Abstract
Purpose
Failed needle-tip positioning in an ultrasound-guided infraclavicular block can be due to improper needle insertion point and steep needle insertion angle. Needle pre-curving enables the user to pass the needle with different curved trajectories on approaching the brachial plexus. Aim of the study was to compare curved and non-curved needles as regards the time needed to perform the lateral sagittal infra-clavicular block.
Methods
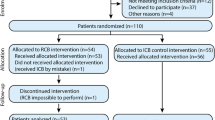
Sixty-nine patients undergoing surgery distal to the elbow were randomly allocated to two groups: group A (n = 35), which received ultrasound-guided infraclavicular block using the curved needle; and group B (n = 34), which received the infraclavicular block using the non-curved needle. The primary outcome measure was the time needed to perform the infraclavicular block. Anesthetist’s experience with the curved vs. non-curved needle was noted.
Results
Mean (SD) recognition time (120 ± 48 vs. 179 ± 72 s, P = 0.0002) and injection time (54 ± 23 vs. 88 ± 36 s, P = 0.0001) were shorter in group A compared to group B. Median (IQR) procedure pain score was less in group A 2 (1–2) than in group B 2 (2–3); P = 0.001. Median (IQR) satisfaction score was higher with regards to the curved needle 4 (4–5) than non-curved needle 3 (3–4) in performing infraclavicular blockade; P = 0.001.
Conclusion
The use of a curved needle reduces the time required to perform the lateral sagittal infraclavicular block. The curved needle provides less procedure pain and higher satisfaction levels among anesthetists than the non-curved needle.
Trial registration
The trial was registered (04/26/2016) with the ClinicalTrials.gov ID: NCT02799576. Approval Number: #2543. Board Name: Research Ethics Committee. Board Affiliation: Suez Canal University, Faculty of Medicine, Suez Canal University hospital, Ismailia, Egypt, 41522.



Similar content being viewed by others
References
Gürkan Y, Hosten T, Solak M, Toker K. Lateral sagittal infraclavicular block. Clinical experience in 380 patients. Acta Anaesthesiol Scand. 2008;52:262–6.
Greher M, Retzl G, Niel P, Kamholz L, Marhofer P, Kapral S. Ultrasonographic assessment of topographic anatomy in volunteers suggests a modification of the infraclavicular brachial block. Br J Anaesth. 2002;88:632–6.
Sauter AR, Dodgson MS, Stubhaug A, Halstensen AM, Klaastad O. Electrical nerve stimulation or ultrasound guidance for lateral sagittal infraclavicular blocks. A randomized, controlled, observer-blinded, comparative study. Anesth Analg. 2008;106:1910–5.
Neal JM, Brull R, Chan VW, Grant SA, Horn JL, Liu SS, McCartney CJ, Narouze SN, Perlas A, Salinas FV, Sites BD, Tsui BC. The ASRA evidence-based medicine assessment of ultrasound-guided regional anesthesia and pain medicine: executive summary. Reg Anesth Pain Med. 2010;35:S1–9.
Bigeleisen P, Wilson M. A comparison of two techniques for ultrasound-guided infraclavicular block. Br J Anaesth. 2006;96:502–7.
Sinha C, Kumar A, Singh AK, Bhadani UK. Retroclavicular approach of brachial plexus block: Here to stay. Saudi J Anaesth. 2017;11(4):519–20.
Klaastad O, Smith H, Smedby O, Winther-Larssen EH, Brodal P, BreiviK H, Fosse ET. A novel infraclavicular brachial plexus block: the lateral and sagittal technique, developed by magnetic resonance imaging studies. Anesth Analg. 2004;98:252–6.
Bowens C Jr, Gupta RK, O'Byrne WT, Schildcrout JS, Shi Y, Hawkins JJ, Michaels DR, Berry JM. Selective local anesthetic placement using ultrasound guidance and neurostimulation for infraclavicular brachial plexus block. Anesth Analg. 2010;110(5):1480–5.
Porter JM, McCartney CJ, Chan VW. Needle placement and injection posterior to the axillary artery may predict successful infraclavicular brachial plexus block: a report of three cases. Can J Anaesth. 2005;52:69–73.
Bloc S, Garnier T, Komly B, Asfazadourian H, Leclerc P, Mercadal L, Morel B, Dhonneur G. Spread of injectate associated with radial or median nerve type motor response during infraclavicular brachial plexus block: an ultrasound evaluation. Reg Anesth Pain Med. 2007;32:130–5.
Hadzic A. Hadzic’s peripehral nerve blocks and anatomy for ultrasound-guided regional anesthesia. 2nd ed. New York: McGrawHill; 2012.
Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932;22(140):55.
Marhofer P, Greher M, Kapral S. Ultrasound guidance in regional anesthesia. Br J Anaesth. 2005;94:7–17.
Dingemans E, Williams SR, Arcand G, Chouinard P, Harris P, Ruel M, Girard F. Neurostimulation in ultrasound-guided infraclavicular block: a prospective randomized trial. Anesth Analg. 2007;104:1275–80.
Nebab EG, Florence IM. An alternative needle geometry for alternative needle geometry for interruption of the ganglion impar. Anesthesiology. 1997;86:1213–4.
Song HS, Kim DY, Yoon KS. Intervention using ultrasonography. J Korean Orthop Assoc. 2013;48:342–9.
Maecken T, Zenz M, Grau T. Ultrasound characteristics of needles for regional anesthesia. Reg Anesth Pain Med. 2007;32:440–7.
Tammam TF, Kamhawy GA. Ultrasound-guided regional blockade for lipoma excision: a new approach to an old technique. Acta Anaesthesiol Scand. 2017;61(10):1325–33.
Acknowledgements
The authors thank Youssef Tammam who helped us in preparation the template to process the needle in a standardized way and get the exact same needle contour curvature.
Funding
The authors have no sources of funding to declare for this manuscript.
Author information
Authors and Affiliations
Contributions
TFT: Role: This author described and recommended the curved needle for technically easier infraclavicular block performance. The author was involved in the design of the study; analysis, interpretation of data and preparation of the manuscript. GAK: Role: This author was involved in the design of the study; analysis of data and preparation of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Tammam, T.F., Kamhawy, G.A. Use of a curved needle to facilitate lateral sagittal infraclavicular block performance: a randomized clinical trial. J Anesth 33, 604–611 (2019). https://doi.org/10.1007/s00540-019-02674-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-019-02674-w