Abstract
Purpose
Spinal anesthesia is a standard technique for cesarean delivery; however, it possesses a risk of hypotension. We hypothesised that the changes in the corrected flow time induced by the Trendelenburg position could predict the incidence of hypotension after spinal anesthesia for cesarean delivery.
Methods
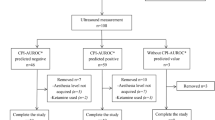
Patients undergoing elective cesarean delivery under spinal anesthesia were enrolled. Before anesthesia induction, corrected flow time was measured in the supine and Trendelenburg positions (FTc-1 and FTc-2, respectively). Additionally, a percent change in corrected flow time induced by the Trendelenburg position was defined as ΔFTc. The primary endpoint was to investigate the ability of ΔFTc to predict the incidence of spinal anesthesia-induced hypotension until delivery. The receiver operating characteristics curves to assess the ability of FTc-1, FTc-2, and ΔFTc to predict the incidence of hypotension were generated.
Results
Finally, 40 patients were included, and of those, 26 (65%) developed spinal anesthesia-induced hypotension. The areas under the curve for FTc-1, FTc-2, and ΔFTc were 0.591 (95% CI: 0.424 to 0.743) (P = 0.380), 0.742 (95% CI: 0.579 to 0.867) (P = 0.004), and 0.882 (95% CI: 0.740 to 0.962) (P < 0.001) respectively, indicating ΔFTc as the best predictor among these three parameters. The best threshold for ΔFTc was 6.4% (sensitivity: 80.8% (95% CI: 53.8 to 96.2), specificity: 85.7% (95% CI: 42.9 to 100.0)).
Conclusions
This study demonstrated that changes in the corrected carotid flow time induced by the Trendelenburg position could serve as a good predictor of spinal anesthesia-induced hypotension for cesarean delivery.




Similar content being viewed by others
Data availability
Data will be available upon reasonable request to corresponding author.
References
Sakata K, Yoshimura N, Tanabe K, Kito K, Nagase K, Iida H. Prediction of hypotension during spinal anesthesia for elective cesarean section by altered heart rate variability induced by postural change. Int J Obstet Anesth. 2017;29:34–8.
Lee JE, George RB, Habib AS. Spinal-induced hypotension: incidence, mechanisms, prophylaxis, and management: summarizing 20 years of research. Best Pract Res Clin Anaesthesiol. 2017;31:57–68.
Frassanito L, Sonnino C, Piersanti A, Zanfini BA, Catarci S, Giuri PP, Scorzoni M, Gonnella GL, Antonelli M, Draisci G. Performance of the hypotension prediction index with noninvasive arterial pressure waveforms in awake cesarean delivery patients under spinal anesthesia. Anesth Analg. 2022;134:633–43.
Kim HJ, Choi YS, Kim SH, Lee W, Kwon JY, Kim DH. Predictability of preoperative carotid artery-corrected flow time for hypotension after spinal anaesthesia in patients undergoing caesarean section: a prospective observational study. Eur J Anaesthesiol. 2021;38:394–401.
Kuwata S, Suehiro K, Juri T, Tsujimoto S, Mukai A, Tanaka K, Yamada T, Mori T, Nishikawa K. Pleth variability index can predict spinal anaesthesia-induced hypotension in patients undergoing caesarean delivery. Acta Anaesthesiol Scand. 2018;62:75–84.
Chooi C, Cox JJ, Lumb RS, Middleton P, Chemali M, Emmett RS, Simmons SW, Cyna AM. Techniques for preventing hypotension during spinal anaesthesia for caesarean section. Cochrane Database Syst Rev. 2020. https://doi.org/10.1002/14651858.CD002251.pub4.
Mukai A, Suehiro K, Kimura A, Kodama S, Tanaka K, Mori T, Nishikawa K. Impact of deep breathing on predictability of stroke volume variation in spontaneous breathing patients. Acta anaesthesiol Scand. 2020;64:648–55.
Suehiro K. Update on the assessment of fluid responsiveness. J Anesth. 2020;34:163–6.
Kimura A, Suehiro K, Juri T, Fujimoto Y, Yoshida H, Tanaka K, Mori T, Nishikawa K. Hemodynamic changes via the lung recruitment maneuver can predict fluid responsiveness in stroke volume and arterial pressure during one-lung ventilation. Anesth Analg. 2021;133:44–52.
Kimura A, Suehiro K, Juri T, Tanaka K, Mori T. Changes in corrected carotid flow time induced by recruitment maneuver predict fluid responsiveness in patients undergoing general anesthesia. J Clin Monit Comput. 2021. https://doi.org/10.1007/s10877-021-00736-7.
Watanabe R, Suehiro K, Mukai A, Tanaka K, Yamada T, Mori T, Nishikawa K. Changes in stroke volume induced by lung recruitment maneuver can predict fluid responsiveness during intraoperative lung-protective ventilation in prone position. BMC Anesthesiol. 2021;21:303.
Toyama S, Kakumoto M, Morioka M, Matsuoka K, Omatsu H, Tagaito Y, Numai T, Shimoyama M. Perfusion index derived from a pulse oximeter can predict the incidence of hypotension during spinal anaesthesia for Caesarean delivery. Br J Anaesth. 2013;111:235–41.
Sun S, Huang SQ. Role of pleth variability index for predicting hypotension after spinal anesthesia for cesarean section. Int J Obstet Anesth. 2014;23:324–9.
Yokose M, Mihara T, Sugawara Y, Goto T. The predictive ability of non-invasive haemodynamic parameters for hypotension during caesarean section: a prospective observational study. Anaesthesia. 2015;70:555–62.
Barjaktarevic I, Toppen WE, Hu S, Aquije Montoya E, Ong S, Buhr R, David IJ, Wang T, Rezayat T, Chang SY, Elashoff D, Markovic D, Berlin D, Cannesson M. Ultrasound assessment of the change in carotid corrected flow time in fluid responsiveness in undifferentiated shock. Crit Care Med. 2018;46:e1040–6.
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, Teboul JL. Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med. 2006;34:1402–7.
Luo JC, Su Y, Dong LL, Hou JY, Li X, Zhang Y, Ma GG, Zheng JL, Hao GW, Wang H, Zhang YJ, Luo Z, Tu GW. Trendelenburg maneuver predicts fluid responsiveness in patients on veno-arterial extracorporeal membrane oxygenation. Ann Intensive Care. 2021;11:16.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45.
Mascha EJ. Identifying the best cut-point for a biomarker, or not. Anesth Analg. 2018;127:820–2.
Cannesson M, Le Manach Y, Hofer CK, Goarin JP, Lehot JJ, Vallet B, Tavernier B. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a “gray zone” approach. Anesthesiology. 2011;115:231–41.
Popović ZB, Thomas JD. Assessing observer variability: a user’s guide. Cardiovasc Diagn Ther. 2017;7:317–24.
Bishop DG, Cairns C, Grobbelaar M, Rodseth RN. Heart rate variability as a predictor of hypotension following spinal for elective caesarean section: a prospective observational study. Anaesthesia. 2017;72:603–8.
Muller L, Bobbia X, Toumi M, Louart G, Molinari N, Ragonnet B, Quintard H, Leone M, Zoric L, Lefrant JY. Respiratory variations of inferior vena cava diameter to predict fluid responsiveness in spontaneously breathing patients with acute circulatory failure: need for a cautious use. Crit Care. 2012;16:R188.
Hossein-Nejad H, Banaie M, Davarani SS, Mohammadinejad P. Assessment of corrected flow time in carotid artery via point-of-care ultrasonography: reference values and the influential factors. J Crit Care. 2017;40:46–51.
Blehar DJ, Glazier S, Gaspari RJ. Correlation of corrected flow time in the carotid artery with changes in intravascular volume status. J Crit Care. 2014;29:486–8.
Kim DH, Shin S, Kim N, Choi T, Choi SH, Choi YS. Carotid ultrasound measurements for assessing fluid responsiveness in spontaneously breathing patients: corrected flow time and respirophasic variation in blood flow peak velocity. Br J Anaesth. 2018;121:541–9.
Xu L, Dai S, Shen J, Lv C, Tang Y, Chen X. The predictive ability of carotid artery corrected flow time and respirophasic variation in blood flow peak velocity measured by ultrasonography for fluid responsiveness in parturients for cesarean delivery. Minerva Anestesiol. 2020;86:1039–46.
Suehiro K. Assessing fluid responsiveness during spontaneous breathing. J Anesth. 2022;36:579–82.
Juri T, Suehiro K, Kimura A, Mukai A, Tanaka K, Yamada T, Mori T, Nishikawa K. Impact of non-invasive continuous blood pressure monitoring on maternal hypotension during cesarean delivery: a randomized-controlled study. J Anesth. 2018;32:822–30.
Acknowledgements
We would like to thank Honyaku Center Inc. for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Koichi Suehiro has received speaker fees from Edwards Lifesciences and Otsuka Pharmaceutical Factory. Other authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
540_2023_3293_MOESM1_ESM.pptx
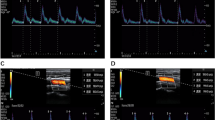
Supplementary file1 Fig. 1. FTc-1: Corrected flow time in the supine position. FTc-2: Corrected flow time in the Trendelenburg position. Flow of the study. The flow time was measured in the supine and subsequently in the Trendelenburg position (15 degrees). (PPTX 47 KB)
540_2023_3293_MOESM3_ESM.pptx
Supplementary file3 Fig. 3. ΔFTc: Percent changes in the corrected flow time induced by the Trendelenburg position. a Correlation between ΔFTc and the duration of hypotension until delivery. b Correlation between ΔFTc and the number of doses of vasoactive drugs until delivery. (PPTX 66 KB)
About this article
Cite this article
Juri, T., Suehiro, K., Yasuda, S. et al. Changes in the corrected carotid flow time can predict spinal anesthesia-induced hypotension in patients undergoing cesarean delivery: an observational study. J Anesth 38, 105–113 (2024). https://doi.org/10.1007/s00540-023-03293-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-023-03293-2