Abstract
A 61-year-old woman with chronic renal failure (CRF) associated with Alport syndrome underwent coronary artery aneurysmectomy under general anesthesia. Hemorrhage control was difficult during the surgery, and she became hemodynamically unstable. The surgery and anesthesia lasted 446 and 552 min, respectively. On postoperative day 1, she developed severe respiratory distress several minutes after extubation. Her trachea was immediately reintubated. The second attempt to extubate her trachea also failed. Fiberoptic examination revealed bilateral vocal cord paralysis (VCP) due to recurrent laryngeal nerve (RLN) paralysis. Although she needed a temporary tracheostomy, vocal cord movement recovered without treatment 3 months after surgery. The mechanisms underlying her symptoms may be multifactorial: the first and foremost factor was that she had been receiving maintenance hemodialysis for 20 years since being diagnosed with Alport syndrome. We speculated that RLN vulnerability due to Alport syndrome and CRF strengthened her symptoms. We also recognized that the long-lasting mechanical stress and low perfusion to the RLN due to hemodynamic instability during surgery were indispensable contributory factors to the development of VCP. This is the first report of postoperative bilateral VCP in a patient with CRF related to Alport syndrome. Based on this experience, we strongly recommend preoperative detailed examination of vocal cord function in patients with CRF associated with Alport syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vocal cord paralysis (VCP) following general anesthesia is a rare entity [1]. The most frequent etiology is a direct injury to the recurrent laryngeal nerve (RLN) as a result of surgical manipulation, such as thyroidectomy [2]. In some cases, however, VCP may occur as a complication of anesthetic practice, such as tracheal intubation, laryngeal mask airway insertion, central venous cannulation, and transesophageal echocardiography (TEE) probe insertion [3–6]. Anesthesiologists must therefore be aware that VCP may occur as a result of various procedures. VCP usually develops unilaterally; bilateral occurrences are extremely rare [1]. Here, we report a case of bilateral VCP following coronary artery aneurysmectomy in a patient with chronic renal failure (CRF) associated with Alport syndrome. In this report, we discuss the patient’s multiple risk factors for developing VCP and conclude that a detailed preoperative examination of vocal cord function, such as a fiberoptic laryngeal examination and stroboscopy, is required in certain patient groups. Consent for the publication of this report was obtained from the patient’s family, in accordance with the patient health information guidelines of the Medical Ethics Committee of the University of Tsukuba.
Case report
A 61-year-old woman (150 cm, 40 kg) with Alport syndrome was scheduled for resection of a coronary aneurysm. Her medical history was significant for CRF, for which she was receiving maintenance hemodialysis three times a week. She also had a history of depression for which she was currently being treated with sulpiride and olanzapine. The patient had undergone parathyroidectomy 13 years previously under general anesthesia without any trouble. On admission, she presented with no respiratory symptoms or speech disturbance. The preoperative important findings were remarkable for antipsychotic drug-induced hypotension, i.e., she always needed an infusion of sympathomimetic agents during hemodialysis. She felt chest discomfort and general fatigue when her systemic BP fell below 60 mmHg. She was receiving amezinium and droxydopa daily for refractory hypotension. The preoperative abnormal values were: pH, 7.278; hemoglobin, 11.3 g dl−1; blood urea nitrogen, 54.3 mg dl−1; serum creatinine, 7.7 mg dl−1 (after hemodialysis). The chest roentgenogram showed severe cardiomegaly (cardio-thoracic ratio 80%).
General anesthesia was induced and maintained with midazolam, remifentanil, and fentanyl. Tracheal intubation was facilitated by vecuronium, and her trachea was easily intubated with a 7.0-mm internal diameter tracheal tube. Cuff pressure was monitored intermittently and adjusted to below 20 cm H2O throughout surgery using a cuff inflator and a pressure monitor device. A pulmonary artery catheter was inserted without difficulty via the right internal jugular vein through an introducer sheath. A TEE probe (S7-2 Omni TEE; Philips Medical Systems, Andover, MA) was inserted and handled without difficulty during surgery. Upon removal of the TEE probe, there was no blood on the probe cover. The surgery was performed through a median sternotomy and cardiopulmonary bypass (CPB) with the patient in supine position. Conventional cannulation of the ascending aorta and right atrial appendage was performed. Intraoperative cardiac arrest was induced and maintained with a standard cardioplegic solution. Topical cooling with ice slush was not used. Her intraoperative course was eventful for refractory hypotension (perfusion pressure of approx. 40 mmHg) and severe dilutional anemia (minimum hemoglobin concentration 3.7 g dl−1) during CPB. After the discontinuation of CPB, she became hemodynamically unstable, and red blood cell products, fresh frozen plasma, and platelet concentrate had to be administered to control oozing. It took a long time to achieve hemostasis. The duration of anesthesia and surgery was 552 and 446 min, respectively. During surgery, she had a positive fluid balance of about 10 l. She was admitted to the intensive care unit (ICU) with tracheal intubation and required continuous infusions of dopamine (12 μg kg−1min−1) and noradrenaline (0.4 μg kg−1min−1).
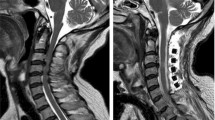
Fourteen hours after the completion of the surgery, attempts were made to extubate her trachea. Before extubation, her arterial blood gas values were: pH 7.42; \( {\text{P}}_{{{\text{CO}}_{ 2} }} \) , 37 mmHg; \( {\text{P}}_{{{\text{O}}_{ 2} }} \) , 86 mmHg (FiO2 0.4, continuous positive airway pressure, CPAP). However, she developed respiratory insufficiency and inspiratory stridor. Arterial blood gas values revealed a pH of 7.31, \( {\text{P}}_{{{\text{CO}}_{ 2} }} \) of 50 mmHg, and \( {\text{P}}_{{{\text{O}}_{ 2} }} \) of 63 mmHg (O2 8 l min−1 via a face mask). She was reintubated, and her respiratory distress resolved dramatically. Because of the excessive intraoperative positive fluid balance, we originally assumed that her extubation failure was due to fluid overload during surgery. On postoperative day 4, we attempted to extubate her trachea under fiberoptic observation, suspecting that she may have also suffered VCP. During the extubation, an anesthesiologist and an otolaryngologist witnessed that the bilateral vocal cords were fixed at the midline position without vocal cord edema or dislocation of the arytenoids. We therefore made a diagnosis of bilateral RLN paralysis. Her trachea was intubated again, but this time with a smaller tracheal tube (internal diameter 6.0 mm) and an Airtraq (Prodol Meditec, Vizcaya, Spain). The tracheostomy that had been planned was suspended due to infection at the surgical site. On postoperative day 10, we performed a tracheostomy, and the patient’s respiratory condition stabilized so that she could be weaned from the ventilator (10 days after the tracheostomy). While being weaned from the ventilator, she became mentally unstable and required an increased quantity of antipsychotics. Although her postoperative course was complicated by an exacerbation of depression and by sternal wound infection, her vocal cord movement gradually resolved spontaneously, and the tracheostomy tube could be removed 3 months after surgery.
Discussion
We experienced a postoperative VCP in a patient with CRF associated with Alport syndrome. VCP is a relatively rare entity. Kikura [1] recently reviewed 31,241 cases of general anesthesia with tracheal intubation and reported that the incidence of postoperative VCP was 0.077%. Previous reports suggest that VCP can be caused by anesthetic practices, such as intubation of the trachea and insertion of a laryngeal mask airway [1, 4] or by the insertion of a nasogastric tube or TEE probe [6]. Most VCPs related to anesthetic practice occur as a consequence of indirect pressure to the RLN and are transient. Indirect pressure neurapraxia usually resolves without treatment within a few weeks to months. In some cases, however, even indirect pressure produces a paralysis of the RLN that lasts several months and requires temporary tracheostomy. Most VCPs occur unilaterally; the bilateral condition accounts for about 3% of all VCP [3].
The mechanisms underlying our patient’s VCP may be multifactorial. First, the patient’s CRF related to Alport syndrome may have contributed to her RLN paralysis. Alport syndrome is a progressive, hereditary glomerulonephritis that is associated with high-tone sensorineural deafness and characteristic eye signs. Mutation in type 4 collagen, a main component of the basement membranes, is a known etiology of the disease. The perineurium and endoneurium contain type 4 collagen in abundance; therefore, the close relationship between Alport syndrome and neuropathy is comprehensible. However, a literature search did not reveal any published mention of a relationship between nerve paralysis and Alport syndrome. The disease is most commonly inherited as an X-linked disorder, with a gene frequency of 1 in 5,000; consequently, female patients are affected less often and more difficult to diagnose. Given this background, particular caution should be exercised when female patients who have Alport syndrome are being treated. Additionally, it is well known that CRF patients have various neurological complications and are more susceptible than healthy patients to neuronal injury [7]. As such, metabolic and circulatory disturbances of the neurons may be present in CRF patients. There is also a close relationship between neurological disorders and VCP; for example, bilateral VCP associated with diabetes mellitus or Shy–Drager syndrome has been reported [8, 9].
Second, the type of surgery may have affected the severity of our patient’s symptoms. Postoperative VCP occurs more frequently during cardiac surgery than during other types of surgeries [3]. The longer duration of the surgery and the use of CPB are associated with this higher incidence of VCP [3]. Median sternotomy with sternal retraction is known to stretch the RLN laterally, and in patients with cardiomegaly, surgeons tend to retract the chest wall more excessively to visualize the surgical field [10]. Manipulation of the aorta and its main branches is also associated with an additional risk of VCP [11]. Patients who undergo cardiac surgery are more prone to intraoperative hemodynamic instability [12], which may partially explain the higher frequency of postoperative VCP in such cases. In our case, the long duration of the surgical procedure and the CPB may also have played an important role in the development of VCP. Moreover, intraoperative severe anemia and low perfusion pressure may have worsened her symptoms still further. Last but not least, repeated reintubation after the operation greatly affected her respiratory problem.
Third, we speculate that the patient’s RLN was subclinically damaged at the time of her parathyroidectomy, which had been performed uneventfully 13 years previously. According to her family, however, she never showed any symptoms of VCP or hoarseness, and her complete recovery from VCP indicated that her RLN was intact before the present surgery. In a previous study, simple voice assessment (say ‘hello’ and coughing) had a positive predictive value of 55% for VCP [13], with a definite diagnosis based on fiberoptic laryngeal examination and stroboscopy. In patients at high risk for postoperative VCP, preoperative evaluation with these diagnostic tools may be useful.
To the best of our knowledge, this is the first case report of bilateral VCP in a patient with Alport syndrome. Neural vulnerability exists in all CRF patients, but especially in those with Alport syndrome. All of the factors listed above may have synergistically contributed to our patient’s severe VCP. In patients with Alport syndrome who have already developed CRF, surgeons should be extremely cautious to avoid VCP and to evaluate vocal cord function in detail prior to surgery. Based on our case study, we recommend a perioperative detailed examination, including stroboscopy and video laryngoscopy, in this patient population. If abnormal findings are identified, the treating physicians should obtain preoperative informed consent and carry out intraoperative monitoring of recurrent nerve function via tracheal tube (the NIM EMG Endotracheal Tube, for example) and a careful postoperative follow-up. As tracheal intubation is the most common cause of vocal cord damage among anesthesia practices, recording the fiberoptic view of a trachea during intubation may be useful.
References
Kikura M, Suzuki K, Itagaki T, Takada T, Sato S. Age and comorbidity as risk factors for vocal cord paralysis associated with tracheal intubation. Br J Anaesth. 2007;98:524–30.
Feehery JM, Pribitkin EA, Heffelfinger RN, Lacombe VG, Lee D, Lowry LD, Keane WM, Sataloff RT. The evolving etiology of bilateral vocal fold immobility. J Voice. 2003;17:76–81.
Dimarakis I, Protopapas AD. Vocal cord palsy as a complication of adult cardiac surgery: surgical correlations and analysis. Eur J Cardiothorac Surg. 2004;26:773–5.
Endo K, Okabe Y, Maruyama Y, Tsukatani T, Furukawa M. Bilateral vocal cord paralysis caused by laryngeal mask airway. Am J Otolaryngol. 2007;28:126–9.
Salman M, Potter M, Ethel M, Myint F. Recurrent laryngeal nerve injury: a complication of central venous catheterization—a case report. Angiology. 2004;55:345–6.
Sakai T, Terao Y, Miyata S, Hasuo H, Haseba S, Yano K. Postoperative recurrent laryngeal nerve palsy following a transesophageal echocardiography (in Japanese with English abstract). Masui (Jpn J Anesthesiol). 1999;48:656–7.
Brouns R, De Deyn PP. Neurological complications in renal failure: a review. Clin Neurol Neurosurg. 2004;107:1–16.
Sommer DD, Freeman JL. Bilateral vocal cord paralysis associated with diabetes mellitus: case reports. J Otolaryngol. 1994;23:169–71.
Bawa R, Ramadan HH, Wetmore SJ. Bilateral vocal cord paralysis with Shy–Drager syndrome. Otolaryngol Head Neck Surg. 1993;109:911–4.
Hamdan AL, Moukarbel RV, Farhat F, Obeid M. Vocal cord paralysis after open-heart surgery. Eur J Cardiothorac Surg. 2002;21:671–4.
Ishimoto S, Ito K, Toyama M, Kawase I, Kondo K, Oshima K, Niimi S. Vocal cord paralysis after surgery for thoracic aortic aneurysm. Chest. 2002;121:1911–5.
Itagaki T, Kikura M, Sato S. Incidence and risk factors of postoperative vocal cord paralysis in 987 patients after cardiovascular surgery. Ann Thorac Surg. 2007;83:2147–52.
Hanna BC, Brooker DS. A preliminary study of simple voice assessment in a routine clinical setting to predict vocal cord paralysis after thyroid or parathyroid surgery. Clin Otolaryngol. 2008;33:63–6.
Acknowledgments
The authors are very grateful to Ms. F. Miyamasu, Associate Professor at the University of Tsukuba, for revising the English of this manuscript.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Watanabe, K., Hagiya, K., Inomata, S. et al. Bilateral vocal cord paralysis in a patient with chronic renal failure associated with Alport syndrome. J Anesth 24, 472–475 (2010). https://doi.org/10.1007/s00540-010-0903-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-010-0903-8