Abstract
Purpose
Appropriate adjustment of cardiac preload is essential to maintain cardiac output (CO), especially in patients after cardiac surgery. This study was intended to determine whether index of right ventricular end-diastolic volume (RVEDVI), corrected RVEDVI using ejection fraction (cRVEDVI), index of initial distribution volume of glucose (IDVGI), or cardiac filling pressures are correlated with cardiac index (CI) following cardiac surgery in the presence or absence of arrhythmias.
Methods
Eighty-six consecutive cardiac surgical patients were studied. Patients were divided into two groups: the non-arrhythmia (NA) group (n = 72) and the arrhythmia (A) group (n = 14). Three sets of measurements were performed: on admission to the ICU and daily on the first 2 postoperative days. The relationship between each cardiac preload variable and cardiac index (CI) was evaluated. A p value less than 0.05 indicated statistically significant differences.
Results
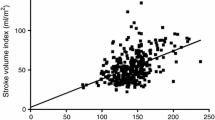
Each studied variable was not different between the two groups immediately after admission to the ICU. cRVEDVI had a linear correlation with CI in both group (NA group: r = 0.67, n = 216, p < 0.001; A group: r = 0.77, n = 42, p < 0.001), but RVEDVI had a poor correlation with CI (NA group: r = 0.27, n = 216, p < 0.001; A group: r = 0.19, n = 42, p = 0.036). IDVGI had a linear correlation with CI (NA group: r = 0.49, n = 216, p < 0.001; A group: r = 0.61, n = 42, p < 0.001), Cardiac filling pressures had no correlation with CI.
Conclusion
Our results demonstrated that cRVEDVI and IDVGI were correlated with CI in the presence or absence of arrhythmias. cRVEDVI and IDVGI have potential as indirect cardiac preload markers following cardiac surgery.


Similar content being viewed by others
References
De Hert SG, Rodrigus IE, Haenen LR, De Mulder PA, Gillebert TC. Recovery of systolic and diastolic left ventricular function early after cardiopulmonary bypass. Anesthesiology. 1996;85:1063–75.
Mangano D. Biventricular function after myocardial revascularization in humans: deterioration and recovery patterns during the first 24 hours. Anesthesiology. 1985;62:571–7.
Breisblatt WM, Stein KL, Wolfe CJ, Follansbee WP, Capozzi J, Armitage JM, Hardesty RL. Acute myocardial dysfunction and recovery: a common occurrence after coronary bypass surgery. J Am Coll Cardiol. 1990;15:1261–9.
Kumar A, Anel R, Bunnnell E, Habet K, Zanotti S, Marshall S, Neumann A, Ali A, Cheang M, Kavinsky C, Parrillo JE. Pulmonary artery occlusion pressure and central venous pressure fail to predict ventricular filling volume, cardiac performance, or the response to volume infusion in normal subjects. Crit Care Med. 2004;32:691–9.
Diebel LN, Wilson RF, Tagett MG, Kline RA. End-diastolic volume: a better indicator of preload in the critically ill. Arch Surg. 1992;127:817–22.
Wiesenack C, Fiegl C, Andreas K, Laule S, Prasser C, Keyl C. Continuously assessed right ventricular end-diastolic volume as a marker of cardiac preload and fluid responsiveness in mechanically ventilated cardiac surgical patients. Crit Care. 2005;9:R226–33.
Godje O, Peyerl M, Lamm P, Mair H, Reichart B. Central venous pressure, pulmonary capillary wedge pressure and intrathoracic blood volumes as preload indicators in cardiac surgery patients. Eur J Cardiothorac Surg. 1998;13:533–40.
Malbrain ML, De Potter TJ, Dits H, Reuter DA. Global and right ventricular end-diastolic volumes correlate better with preload after correction for ejection fraction. Acta Anaesthesiol Scand. 2010;54:622–31.
Iwakawa T, Ishihara H, Takamura K, Sakai I, Suzuki A. Measurements of extracellular fluid volume in highly perfused organs and lung water in hypo- and hyper-volaemic dogs. Eur J Anaesthesiol. 1998;15:414–21.
Ishihara H, Suzuki A, Okawa H, Sakai I, Tsubo T, Matsuki A. The initial distribution volume of glucose rather than indocyanine green derived plasma volume is correlated with cardiac output following major surgery. Intensive Care Med. 2000;26:1441–8.
Ishihara H, Suzuki A, Okawa H, Ebina T, Tsubo T, Matsuki A. Comparison of the initial distribution volume of glucose and plasma volume in thoracic fluid accumulated patients. Crit Care Med. 2001;29:1532–8.
Ishihara H, Nakamura H, Okawa H, Yatsu Y, Tsubo T, Hirota K. Comparison of initial distribution volume of glucose and intrathoracic blood volume during hemodynamically unstable states early after esophagectomy. Chest. 2005;128:1713–9.
Orban JC, Blasin-Chadoutaud A, Zolfaghari P, Ishihara H, Grimaud D, Ichai C. Hypovolaemic hypotension after abdominal aortic surgery is predicted by initial distribution volume of glucose. Eur J Anaesthesiol. 2010;27:364–8.
Suzuki A, Ishihara H, Okawa H, Tsubo T, Matsuki A. Can initial distribution volume of glucose predict hypovolemic hypotension after radical surgery for esophageal cancer? Anesth Analg. 2001;92:1146–51.
Ishihara H, Otomo N, Suzuki A, Takamura K, Tsubo T, Matsuki A. Detection of capillary protein leakage by glucose and indocyanine green dilutions during the early post-burn period. Burns. 1998;24:525–31.
Ishida T, Lee T, Shimabukuro T, Niinami H. Right ventricular end-diastolic volume monitoring after cardiac surgery. Ann Thorac Cardiovasc Surg. 2004;10:167–70.
Ishihara H, Nakamura H, Okawa H, Takase H, Tsubo T, Hirota K. Initial distribution volume of glucose can be approximated using a conventional glucose analyzer in the intensive care unit. Crit Care. 2005;9:R144–9.
Hirota K, Ishihara H, Tsubo T, Matsuki A. Estimation of the initial distribution volume of glucose by an incremental plasma glucose level at 3 minutes after i.v. glucose in humans. Br J Clin Pharmacol. 1999;47:361–4.
Wagner JG, Leatherman JW. Right ventricular end-diastolic volume as a predictor of the hemodynamic response to a fluid challenge. Chest. 1998;113:1048–54.
Rocca GD, Costa MG, Feltracco P, Biancofiore G, Begliomini B, Taddei S, Coccia C, Pompei L, Di Marco P, Pietropaoli P. Continuous right ventricular end diastolic volume and right ventricular ejection fraction during liver transplantation: a multicenter study. Liver Transpl. 2008;14:327–32.
Ghoneim M, Pearson K. Pharmacokinetics of drugs administered intravenously. In: Scurr C, Feldman S, Soni N, editors. Scientific foundations of anaesthesia. 4th ed. Chicago: Year Book Medical; 1990. p. 559–571.
Ishihara H, Shimodate Y, Koh H, Isozaki K, Tsubo T, Matsuki A. The initial distribution volume of glucose and cardiac output in critically ill. Can J Anaesth. 1993;40:28–31.
Miyahara A, Okawa H, Ishihara H, Matsuki A. Changes in the initial distribution volume of glucose and plasma volume following volume challenge in dogs. Infusther Transfusmed. 1995;22:274–9.
Ishihara H, Takamura K, Koh H, Iwakawa T, Tsubo T, Matsuki A. Does the initial distribution volume of glucose reflect the central extracellular fluid volume status in critically ill patients? Infusther Transfusmed. 1996;23:196–201.
Biancofiore G, Critchley LA, Lee A, Biandi L, Bisa M, Esposito M, Meacci L, Mozzo R, DeSimone P, Urbani L, Filipponi F. Evaluation of an uncalibrated arterial pulse contour cardiac output monitoring system in cirrhotic patients undergoing liver surgery. Br J Anaesth. 2009;102:47–54.
Critchley L, Lee A, Ho AH. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111:1180–92.
Breukers RM, Sepehrkhouy S, Spiegelenberg SR, Groeneveld AB. Cardiac output measured by a new arterial pressure waveform analysis method without calibration compared with thermodilution after cardiac surgery. J Cardiothorac Vasc Anesth. 2007;21:632–5.
Rose BO, Ishihara H, Okawa H, Panning B, Piepenbrock S, Matsuki A. Repeatability of measurements of the initial distribution volume of glucose in haemodynamically stable patients. J Clin Pharm Ther. 2004;29:317–23.
van Tulder L, Michaeli B, Chiolero R, Berger MM, Revelly JP. An evaluation of initial distribution volume of glucose to assess plasma volume during a fluid challenge. Anesth Analg. 2005;101:1089–93.
Harvey M, Voss L, Sleigh J. Preload response in patients after cardiac surgery: a comparison of systolic pressure and systolic area variability and initial distribution volume of glucose. Crit Care Resusc. 2003;5:171–6.
Ishihara H. Initial distribution volume of glucose early after cardiac surgery. Anesth Analg. 2006;102:1904.
Ishihara H, Giesecke AH. Fluid volume monitoring with glucose dilution. Tokyo: Springer; 2007. p. 23–37.
Hashiba E, Ishihara H, Tsubo T, Okawa H, Hirota K. Use of initial distribution volume of glucose to determine fluid volume loading in pulmonary thromboembolism and right ventricular myocardial infarction. J Anesth. 2008;22:453–6.
Guyton AC, Hall JE. Textbook of medical physiology. 10th ed. Philadelphia: Saunders; 2000. p. 162–83.
Maguire S, Rinehart J, Vakharia S, Cannesson M. Respiratory variation in pulse pressure and plethysmographic waveform: intraoperative applicability in a North American academic center. Anesth Analg. 2011;112:94–6.
He Z, Qiao H, Zhou W, Wang Y, Xu Z, Che X, Zhang J, Liang W. Assessment of cardiac preload status by pulse pressure variation in patients after anesthesia induction: comparison with central venous pressure and initial distribution volume of glucose. J Anesth. 2011;25:812–7.
Scheuren K, Wente MN, Hainer C, Scheffler M, Lichtenstem C, Martin E, Schmidt J, Bopp C, Weigand MA. Left ventricular end-diastolic area is a measure of cardiac preload in patients with early septic shock. Eur J Anaesthesiol. 2009;26:759–65.
Tousignant CP, Walsh F, Mazer CD. The use of transesophageal echocardiography for preload assessment in critically ill patients. Anesth Analg. 2000;90:351–5.
Acknowledgments
The authors are grateful to Professor Paul Hollister (Medical English Center, Hirosaki University Graduate School of Medicine, Hirosaki, Japan) for his useful suggestions.
Conflict of interest
The author(s) declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Saito, J., Ishihara, H., Hashiba, E. et al. Corrected right ventricular end-diastolic volume and initial distribution volume of glucose correlate with cardiac output after cardiac surgery. J Anesth 27, 512–520 (2013). https://doi.org/10.1007/s00540-013-1558-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-013-1558-z