Abstract
Background
Prostate cancer (PCa) is the most prevalent type of cancer in men in the UK. Exercise has been shown to improve the health and quality of life of PCa patients. Exercise should be easily accessible to men with PCa regardless of socioeconomic group or ethnicity. There is a need to better understand whether the current evidence base for exercise interventions is representative and inclusive of racial and ethnic minority men with PCa.
Methods
A systematic review of the literature was conducted according to PRISMA guidelines and prospectively registered via Prospero (ID: CRD42022384373). The MEDLINE Ovid, Cochrane Library and PubMed databases were searched from inception to December 2022. The search strategy keywords and MeSH terms used included the following: (1) exercise, (2) training, (3) prostate cancer, (4) ethnic and (5) diversity.
Results
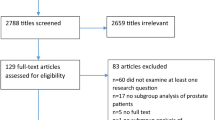
A total of 778 records were retrieved from database searches, of which 15 records were duplicates. A further 649 were eliminated following the screening of titles and abstracts. After full-text screening of 186 articles, 28 manuscripts were included for review.
Conclusion
This systematic review highlights that there is high heterogeneity in the reporting of participants’ ethnicity and there are low numbers of ethnic minority men included in PCa and exercise studies in the UK. Further work is required to understand why representation is lacking within PCa exercise trials in the UK and strategies are needed to achieve representation from all ethnic groups.
Implications for cancer survivors
Improved representation and reporting of ethnicity in exercise trials is vital to ensure the results are applicable to all patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Prostate cancer (PCa) is the most prevalent type of cancer in men in the UK, with approximately 55,100 confirmed new cases each year and a further 1.4 million worldwide [1, 2]. Effective treatments for localised and metastatic PCa are recognised to have side effects which may be associated with negative impacts on patients’ quality of life, functional status and physical and mental health [3,4,5,6]. Despite advances in PCa management and improvements in outcomes driven by clinical trials, it is recognised that significant PCa health disparity remains due to a poorly understood, complex interplay of factors [7]. It is well documented that Black men are at a 2.1 times greater risk of being diagnosed with PCa (23.5–37.2%) compared to individuals of White (13.2–15.0%) or Asian (6.3–10.5%) ethnicity [8, 9]. Black men are more likely to be diagnosed at a younger age and with a more advanced stage PCa compared to men of other ethnicities. Advanced PCa can have a significant impact on patients’ survival, quality of life and ability to carry out activities of daily living effectively [10].
Exercise has been demonstrated to improve the health outcomes and quality of life of men with PCa [11,12,13]. The evidence supporting the benefits of exercise in men with PCa has become more compelling over the past decade, to the extent that exercise is recommended in current national and international PCa guidelines [14, 15]. The effect of aerobic, resistance and flexibility exercise on patients’ outcomes at different stages of the pathway and in multiple settings for example home, community and hospital has been researched over varying durations [16, 17]. Exercise during and after PCa treatment is safe and effective at improving important health outcomes, including improved aerobic capacity and body composition [6, 11, 18]. Varying exercise modalities have been shown to improve body composition, strength, blood pressure, blood biomarkers such as plasma triglycerides and fasting plasma glucose, aerobic capacity, quality of life and attenuate fatigue [11, 12, 19,20,21]. Interventions involving combined exercise modalities, such as aerobic and strength training concurrently, have been demonstrated to improve bone density [6].
Exercise opportunities should be easily accessible to men with PCa regardless of racial or ethnic minority status. Recent reports have highlighted that diversity and representation are poor in PCa clinical trials, with approximately 96% of men participating in PCa research being White [22]. There is a need to understand whether the present evidence base for exercise interventions is representative and inclusive of racial and ethnic minority men with PCa and, if not, explore the barriers and seek tailored acceptable interventions or strategies which are more inclusive. The aim of this systematic review is to examine current reporting of race and ethnicity data and strategies to increase inclusivity and demographic representation within PCa and exercise trials.
Methods
Protocol and registration
The preferred reporting items for systematic review and meta-analyses (PRISMA) guidelines were followed when conducting and reporting this prospectively registered systematic review (PROSPERO ID: CRD42022384373) [23].
Eligibility criteria
We included trials published in the English language that studied exercise interventions in PCa patients. Manuscripts were excluded if they were protocols, reports, conference abstracts, position statements or case series reports. Participants must have been aged > 16 years and have been diagnosed with PCa. Studies could include any form of exercise intervention in isolation or combined with other lifestyle factors such as nutritional supplementation or smoking cessation. Studies that included either details of participants’ ethnicity or strategies to ensure inclusion and representation were eligible.
Search strategy
The MEDLINE Ovid, Cochrane Library and PubMed databases were searched from inception to July 2024. The search strategy keywords and MeSH terms used included the following: (1) exercise, (2) training, (3) prostate cancer, (4) ethnic and (5) diversity. Reference lists of all relevant systematic reviews identified were searched for additional studies. All searches were conducted by the same author (RA), with search results collated using Rayyan software [24], and duplicates were removed. All titles, abstracts and full texts were screened by one reviewer (RA). Any uncertainty of a manuscript was resolved by a second reviewer (MF).
Data extraction
One author (RA) extracted data using Microsoft Excel which was checked by a second author (MF). Any disagreements were resolved via consensus with a third party (CR). Extracted data included study design, participant demographics, intervention details and data for all outcomes.
Results
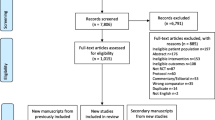
Seven hundred and seventy-eight records were retrieved from database searches, of which 15 records were duplicates. A further 649 were eliminated following a screening of titles and abstracts. After the full-text screening of 186 articles, 28 manuscripts were found to be eligible for inclusion in this review (Fig. 1) with an increase in the volume of papers published over the last three decades (Fig. 2).
Characteristics of studies
The 28 studies included comprised 15,946 participants, with sample sizes ranging from 11 to 7328 per study. Summary details of the included studies and populations are presented in Table 1.
The majority of studies (21/28) were performed in North America. Eleven studies (12/28) were conducted at a single site and another 11/28 recruited patients from multiple sites with the remaining 5/28 not stating the number of recruiting sites. The trial enrolment duration varied from 1 day to 14 years with 3/28 studies stating a range of lengths depending on the patient and 6/28 studies not stating the trial duration.
Narrative synthesis
All studies included reported the ethnicity of participants. Four studies 4/28 (14.3%; [28, 34, 44, 47]) only reported including Caucasian individuals and one study 1/28 (3.6%; [46]) reported only including African American patients. The remaining studies 23/28 (82.1%; [11, 25,26,27, 29,30,31,32,33, 35,36,37,38,39,40,41,42,43, 45]) all recruited patients from multiple ethnicities. No studies included a statement regarding inclusivity as part of the published manuscripts.
Fifteen studies 15/28 (53.6%; [11, 25, 26, 29,30,31, 33, 38,39,40, 42, 43, 45, 47, 50]) adopted a randomised control trial design, four 4/28 (14.3%; [36, 41, 46, 51]) cross-sectional, two 2/28 (7.1%; [31, 49]) cohort, two prospective 2/28 (7.1%; [44, 48]), two feasibility 2/28 (7.1%; [27, 28]), laboratory analysis 1/28 (3.6%; [34]), secondary analysis 1/28 (3.6%; [35]) and case–control study 1/28 (3.6%; [37]). Ten studies 10/28 (35.7%; [25, 28, 32, 33, 35, 38, 43, 44, 47, 48]) only recruited patients on androgen deprivation therapy (ADT), nine studies 9/28 (32.1%; [29,30,31, 34, 37, 41, 46, 49, 50]) involved patients on any form of treatment and six studies 6/28 (21.4%; [11, 26, 40, 42, 45, 51]) recruited those who had undergone radical prostatectomy. One study 1/28 (3.6%; [27]) recruited those receiving radiotherapy only, one study 1/28 (3.6%; [39]) recruited either radical prostatectomy or radiotherapy and a single study 1/28 (3.6%; [36]) involved either ADT, radical prostatectomy or radiotherapy patients.
The exercise elements of the studies varied, and individual study exercise details are presented in Table 2. Seven studies 7/28 (25%; [26, 28, 30, 43,44,45, 49]) involved home-based or unsupervised exercise. Six studies 6/28 (21.4%; [27, 29, 34, 40, 42, 50]) reported exercise sessions that were supervised by an exercise trainer or exercise physiologist and a further six studies 6/28 (21.4%; [11, 25, 32, 33, 38, 47]) had a mix of supervision over the trial period. Nine studies 9/28 (32.1%; [31, 35,36,37, 39, 41, 46, 48, 51]) did not explicitly state whether exercise was supervised or unsupervised. Three studies 3/28 (10.7%; [11, 35, 50]) included resistance exercise interventions, two 2/28 (7.1%; [40, 42]) included aerobic exercise interventions and a further two studies 2/28 (7.1%; [27, 29]) included yoga or flexibility programmes. Eleven studies 11/28 (39.3%; [25, 26, 28, 32, 33, 36, 38, 43,44,45, 47]) investigated an intervention which used a mix of exercise modalities (i.e. aerobic, resistance and flexibility). Ten studies 10/28 (35.7%; [30, 31, 34, 37, 39, 41, 46, 48, 49, 51]) were physical activity-based and primarily involved activity tracking.
Risk of bias
Risk of bias was assessed on all randomised studies and conducted by one author (RA). The Cochrane Risk of Bias tool [52] was used with risk of bias on the study level classified as ‘low’, ‘unclear’ or ‘high’ risk [53]. Table 3 shows a summary of the risk of bias for each of the included studies.
Discussion
Summary of findings
This review highlights the lack of reporting of patient ethnicity in PCa clinical trials involving exercise. Only 28 manuscripts reported ethnicity and none of the studies included a statement regarding strategies for ensuring inclusion or representative sampling. For example, studies may want to consider who the under-served groups are within the delivery area and barriers they face, plan for digital exclusion, recruit a sample who represents those who live with the specific condition, use language carefully or involve those under-served in the planning phase [54]. In the papers included in this review, it is evident that there is inconsistency in how ethnicity is reported making the results of the studies difficult to apply to the general PCa population. Accordingly, there is a greater need for those developing and running clinical trials in PCa and subsequently academic research outputs to adopt standardised terminology when it comes to describing and reporting the race and ethnicity of participants in exercise research, for example using those listed on countries official websites [55, 56]. To the authors’ knowledge, this is the first systematic review investigating ethnicity reporting in PCa and exercise trials and it therefore acts as a baseline for future practice.
Only one pilot trial has been included in this review that specifically recruited black men and this was in an African American community population. This mixed-methods study explored the quality of life, dietary and physical activity habits of African American PCa survivors [46]. The findings suggest that exercise interventions involving supervised strength training that are group-based; increase knowledge, skills-building and social support; address financial challenges and are easily accessed; these exercise interventions will help address some of the barriers in this underserved population [46]. Recognising that black men are at an increased risk of PCa, there is a clear need to design trials to fulfil the needs of black men, or at the very least further investigate qualitatively their views on exercise interventions and barriers. A study in 2017 explored the acceptability, barriers and facilitators to lifestyle interventions in African Caribbean PCa survivors and found that a PCa diagnosis, alongside ageing, heightened men’s awareness of their health [57]. They concluded that lifestyle interventions which enhance men’s independence and are framed as helping to regain fitness and aid post-treatment recovery are appealing and acceptable to African Caribbean PCa survivors [57].
Some of the barriers to research participation have been explored in other clinical populations and include a lack of childcare, mistrust, financial constraints, relatives’ influence and beliefs, lack of communication and cultural awareness between research staff and patients [58, 59]. The under-representation of ethnic minority groups in clinical trials affects the generalisability of study findings and ultimately contributes to exacerbating bias and inequities in access to healthcare if public health policies based on such evidence are implemented. It is possible that different ethnic groups respond in distinct ways to an intervention due to variations in physiology and/or disease state. Therefore, by studying the effects of an intervention in multiple ethnic groups, we can be sure that the outcomes are applicable to all.
Strengths and limitations
This systematic review has been conducted rigorously with regard to methodology and in line with the PRISMA guidelines. However, the main findings of this systematic review need to be considered in the context of some key limitations. For example, it is difficult to ascertain reasons for low recruitment numbers and, even when ethnicity was reported, recruitment strategy was not acknowledged in the manuscripts. Additionally, we must acknowledge that the lack of diversity may be due to the single centre studies being conducted in predominantly Caucasian areas, however, it is important that this is considered in their limitations section. More work is needed therefore to understand the barriers and facilitators of different ethnic groups to exercise research. Furthermore, recruitment strategies to ensure an inclusive sample need to be employed alongside reporting of participant ethnicities needs to be improved,
Implications for research and practice
The findings from this systematic review demonstrate that whilst there are many studies into the benefits of exercise within PCa patients, there are clear disparities between studies on the reporting of participants’ ethnicities and overall low numbers of ethnic minority men included. This systematic review suggests that representation is achieved in a few trials. Work needs to be performed to understand why representation is lacking in PCa exercise trials in the UK and action is needed to address this. Future studies may want to explore the barriers patients from different ethnic groups face when taking part in clinical trials and any potential bias within the recruitment process. Studies should include defined strategies to recruit a representative study sample and report this within the methods section of the manuscript in accordance with NIHR INCLUDE [54] to ensure the results are applicable and representative of the patient group. Additionally, authors should clearly report the ethnicity of participants within the demographic information of manuscripts to allow the reader to properly interpret the results in the context of the patients included.
Conclusion
This systematic review highlights that there is high heterogeneity in the reporting of participants’ ethnicity within PCa trials involving exercise. Additionally, it has also demonstrated that there are low numbers of ethnic minority men included in PCa and exercise studies in the UK and a lack of reporting of ethnicities in published papers. As such, further work is required to understand why representation is lacking within PCa exercise trials in the UK and strategies are needed to achieve representation. Future studies should seek to explore the barriers PCa patients from different ethnic groups face when taking part in clinical trials in the UK.
Data availability
No datasets were generated or analysed during the current study.
References
Cancer Research UK. Prostate cancer statistics. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer#heading-Zero. Accessed 17 July 2024
Wang L et al (2022) Prostate cancer incidence and mortality: global status and temporal trends in 89 countries from 2000 to 2019. Front Public Health 10:811044
Paterson C et al (2015) Identifying the unmet supportive care needs of men living with and beyond prostate cancer: a systematic review. Eur J Oncol Nurs 19(4):405–418
Paterson C et al (2022) The effects of multimodal prehabilitation interventions in men affected by prostate cancer on physical, clinical and patient reported outcome measures: a systematic review. Semin Oncol Nurs 38(5):151333
Aning JJ et al (2018) Detailed analysis of patient-reported lower urinary tract symptoms and effect on quality of life after robotic radical prostatectomy. Urol Oncol 36(8):364.e15-364.e22
Campbell KL et al (2019) Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc 51(11):2375–2390
Lowder D et al (2022) Racial disparities in prostate cancer: a complex interplay between socioeconomic inequities and genomics. Cancer Lett 531:71–82
Lloyd T et al (2015) Lifetime risk of being diagnosed with, or dying from, prostate cancer by major ethnic group in England 2008–2010. BMC Med 13(1):171
Delon C et al (2022) Differences in cancer incidence by broad ethnic group in England, 2013–2017. Br J Cancer 126(12):1765–1773
Chornokur G et al (2011) Disparities at presentation, diagnosis, treatment, and survival in African American men, affected by prostate cancer. Prostate 71(9):985–997
Ashton RE et al (2021) Supported progressive resistance exercise training to counter the adverse side effects of robot-assisted radical prostatectomy: a randomised controlled trial. Support Care Cancer 29(8):4595–4605
Bourke L et al (2018) Exercise training as a novel primary treatment for localised prostate cancer: a multi-site randomised controlled phase II study. Sci Rep 8(1):8374
Banerjee S et al (2018) Vigorous intensity aerobic interval exercise in bladder cancer patients prior to radical cystectomy: a feasibility randomised controlled trial. Support Care Cancer 26(5):1515–1523
Mottet N, Cornford P, van den Bergh RCN, Briers E, Expert Patient Advocate, De Santis M, Gillessen S, Grummet J, Henry AM, van der Kwast TH, Lam TB, Mason MD, O'Hanlon S, Oprea-Lager De, Ploussard G, van der Poel HG, Rouviere O, Schoots IG, Tilki D, Wiegel T (2022) EAU guidelines on prostate cancer. Available from: https://uroweb.org/guidelines/prostate-cancer/chapter/introduction. Accessed 12 Feb 2024
NICE (2014) Physical activity: exercise referral schemes - public health guideline [PH54]. Available from: https://www.nice.org.uk/guidance/ph54. Accessed 12 Feb 2024
Bourke L et al (2016) Exercise for men with prostate cancer: a systematic review and meta-analysis. Eur Urol 69(4):693–703
Andersen MF, J Midtgaard, ED Bjerre (2022) Do patients with prostate cancer benefit from exercise interventions? A systematic review and meta-analysis. Int J Environ Res Public Health 19(2): 972
Hart NH, Galvão DA, Newton RU (2017) Exercise medicine for advanced prostate cancer. Curr Opin Support Palliat Care 11(3):247–257
Hasenoehrl T et al (2015) The effects of resistance exercise on physical performance and health-related quality of life in prostate cancer patients: a systematic review. Support Care Cancer 23(8):2479–2497
Keilani M et al (2017) Effects of resistance exercise in prostate cancer patients: a meta-analysis. Support Care Cancer 25(9):2953–2968
Hvid T et al (2016) Effect of a 2-year home-based endurance training intervention on physiological function and PSA doubling time in prostate cancer patients. Cancer Causes Control 27(2):165–174
Rencsok EM et al (2020) Diversity of enrollment in prostate cancer clinical trials: current status and future directions. Cancer Epidemiol Biomarkers Prev 29(7):1374–1380
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan — a web and mobile app for systematic reviews. Syst Rev 5:210
Alibhai SMH et al (2019) A phase II randomized controlled trial of three exercise delivery methods in men with prostate cancer on androgen deprivation therapy. BMC Cancer 19(1):2
Au D et al (2019) Prehabilitation and acute postoperative physical activity in patients undergoing radical prostatectomy: a secondary analysis from an RCT. Sports Med Open 5(1):18
Ben-Josef AM et al (2016) Yoga intervention for patients with prostate cancer undergoing external beam radiation therapy: a pilot feasibility study. Integr Cancer Ther 15(3):272–278
Brown M, Murphy MH, McAneney H, McBride K, Crawford F, Cole A, O'Sullivan JM, Jain S, Prue G (2023) Feasibility of home‑based exercise training during adjuvant treatment for metastatic castrate‑resistant prostate cancer patients treated with an androgen receptor pathway inhibitor (EXACT). Supportive Care Cancer 31(7):442
Campo RA et al (2014) Levels of fatigue and distress in senior prostate cancer survivors enrolled in a 12-week randomized controlled trial of Qigong. J Cancer Surviv 8(1):60–69
Chan JM et al (2020) Feasibility and acceptability of a remotely delivered, web-based behavioral intervention for men with prostate cancer: four-arm randomized controlled pilot trial. J Med Internet Res 22(12):e19238
Dai JY et al (2019) Vigorous physical activity is associated with lower risk of metastatic-lethal progression in prostate cancer and hypomethylation in the CRACR2A gene. Cancer Epidemiol Biomarkers Prev 28(2):258–264
Dalla Via J et al (2021) Musculoskeletal responses to exercise plus nutrition in men with prostate cancer on androgen deprivation: a 12-month RCT. Med Sci Sports Exerc 53(10):2054–2065
Dawson JK et al (2018) Impact of resistance training on body composition and metabolic syndrome variables during androgen deprivation therapy for prostate cancer: a pilot randomized controlled trial. BMC Cancer 18(1):368
Evans HE et al (2021) Usability, acceptability, and safety analysis of a computer-tailored web-based exercise intervention (ExerciseGuide) for individuals with metastatic prostate cancer: multi-methods laboratory-based study. JMIR Cancer 7(3):e28370
Fairman CM et al (2018) Monitoring resistance exercise intensity using ratings of perceived exertion in previously untrained patients with prostate cancer undergoing androgen deprivation therapy. J Strength Cond Res 32(5):1360–1365
Faithfull S et al (2021) Obesity and low levels of physical activity impact on cardiopulmonary fitness in older men after treatment for prostate cancer. Eur J Cancer Care (Engl) 30(6):e13476
Friedenreich CM et al (2016) Physical activity and survival after prostate cancer. Eur Urol 70(4):576–585
Gilbert SE et al (2016) Effects of a lifestyle intervention on endothelial function in men on long-term androgen deprivation therapy for prostate cancer. Br J Cancer 114(4):401–408
Hébert JR et al (2012) A diet, physical activity, and stress reduction intervention in men with rising prostate-specific antigen after treatment for prostate cancer. Cancer Epidemiol 36(2):e128–e136
Jones LW et al (2014) Effects of nonlinear aerobic training on erectile dysfunction and cardiovascular function following radical prostatectomy for clinically localized prostate cancer. Eur Urol 65(5):852–855
Langelier DM et al (2018) Perceptions of masculinity and body image in men with prostate cancer: the role of exercise. Support Care Cancer 26(10):3379–3388
Nilsen TS et al (2018) Novel methods for reporting of exercise dose and adherence: an exploratory analysis. Med Sci Sports Exerc 50(6):1134–1141
Sajid S et al (2016) Novel physical activity interventions for older patients with prostate cancer on hormone therapy: a pilot randomized study. J Geriatr Oncol 7(2):71–80
Santa Mina D et al (2013) Exercise effects on adipokines and the IGF axis in men with prostate cancer treated with androgen deprivation: a randomized study. Can Urol Assoc J 7(11–12):E692–E698
Santa Mina D et al (2018) Prehabilitation for radical prostatectomy: a multicentre randomized controlled trial. Surg Oncol 27(2):289–298
Stolley MR et al (2020) Exploring health behaviors, quality of life, and support needs in African-American prostate cancer survivors: a pilot study to support future interventions. Support Care Cancer 28(7):3135–3143
Taaffe DR et al (2017) Effects of different exercise modalities on fatigue in prostate cancer patients undergoing androgen deprivation therapy: a year-long randomised controlled trial. Eur Urol 72(2):293–299
Trinh L et al (2018) RiseTx: testing the feasibility of a web application for reducing sedentary behavior among prostate cancer survivors receiving androgen deprivation therapy. Int J Behav Nutr Phys Act 15(1):49
Wang Y et al (2017) Recreational physical activity in relation to prostate cancer-specific mortality among men with nonmetastatic prostate cancer. Eur Urol 72(6):931–939
Winters-Stone KM et al (2016) Benefits of partnered strength training for prostate cancer survivors and spouses: results from a randomized controlled trial of the Exercising Together project. J Cancer Surviv 10(4):633–644
Wolin KY et al (2010) Risk of urinary incontinence following prostatectomy: the role of physical activity and obesity. J Urol 183(2):629–633
Higgins JPT et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Julian PT Higgins, JT Jacqueline Chandler, Miranda Cumpston, Tianjing Li, Matthew J Page, Vivian A Welch (2019) Cochrane Handbook for systematic reviews of interventions, 2nd ed, Wiley-Blackwell
NIHR (2020) Improving inclusion of under-served groups in clinical research: guidance from the NIHR-INCLUDE project. UK: NIHR. 14th March 2023]. Available from: www.nihr.ac.uk/documents/improving-inclusion-of-under-served-groups-in-clinical-research-guidance-from-include-project/25435. Accessed 12 Feb 2024
Jenson E, Jones N, Orozco K, Medina L, Peery M, Bolender B, Battle K (2022) Measuring racial and ethnic diversity for the 2020 census. Available from: https://www.census.gov/newsroom/blogs/random-samplings/2021/08/measuring-racial-ethnic-diversity-2020-census.html. Accessed 23 July 2024
UK Government (N.D) List of ethnic groups. Available from: https://www.ethnicity-facts-figures.service.gov.uk/style-guide/ethnic-groups/. Accessed 23 July 2024
Er V et al (2017) Barriers and facilitators to healthy lifestyle and acceptability of a dietary and physical activity intervention among African Caribbean prostate cancer survivors in the UK: a qualitative study. BMJ Open 7(10):e017217
Waheed W et al (2015) Overcoming barriers to recruiting ethnic minorities to mental health research: a typology of recruitment strategies. BMC Psychiatry 15(1):101
Duma N et al (2018) Representation of minorities and women in oncology clinical trials: review of the past 14 years. J Oncol Pract 14(1):e1–e10
Funding
This project was partially supported by the University of Derby Knowledge Exchange Impact Accelerator Fund.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. RA conducted the database searches with data extraction supported by MF. All authors contributed to the writing of the manuscripts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ashton, R.E., Faghy, M.A., Roscoe, C.M.P. et al. Inclusivity in prostate cancer and exercise research: a systematic review. Support Care Cancer 32, 616 (2024). https://doi.org/10.1007/s00520-024-08793-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08793-9