Abstract
Purpose
This retrospective study was performed in order to determine if patients with very severe chronic obstructive pulmonary disease (COPD) have larger main bronchi than patients with less severe disease.
Methods
Charts of patients having had a spirometric evaluation of their COPD and a digitized thin-slice computed tomography (CT) scan between January 2004 and September 2007 were reviewed. Adequate CT scans of male patients [i.e., those allowing a multiplane reconstruction (MPR) of the upper tracheobronchial tree using a double orthogonal oblique method] were divided into two groups: group 1 [forced expiratory volume in 1 s (FEV1) ranging from 30% to 80%] and group 2 (FEV1 < 30%).
Results
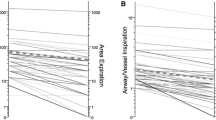
Intraobserver and interobserver coefficients of repeatability were 1.79 and 2.51 mm, respectively. Median values and interquartile ranges of minimum right main bronchial diameter were 11.0 (9.6–12.7) mm versus 12.7 (10.8–13.9) mm in groups 1 (27 patients) and 2 (10 patients), respectively (P = 0.048); values for the minimum left main bronchial diameter were 10.7 (8.9–11.9) mm versus 11.8 (11.2–12.4) mm in groups 1 and 2, respectively (P = 0.040). The difference between the groups in median values of the minimum right and left main bronchial diameters was 1.2 mm. Other values were similar in both groups.
Conclusion
The difference in minimum main bronchial diameters between our two groups corresponded to a difference of two or three sizes of a double-lumen tube. This difference must be taken into account for tube selection for such patients. Further studies are needed to prove that CT scan MPR can improve patients’ intraoperative care.



Similar content being viewed by others
References
Jeon Y, Ryu HG, Bahk JH, Jung CW, Goo JM. A new technique to determine the size of double-lumen endobronchial tubes by the two perpendicularly measured bronchial diameters. Anaesth Intensive Care. 2005;33:59–63.
Brodsky JB, Adkins MO, Gaba DM. Bronchial cuff pressures of double-lumen tubes. Anesth Analg. 1989;69:608–10.
Bardoczky G, d’Hollander A, Yernault JC, Van Meuylem A, Moures JM, Rocmans P. On-line expiratory flow-volume curves during thoracic surgery: occurrence of auto-PEEP. Br J Anaesth. 1994;72:25–8.
Dal Corso B, Tanaskovic G, Mastropasqua D, Luzzani A. Iatrogenic rupture of the left mainstem bronchus in tracheobronchial intubation. Minerva Anestesiol. 1998;64:581–5.
Amar D, Desiderio DP, Heerdt PM, Kolker AC, Zhang H, Thaler HT. Practice patterns in choice of left double-lumen tube size for thoracic surgery. Anesth Analg. 2008;106:379–83.
Lohser J, Brodsky JB. Tracheal perforation from double-lumen tubes: size may be important. Anesth Analg. 2005;101:1243–4.
Slinger P, Sullivan EA. Anesthetic management for surgery of the lungs and mediastinum. In: Hensley FA, editor. A practical approach to cardiac anesthesia. 3rd ed. Philadelphia: Lippincott; 2003. p. 658.
Olivier P, Hayon-Sonsino D, Convard JP, Laloe PA, Fischler M. Measurement of left mainstem bronchus using multiplane CT reconstructions and relationship between patient characteristics or tracheal diameters and left bronchial diameters. Chest. 2006;130:101–7.
Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, Zielinski J. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532–55.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Russell WJ, Strong TS. Dimensions of double-lumen tracheobronchial tubes. Anaesth Intensive Care. 2003;31:50–3.
Jesseph JE, Merendino KA. The dimensional interrelationships of the major components of the human tracheobronchial tree. Surg Gynecol Obstet. 1957;105:210–4.
Chow MY, Liam BL, Thng CH, Chong BK. Predicting the size of a double-lumen endobronchial tube using computed tomographic scan measurements of the left main bronchus diameter. Anesth Analg. 1999;88:302–5.
Hagihira S, Takashina M, Mashimo T. Application of a newly designed right-sided, double-lumen endobronchial tube in patients with a very short right mainstem bronchus. Anesthesiology. 2008;109:565–8.
Montaudon M, Berger P, Cangini-Sacher A, de Dietrich G, Tunon-de-Lara JM, Marthan R, Laurent F. Bronchial measurement with three-dimensional quantitative thin-section CT in patients with cystic fibrosis. Radiology. 2007;242:573–81.
Niimi A, Matsumoto H, Amitani R, Nakano Y, Mishima M, Minakuchi M, Nishimura K, Itoh H, Izumi T. Airway wall thickness in asthma assessed by computed tomography. Relation to clinical indices. Am J Respir Crit Care Med. 2000;162:1518–23.
Matsumoto H, Niimi A, Tabuena RP, Takemura M, Ueda T, Yamaguchi M, Matsuoka H, Jinnai M, Chin K, Mishima M. Airway wall thickening in patients with cough variant asthma and nonasthmatic chronic cough. Chest. 2007;131:1042–9.
Hannallah MS, Benumof JL, Ruttimann UE. The relationship between left mainstem bronchial diameter and patient size. J Cardiothorac Vasc Anesth. 1995;9:119–21.
Hampton T, Armstrong S, Russell WJ. Estimating the diameter of the left main bronchus. Anaesth Intensive Care. 2000;28:540–2.
Brodsky JB, Macario A, Mark JB. Tracheal diameter predicts double-lumen tube size: a method for selecting left double-lumen tubes. Anesth Analg. 1996;82:861–4.
Chow MY, Liam BL, Lew TW, Chelliah RY, Ong BC. Predicting the size of a double-lumen endobronchial tube based on tracheal diameter. Anesth Analg. 1998;87:158–60.
King GG, Muller NL, Pare PD. Evaluation of airways in obstructive pulmonary disease using high-resolution computed tomography. Am J Respir Crit Care Med. 1999;159:992–1004.
Edwards PD, Bull RK, Brown VS, Curtin J. Spiral CT optimization for measurement of bronchial lumen diameter using an experimental model. Br J Radiol. 2000;73:715–9.
Haraguchi M, Shimura S, Shirato K. Morphometric analysis of bronchial cartilage in chronic obstructive pulmonary disease and bronchial asthma. Am J Respir Crit Care Med. 1999;159:1005–13.
Bosken CH, Wiggs BR, Pare PD, Hogg JC. Small airway dimensions in smokers with obstruction to airflow. Am Rev Respir Dis. 1990;142:563–70.
Kuwano K, Bosken CH, Pare PD, Bai TR, Wiggs BR, Hogg JC. Small airways dimensions in asthma and in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1993;148:1220–5.
Hasegawa M, Nasuhara Y, Onodera Y, Makita H, Nagai K, Fuke S, Ito Y, Betsuyaku T, Nishimura M. Airflow limitation and airway dimensions in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173:1309–15.
Matsuoka S, Kurihara Y, Yagihashi K, Hoshino M, Nakajima Y. Airway dimensions at inspiratory and expiratory multisection CT in chronic obstructive pulmonary disease: correlation with airflow limitation. Radiology. 2008;248:1042–9.
Nakano Y, Muro S, Sakai H, Hirai T, Chin K, Tsukino M, Nishimura K, Itoh H, Pare PD, Hogg JC, Mishima M. Computed tomographic measurements of airway dimensions and emphysema in smokers. Correlation with lung function. Am J Respir Crit Care Med. 2000;162:1102–8.
Ohara T, Hirai T, Sato S, Sato A, Nishioka M, Muro S, Mishima M. Comparison of airway dimensions in different anatomic locations on chest CT in patients with COPD. Respirology. 2006;11:579–85.
Jokinen K, Palva T, Sutinen S, Nuutinen J. Acquired tracheobronchomalacia. Ann Clin Res. 1977;9:52–7.
Loring SH, O’Donnell CR, Feller-Kopman DJ, Ernst A. Central airway mechanics and flow limitation in acquired tracheobronchomalacia. Chest. 2007;131:1118–24.
Iwamoto T, Takasugi Y, Hiramatsu K, Koga Y, Konishi T, Kozuka K, Murakami T. Three-dimensional CT image analysis of a tracheal bronchus in a patient undergoing cardiac surgery with one-lung ventilation. J Anesth. 2009;23:260–5.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Mourissoux, G., Vandendries, C., Neveu, H. et al. Main bronchial diameters in patients with very severe COPD. J Anesth 24, 359–365 (2010). https://doi.org/10.1007/s00540-010-0924-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-010-0924-3