Abstract
Purpose
Generally, novices are taught fiberoptic intubation on patients by attending anesthesiologists; however, this approach raises patient safety concerns. Patient safety should improve if novice learners are trained for basic skills on simulators. In this educational study, we assessed the time and number of attempts required to train novices in fiberoptic bronchoscopy and fiberoptic intubation on simulators. Because decay in skills is inevitable, we also assessed fiberoptic bronchoscopy and fiberoptic intubation skill decay and the amount of effort required to regain fiberoptic bronchoscopy skill.
Methods
First, we established attempt- and duration-based quantitative norms for reaching skill proficiency for fiberoptic bronchoscopy and fiberoptic intubation by experienced anesthesiologists (n = 8) and prepared an 11-step checklist and a 5-point global rating scale for assessment. Novice learners (n = 15) were trained to reach the established skill proficiency in a Virtual Reality simulator for fiberoptic bronchoscopy skills and a Human Airway Anatomy Simulator for fiberoptic intubation skills. Two months later, novices were reassessed to determine decay in learned skills and the required time to retrain them to fiberoptic bronchoscopy proficiency level.
Results
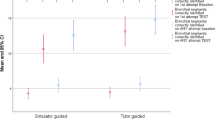
Proficiency in fiberoptic bronchoscopy skill level was achieved with 11 ± 5 attempts and after 658 ± 351 s. After 2 months without practice, the time taken by the novices to successful fiberoptic bronchoscopy on the Virtual Reality simulator increased from 41 ± 8 to 68 ± 31 s (P = 0.0138). Time and attempts required to retrain them were 424 ± 230 s and 9.1 ± 4.6 attempts, respectively.
Conclusion
Novices were successfully trained to proficiency skill level. Although fiberoptic bronchoscopy skills started to decay within 2 months, the re-training time was shorter.
Similar content being viewed by others
References
Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of the difficult airway: a closed claims analysis. Anesthesiology. 2005;103(1):33–9.
Tomlinson A. Effects of the EWTD on anaesthetic training in the UK. Anaesthesia. 2005;60(1):96–7.
Paolini JB, Donati F, Drolet P. Review article: video-laryngoscopy: another tool for difficult intubation or a new paradigm in airway management? Can J Anaesth. 2013;60(2):184–91.
Smith M, Calder I, Crockard A, Isert P, Nicol ME. Oxygen saturation and cardiovascular changes during fibreoptic intubation under general anaesthesia. Anaesthesia. 1992;47(2):158–61.
Goldmann K, Steinfeldt T. Acquisition of basic fiberoptic intubation skills with a virtual reality airway simulator. J Clin Anesth. 2006;18(3):173–8.
Naik VN, Matsumoto ED, Houston PL, Hamstra SJ, Yeung RY, Mallon JS, Martire TM. Fiberoptic orotracheal intubation on anesthetized patients: do manipulation skills learned on a simple model transfer into the operating room? Anesthesiology. 2001;95(2):343–8.
Arthur W Jr, Bennett W Jr, Stanush P, McNelly T. Factors that influence skill decay and retention: a quantitative review and analysis. Hum Perf. 1998;11(1):57–101.
Anderson GS, Gaetz M, Masse J. First aid skill retention of first responders within the workplace. Scand J Trauma Resusc Emerg Med. 2011;19:11.
Ahya SN, Barsuk JH, Cohen ER, Tuazon J, McGaghie WC, Wayne DB. Clinical performance and skill retention after simulation-based education for nephrology fellows. Semin Dial. 2012;25(4):470–3.
Policies and Procedures for Certification: American Board of Internal Medicine (ABIM). http://www.abim.org/certification/policies/imss/im.aspx#procedures. Accessed March 2015.
Duan X, Wu D, Bautista AF, Akca O, Carter MB, Latif RK. Assessment of reaching proficiency in procedural skills: fiberoptic airway simulator training in novices. Open Access Med Stat. 2011;1:45–50
Rowe R, Cohen RA. An evaluation of a virtual reality airway simulator. Anesth Analg. 2002;95(1):62–6.
Anderson GS, Gaetz M, Statz C, Kin B. CPR skill retention of first aid attendants within the workplace. Prehosp Disaster Med. 2012;27(4):312–8.
Martin KM, Larsen PD, Segal R, Marsland CP. Effective nonanatomical endoscopy training produces clinical airway endoscopy proficiency. Anesth Analg. 2004;99(3):938–44.
Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med. 2009;169(15):1420–3.
Barsuk JH, McGaghie WC, Cohen ER, O’Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med. 2009;37(10):2697–701.
Marsland CP, Robinson BJ, Chitty CH, Guy BJ. Acquisition and maintenance of endoscopic skills: developing an endoscopic dexterity training system for anesthesiologists. J Clin Anesth. 2002;14(8):615–9.
Hodges B, Regehr G, McNaughton N, Tiberius R, Hanson M. OSCE checklists do not capture increasing levels of expertise. Acad Med. 1999;74(10):1129–34.
Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35(6):382–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Appendices
Appendix A
Simulators. We utilized two different types of simulators in this research:
-
1.
The computerized AccuTouch® Bronchoscopy Simulator (Immersion Medical, Gaithersburg, MD, USA) is a Virtual Reality partial-task trainer consisting of a proxy flexible bronchoscope, a robotic interface device, a computer, a monitor, and simulation software. The monitor of the Virtual Reality computer generates anatomical 3-D images. This simulator can be used to learn fiberoptic bronchoscopy but not fiberoptic intubation because the actual placement of the endotracheal tube into the trachea cannot be simulated. The bronchoscope part of the simulator can be steered and maneuvered through the Virtual Reality simulator nose into the trachea. During fiberoptic bronchoscopy, the Virtual Reality computer records a variety of data, such as the total duration of the procedure and time spent in ‘red out’ (viewing only mucosa at contact range). At the end of the simulated procedure, these data can be saved and printed for analysis of performance and for teaching purposes.
-
2.
The Human Anatomy Airway Simulator (HAAS—Medical Plastic Laboratory, Gatesville, TX, USA) consists of a manikin-like face, head, neck, and upper chest. Inside the mouth is a simulated pharynx and larynx that lead to a simulated trachea and bronchi. The HAAS is not electronic or computerized in any way. When used for training purposes, the learner’s performance must be assessed by a trained observer.
Appendix B: Checklist for fiberoptic intubation performance
Done correctly | Done incorrectly | ||
|---|---|---|---|
1 | Hold control section correctly in one hand with thumb position for flexion and extension control, and index finger for suction | ||
2 | Focus scope using appropriate external object | ||
3 | Control tip of scope with other hand | ||
4 | Hold the fiberoptic scope firmly and straight | ||
5 | Introduce bronchoscope into mouth/nose centered | ||
6 | Maneuvers bronchoscope through nasopharynx/oropharynx and visualizes cords | ||
7 | Passes cords | ||
8 | Continues insertion of bronchoscope until visualization of carina | ||
9 | Passes endotracheal tube | ||
10 | Reconfirm vision of carina after ETT in situ | ||
11 | Removes bronchoscope smoothly |
Appendix C: Five-point global rating scale (GRS) of fiberoptic intubation performance
Please circle the number corresponding to the candidate’s performance in each category | ||||
|---|---|---|---|---|
1 | 2 | 3 | 4 | 5 |
Very poor | Competent | Clearly superior | ||
Repeatedly makes tentative or awkward moves with bronchoscope by inappropriate use of scope | Competent use of instruments but occasionally appears stiff and awkward | Fluid manipulation of bronchoscope and no awkwardness | ||
Hesitant or jerky attempts to progress | General progression, occasional hesitancy | Progresses smoothly between sequential landmarks | ||
Image not oriented | Image usually oriented | Maintains orientation | ||
Loses view and hits mucosa frequently | Occasionally loses view and collides with mucosa | Maintains view in center of air space | ||
Hit-and-miss approach to navigation | Generally purposeful; some inaccuracy with initial movement | Initial movement is desired movement, i.e., purposeful and accurate | ||
Misses targets outside field of view | Achieves most targets | Achieves targets | ||
Appendix D: Development of video assessment tools and training of raters
Video assessment tools
Once the study data collection was complete, recorded videos were reviewed to confirm their blinded codes without any identifiers.
-
1.
HAAS assessment tool development:
-
(a)
Checklist. Prior to recruitment of study subjects, we assigned two attending anesthesiologists from our fiberoptic intubation training team to serve as a panel to select and develop research instruments to rate each participant’s fiberoptic intubation performance on the HAAS. They adopted a previously used 10-item binary scoring checklist [6] (with permission), added one essential item (#4: holds the fiberoptic scope firmly and straight) to create an 11-item scoring fiberoptic intubation scoring checklist (Appendix B). For each item, a score of ‘1’ meant ‘done correctly’ and ‘0’ meant ‘done incorrectly’. Thus the maximum score was 11 if every item was performed correctly.
-
(b)
Global rating scale (GRS). To give raters more flexibility, the panel added a previously used 6-item Global Rating Scale (GRS) to assess subject hand movements and image maintenance on a 5-point Likert scale (with permission) [6] with a maximum score of 30 points (Appendix C). The panel of experts reviewed and agreed on each item to ensure construct and face validity in a method modified by Lynn [19].
-
(c)
Definition of successful fiberoptic intubation. To achieve a successful fiberoptic intubation the participant must move the tip of the bronchoscope from the nostril or lips to the carina, advance the endotracheal tube over the bronchoscope into the trachea, and the position of the tube is confirmed by relative positioning to the carina. The total time required to complete a successful fiberoptic intubation was measured from the recorded video clips.
Training the raters
We recruited two more anesthesia faculty members to serve as blinded raters and trained them in the use of the Video Assessment Tools by showing them the fiberoptic intubation instructional video (author originated) developed for teaching novices. During this session, they were trained in what constitute ‘done correctly’ and ‘done incorrectly’ elements of the checklist scoring instrument and quality of fiberoptic intubation process using the five-point GRS (Likert scale, anchored 1 to 5 with 5 being ‘clearly superior’). In order to minimize bias, we selected raters who were experienced anesthesiology faculty members but not involved in the creation of the rating instrument or in the recruitment or training of subjects. All items on the fiberoptic intubation scoring checklist and GRS were explained to the raters and their questions answered. All the video clips were rated independently by the two blinded raters using Video Assessment Tools.
About this article
Cite this article
K Latif, R., Bautista, A., Duan, X. et al. Teaching basic fiberoptic intubation skills in a simulator: initial learning and skills decay . J Anesth 30, 12–19 (2016). https://doi.org/10.1007/s00540-015-2091-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-015-2091-z