and DO2. The data suggest that some cases behaved differently in response to changes in the oxygen supply–demand balance despite having the same settings for breathing conditions.
Data availability
The data used and/or generated in this study are available upon reasonable request. Data sharing will be done after ensuring there are no issues with protecting personal information or intellectual property rights. If you wish to access the data, please contact the corresponding author.
References
Hirota K. Hypoxia-inducible factor 1, a master transcription factor of cellular hypoxic gene expression. J Anesth. 2002;16(2):150–9.
Semenza GL. Regulation of mammalian O2 homeostasis by hypoxia-inducible factor 1 annual review of cell and developmental biology. Annu Rev Cell Dev Biol. 1999;15:551–78. https://doi.org/10.1146/annurev.cellbio.15.1.551.
Hochachka PW, Buck LT, Doll CJ, Land SC. Unifying theory of hypoxia tolerance: molecular/metabolic defense and rescue mechanisms for surviving oxygen lack. Proc Natl Acad Sci USA. 1996;93(18):9493–8.
Soong JTY, Soni N. Circulatory shock. Med UKi. 2013;41(2):64–9.
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Roman J, Alexandre M, Michael Pinksey R, Jean Louis T, Jean Louis V, Andrew R. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European society of intensive care medicine. Intensive Care Med. 2014;40(12):1795–815.
Dyson A, Ekbal N, Stotz M, Barnes S, Carré J, Tully S, Henderson S, Barret L, Singer M. Component reductions in oxygen delivery generate variable haemodynamic and stress hormone responses. Br J Anaesth. 2014;113(4):708–16.
Shibutani K, Komatsu T, Kubal K, Sanchala V, Kumar V, Bizzarri DV. Critical level of oxygen delivery in anesthetized man. Crit Care Med. 1983;11(8):640–3.
De Backer D. VO2/DO2 relationship: how to get rid of methodological pitfalls? Intensive Care Med. 2000;26(12):1719–22.
Vincent JL. DO 2/VO 2 relationships. Funct Hemodynamic Monit Updat Intensive Care Emerg Med. 2005;42:1–2.
Vincent JL, De Backer D. Oxygen transport - the oxygen delivery controversy. Intensive Care Med. 2004;30(11):1990–6.
De Backer D. Lactic acidosis. Intensive Care Med. 2003;29(5):699–702.
Dubin A, Pozo MO, Hurtado J. Central venous minus arterial carbon dioxide pressure to arterial minus central venous oxygen content ratio as an indicator of tissue oxygenation: a narrative review. Rev Bras Ter Intensiva. 2020;32(1):115–22.
Dubin A, Ferrara G, Kanoore Edul VS, Martins E, Canales HS, Canullán C, Murias G, Pozo MO, Estenssoro E. Venoarterial PCO2-to-arteriovenous oxygen content difference ratio is a poor surrogate for anaerobic metabolism in hemodilution: an experimental study. Ann Intensive Care. 2017. https://doi.org/10.1186/s13613-017-0288-z.
Kang AR, Lee J, Jung W, Lee M, Park SY, Woo J, Kim SH. Development of a prediction model for hypotension after induction of anesthesia using machine learning. PLoS ONE. 2020;15(4):1–17. https://doi.org/10.1371/journal.pone.0231172.
Terao Y, Miura K, Saito M, Sekino M, Fukusaki M, Sumikawa K. Quantitative analysis of the relationship between sedation and resting energy expenditure in postoperative patients. Crit Care Med. 2003;31(3):830–3.
Vernon DD. effect of neuromuscular blockade on oxygen consumption and energy expenditure in sedated, mechanically ventilated children. Pediatr Crit Care. 2000;28(5):10–27.
Bardutzky J, Georgiadis D, Kollmar R, Schwab S. Energy expenditure in ischemic stroke patients treated with moderate hypothermia. Intensive Care Med. 2004;30(1):151–4.
Jakobsson J, Vadman S, Hagel E, Kalman S, Bartha E. The effects of general anaesthesia on oxygen consumption: a meta-analysis guiding future studies on perioperative oxygen transport. Acta Anaesthesiol Scand. 2018;63(2):144–53.
Schüttler J, Eisenried A, Lerch M, Fechner J, Jeleazcov C, Ihmsen H. Pharmacokinetics and pharmacodynamics of remimazolam (CNS 7056) after continuous infusion in healthy male volunteers part I. Pharma Clin Pharma Anesthesiol. 2020;4:636–51.
Doi M, Morita K, Takeda J, Sakamoto A, Yamakage M, Suzuki T. Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth. 2020;34(4):543–53. https://doi.org/10.1007/s00540-020-02788-6.
Rex DK, Bhandari R, Desta T, DeMicco MP, Schaeffer C, Etzkorn K, Barish CF, Pruitt R, Cash BD, Quirk D, Tiongco F, Sullivan S, Bernstein D. A phase III study evaluating the efficacy and safety of remimazolam (CNS 7056) compared with placebo and midazolam in patients undergoing colonoscopy. Gastrointest Endosc. 2018;88(3):427-437.e6. https://doi.org/10.1016/j.gie.2018.04.2351.
Suga H, Hisano R, Goto Y, Yamada O, Igarashi Y. Effect of positive inotropic agents on the relation between oxygen consumption and systolic pressure volume area in canine left ventricle. Circ Res. 1983;53(3):306–18.
Jakobsson J, Norén C, Hagel E, Kalman S, Bartha E. Peri-operative oxygen consumption revisited: an observational study in elderly patients undergoing major abdominal surgery. Eur J Anaesthesiol. 2021;38(1):4–12.
Crystal GJ, Silver JM, Salem MR. Mechanisms of increased right and left ventricular oxygen uptake during inotropic stimulation. Life Sci. 2013;93(2–3):59–63. https://doi.org/10.1016/j.lfs.2013.05.011.
Hahm TS, Jeong H, Ahn HJ. Systemic oxygen delivery during one-lung ventilation: comparison between propofol and sevoflurane anaesthesia in a randomised controlled trial. J Clin Med. 2019;8(9):1438.
Acute Respiratory Distress Syndrome Network Roy G Brower Michael A Matthay Alan Morris David Schoenfeld B Taylor Thompson Arthur WheelerAcute Respiratory Distress Syndrome Network Roy G Brower Michael A Matthay Alan Morris David Schoenfeld B Ta AW. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000. https://doi.org/10.1056/NEJM200005043421801.
Frayn KN. Calculation of substrate oxidation rates in vivo from gaseous exchange. J Appl Physiol. 2016;121(6):628–34.
Jorgensen CR, Wang K, Wang Y, Gobel FL, Nelson RR, Taylor H, Frank Gams R, JohnVilandre E. Effect of propranolol on myocardial oxygen consumption and its hemodynamic correlates during upright exercise. Circulation. 1973;48(6):1173–82.
LaFarge CG, Miettinen OS. The estimation of oxygen consumption. Cardiovasc Res. 1970;4(1):23–30. https://doi.org/10.1093/cvr/4.1.23.
Badal JJ, Loeb RG, Trujillo DK. A simple method to determine mixed exhaled CO2 using a standard circle breathing circuit. Anesth Analg. 2007;105(4):1048–52.
Kligfield P. Heart disease: a textbook of Cardiovascular Medicine, 5/E, edited by Eugene Braunwald, W.B. Saunders, Philadelphia (1997) 2143 pages, illustrated, $125.00 ISBN: 9‐7216‐5666‐8. Clin Cardiol. 1998;21(2):147–8. https://doi.org/10.1002/clc.4960210223.
Jakobsson J, Vadman S, Hagel E, Kalman S, Bartha E. The effects of general anaesthesia on oxygen consumption: a meta-analysis guiding future studies on perioperative oxygen transport. Acta Anaesthesiol Scand. 2019;63(2):144–53.
Crozier TA, Langenbeck M, Müller J, Kietzmann D, Sydow M, Kettler D. Total intravenous anaesthesia with sufentanil-midazolam for major abdominal surgery. Eur J Anaesthesiol. 1994;11(6):449–59.
Weg JG. Oxygen transport in adult respiratory distress syndrome and other acute circulatory problems: relationship of oxygen delivery and oxygen consumption. Crit Care Med. 1991;19(5):650–7.
Lieberman JA, Weiskopf RB, Kelley SD, Feiner J, Noorani M, Leung J, Pearl T, Maurene V. Critical oxygen delivery in conscious humans is less than 7.3 ml O2 kg−1 min−1. Anesthesiology. 2000;92(2):407–13.
Smoor RM, van Dongen EPA, Verwijmeren L, Schreurs IAAM, Vernooij LM, van Klei WA, Noordzij PG. Critical oxygen delivery threshold during cardiopulmonary bypass in older cardiac surgery patients with increased frailty risk. Eur J Cardio Thorac Surg. 2021;00:1–8.
Protti A, Fortunato F, Monti M, Vecchio S, Gatti S, Comi GP, Giuseppe RD, Gattinoni L. Metformin overdose, but not lactic acidosis per se, inhibits oxygen consumption in pigs. Crit Care. 2012;16(3):R75.
Brody JS. Oxygen uptake supply dependency. Effects of short-term dobutamine infusion. Am Rev Respir Dis. 1990;4(3):1–5.
Yilmaz B, Göktepe S, Yaşar E, Kesikburun S, Adigüzel E. The effect of autonomic nervous system dysfunction on oxygen consumption during daily living activities in patients with spinal cord injury. Spinal Cord. 2017;55(3):300–3.
Chen S, Lotz C, Roewer N, Broscheit JA. Comparison of volatile anesthetic-induced preconditioning in cardiac and cerebral system: molecular mechanisms and clinical aspects. Eur J Med Res. 2018;23(1):1–10. https://doi.org/10.1186/s40001-018-0308-y.
Baraka A. Influence of surface cooling and rewarming on whole-body oxygen supply-demand balance. Br J Anaesth. 1994;73(3):418–20.
Matsukawa T, Sessler DI, Sessler AM, Schroeder M, Ozaki M, Kurz A, Christi C. Heat flow and distribution during induction of general anesthesia. Anesthesiology. 1995;82(3):662–73.
Acknowledgements
We thank Keisuke Nakamura, Master of Medicine (Department of Medical Engineering, Yamagata University Hospital, Yamagata, Japan) for support during the measurements with the indirect calorimeter
Funding
Financial support was provided solely by departmental sources.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection and analysis were performed by Kenya Yarimizu. The first draft of the manuscript was written by Kenya Yarimizu. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Yarimizu, K., Onodera, Y., Suzuki, H. et al. Changes in oxygen supply–demand balance during induction of general anesthesia: an exploratory study using remimazolam. J Anesth (2024). https://doi.org/10.1007/s00540-024-03362-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00540-024-03362-0