Abstract
Background
Individuals with celiac disease (CD) are at increased risk of lymphoproliferative malignancy (LPM). We examined if a family history of LPM or any cancer influenced the risk of LPM in individuals with CD.
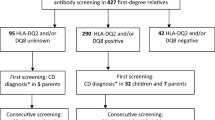
Methods
We identified 28,996 individuals with biopsy-verified CD (equal to villous atrophy, Marsh histopathology stage 3), of whom 616 had family history of LPM. Cox regression then estimated hazard ratios (HRs) for LPM in these 616 compared with two control groups. We also examined the risk of LPM in CD individuals with a family history of any cancer (n = 8,439).
Results
During follow-up, 2/616 CD individuals with a family history of LPM, and 235/28,380 CD individuals without a family history of LPM developed LPM themselves. CD individuals with a family history of LPM were not at increased risk of LPM compared to general population controls (HR = 1.18; 95 % CI = 0.27–5.10), or compared to CD individuals without a family history of LPM (adjusted HR = 0.31; 95 % CI = 0.08–1.23). We found no increased risk of LPM in CD individuals with a family history of any cancer.
Conclusion
This study found no evidence that a family history of LPM or any cancer increases the risk of future LPM in individuals with CD. Despite the large number of study participants, this study is nevertheless limited by few positive events due to a low absolute risk of LPM even in individuals with CD.

Similar content being viewed by others
Abbreviations
- CD:
-
Celiac disease
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- LPM:
-
Lymphoproliferative malignancy
- NHL:
-
Non-Hodgkin lymphoma
- OR:
-
Odds ratio
- VA:
-
Villous atrophy
References
Ludvigsson JF, Leffler DA, Bai JC, Biagi F, Fasano A, Green PH, et al. The Oslo definitions for coeliac disease and related terms. Gut. 2013;62:43–52.
Dube C, Rostom A, Sy R, Cranney A, Saloojee N, Garritty C, et al. The prevalence of celiac disease in average-risk and at-risk Western European populations: a systematic review. Gastroenterology. 2005;128:S57–67.
Tio M, Cox MR, Eslick GD. Meta-analysis: coeliac disease and the risk of all-cause mortality, any malignancy and lymphoid malignancy. Aliment Pharmacol Ther. 2012;35:540–51.
Askling J, Linet M, Gridley G, Halstensen TS, Ekstrom K, Ekbom A. Cancer incidence in a population-based cohort of individuals hospitalized with celiac disease or dermatitis herpetiformis. Gastroenterology. 2002;123:1428–35.
Anderson LA, McMillan SA, Watson RG, Monaghan P, Gavin AT, Fox C, et al. Malignancy and mortality in a population-based cohort of patients with coeliac disease or “gluten sensitivity”. World J Gastroenterol. 2007;13:146–51.
Catassi C, Fabiani E, Corrao G, Barbato M, De Renzo A, Carella AM, et al. Risk of non-Hodgkin lymphoma in celiac disease. JAMA. 2002;287:1413–9.
Elfstrom P, Granath F, Ekstrom Smedby K, Montgomery SM, Askling J, Ekbom A, et al. Risk of lymphoproliferative malignancy in relation to small intestinal histopathology among patients with celiac disease. J Natl Cancer Inst. 2011;103:436–44.
Gao Y, Kristinsson SY, Goldin LR, Bjorkholm M, Caporaso NE, Landgren O. Increased risk for non-Hodgkin lymphoma in individuals with celiac disease and a potential familial association. Gastroenterology. 2009;136:91–8.
Mearin ML, Catassi C, Brousse N, Brand R, Collin P, Fabiani E, et al. European multi-centre study on coeliac disease and non-Hodgkin lymphoma. Eur J Gastroenterol Hepatol. 2006;18:187–94.
Smedby KE, Hjalgrim H, Askling J, Chang ET, Gregersen H, Porwit-MacDonald A, et al. Autoimmune and chronic inflammatory disorders and risk of non-Hodgkin lymphoma by subtype. J Natl Cancer Inst. 2006;98:51–60.
West J, Logan RF, Smith CJ, Hubbard RB, Card TR. Malignancy and mortality in people with coeliac disease: population based cohort study. BMJ. 2004;329:716–9.
Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992–2001. Blood. 2006;107:265–76.
Smedby KE, Askling J, Mariette X, Baecklund E. Autoimmune and inflammatory disorders and risk of malignant lymphomas—an update. J Intern Med. 2008;264:514–27.
Linet MS, Pottern LM. Familial aggregation of hematopoietic malignancies and risk of non-Hodgkin’s lymphoma. Cancer Res. 1992;52:5468s–73s.
Goldgar DE, Easton DF, Cannon-Albright LA, Skolnick MH. Systematic population-based assessment of cancer risk in first-degree relatives of cancer probands. J Natl Cancer Inst. 1994;86:1600–8.
Altieri A, Bermejo JL, Hemminki K. Familial risk for non-Hodgkin lymphoma and other lymphoproliferative malignancies by histopathologic subtype: the Swedish Family-Cancer Database. Blood. 2005;106:668–72.
Wang SS, Slager SL, Brennan P, Holly EA, De Sanjose S, Bernstein L, et al. Family history of hematopoietic malignancies and risk of non-Hodgkin lymphoma (NHL): a pooled analysis of 10 211 cases and 11 905 controls from the International Lymphoma Epidemiology Consortium (InterLymph). Blood. 2007;109:3479–88.
Goldin LR, Bjorkholm M, Kristinsson SY, Turesson I, Landgren O. Highly increased familial risks for specific lymphoma subtypes. Br J Haematol. 2009;146:91–4.
Au WY, Gascoyne RD, Klasa RD, Connors JM, Gallagher RP, Le ND, et al. Incidence and spectrum of non-Hodgkin lymphoma in Chinese migrants to British Columbia. Br J Haematol. 2005;128:792–6.
Straus SE, Jaffe ES, Puck JM, Dale JK, Elkon KB, Rosen-Wolff A, et al. The development of lymphomas in families with autoimmune lymphoproliferative syndrome with germline Fas mutations and defective lymphocyte apoptosis. Blood. 2001;98:194–200.
Ludvigsson JF, Brandt L, Montgomery SM, Granath F, Ekbom A. Validation study of villous atrophy and small intestinal inflammation in Swedish biopsy registers. BMC Gastroenterol. 2009;9:19.
Marsh MN. Gluten, major histocompatibility complex, and the small intestine. A molecular and immunobiologic approach to the spectrum of gluten sensitivity (‘celiac sprue’). Gastroenterology. 1992;102:330–54.
Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24:659–67.
Ludvigsson JF, Montgomery SM, Ekbom A, Brandt L, Granath F. Small-intestinal histopathology and mortality risk in celiac disease. JAMA. 2009;302:1171–8.
Mattsson B, Wallgren A. Completeness of the Swedish Cancer Register. Non-notified cancer cases recorded on death certificates in 1978. Acta Radiol Oncol. 1984;23:305–13.
Swedish Cancer Registry, by the Swedish National Board of Health and Welfare. http://www.socialstyrelsen.se/register/halsodataregister/cancerregistret/inenglish.
Barlow L, Westergren K, Holmberg L, Talback M. The completeness of the Swedish Cancer Register: a sample survey for year 1998. Acta Oncol. 2009;48:27–33.
Ekbom A. The Swedish Multi-generation Register. Methods Mol Biol. 2011;675:215–20.
Leslie LA, Lebwohl B, Neugut AI, Gregory Mears J, Bhagat G, Green PH. Incidence of lymphoproliferative disorders in patients with celiac disease. Am J Hematol. 2012;87:754–9.
Grainge MJ, West J, Solaymani-Dodaran M, Card TR, Logan RF. The long-term risk of malignancy following a diagnosis of coeliac disease or dermatitis herpetiformis: a cohort study. Aliment Pharmacol Ther. 2012;35:730–9.
Nogai H, Dorken B, Lenz G. Pathogenesis of non-Hodgkin’s lymphoma. J Clin Oncol. 2011;29:1803–11.
Olen O, Askling J, Ludvigsson JF, Hildebrand H, Ekbom A, Smedby KE. Coeliac disease characteristics, compliance to a gluten free diet and risk of lymphoma by subtype. Dig Liver Dis. 2011;43:862–8.
Godfrey JD, Brantner TL, Brinjikji W, Christensen KN, Brogan DL, Van Dyke CT, et al. Morbidity and mortality among older individuals with undiagnosed celiac disease. Gastroenterology. 2010;139:763–9.
Elli L, Contiero P, Tagliabue G, Tomba C, Bardella MT. Risk of intestinal lymphoma in undiagnosed coeliac disease: results from a registered population with different coeliac disease prevalence. Dig Liver Dis. 2012;44:743–7.
Lohi S, Maki M, Rissanen H, Knekt P, Reunanen A, Kaukinen K. Prognosis of unrecognized coeliac disease as regards mortality: a population-based cohort study. Ann Med. 2009;41:508–15.
Lohi S, Maki M, Montonen J, Knekt P, Pukkala E, Reunanen A, et al. Malignancies in cases with screening-identified evidence of coeliac disease: a long-term population-based cohort study. Gut. 2009;58:643–7.
Canavan C, Logan RF, Khaw KT, West J. No difference in mortality in undetected coeliac disease compared with the general population: a UK cohort study. Aliment Pharmacol Ther. 2011;34:1012–9.
Castillo JJ, Dalia S. Cigarette smoking is associated with a small increase in the incidence of non-Hodgkin lymphoma: a meta-analysis of 24 observational studies. Leuk Lymphoma. 2012;53:1911–9.
Austin AS, Logan RF, Thomason K, Holmes GK. Cigarette smoking and adult coeliac disease. Scand J Gastroenterol. 2002;37:978–82.
Snook JA, Dwyer L, Lee-Elliott C, Knan S, Wheeler DW, Nicholas DS, et al. Smoking benefits celiac sprue and pouchitis: implications for nicotine therapy? Gastroenterology. 1997;112:1048–50.
Ludvigsson JF, Brandt L, Montgomery SM. Symptoms and signs in individuals with serology positive for celiac disease but normal mucosa. BMC Gastroenterol. 2009;9:57.
Pais WP, Duerksen DR, Pettigrew NM, Bernstein CN. How many duodenal biopsy specimens are required to make a diagnosis of celiac disease? Gastrointest Endosc. 2008;67:1082–7.
Corazza GR, Villanacci V, Zambelli C, et al. Comparison of the interobserver reproducibility with different histologic criteria used in celiac disease. Clin Gastroenterol Hepatol. 2007;5(7):838–43.
Acknowledgments
JFL: Örebro University Hospital, Karolinska Institutet, the Swedish Society of Medicine, the Swedish Research Council—Medicine (522-2A09-195), the Swedish Celiac Society, the Fulbright commission. BL: The American Scandinavian Foundation, the Celiac Sprue Association, and the National Center for Research Resources, a component of the National Institutes of Health (KL2 RR024157). JAM: The National Institutes of Health—DK071003 and DK057892. AE was supported by Stockholm county council (ALF).
Conflict of interest
JAM: Grant support: Alba Therapeutics (>$50,000 USD); Advisory board: Alvine Pharmaceuticals, Inc. (<$10,000 USD), Nexpep (<$10,000 USD), Consultant (none above 10,000 USD): Ironwood, Inc., Flamentera, Actogenix, Ferring Research Institute inc., Bayer Healthcare Pharmaceuticals, Vysera Biomedical, 2G Pharma, Inc, ImmunosanT, Inc and Shire US Inc. With the exception of JAM, all authors declare that they have no conflicts of interest and nothing to declare.
Ethical approval
This project (2006/633-31/4) was approved by the Research Ethics Committee of the Karolinska Institute, Sweden on June 14, 2006.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
The Swedish histopathology SnoMed classification compared to other international histopathology classifications.
Comparison of small intestinal histopathology classifications [43]
Classification used in this project | Villous atrophy | |||
|---|---|---|---|---|
Marsh classification | Type IIIa | Type IIIb | Type IIIc | |
Marsh description | Flat destructive | |||
Corazza et al. [43] | Grade B1 | Grade B2 | ||
SnoMed codes | M58, D6218, M58005 | M58, D6218, M58006 | M58, D6218, M58007 | |
KVAST/Alexander classification | III partial VA | IV subtotal VA | IV total VA | |
Characteristics | ||||
Villous atrophy | + | ++ | ++ | |
IEL | + | + | + | |
Crypt hyperplasia | + | ++ | ++ | |
Rights and permissions
About this article
Cite this article
Ludvigsson, J.F., Lebwohl, B., Rubio-Tapia, A. et al. Risk of lymphoproliferative malignancy in celiac patients with a family history of lymphoproliferative malignancy. J Gastroenterol 48, 1324–1331 (2013). https://doi.org/10.1007/s00535-013-0757-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-013-0757-6