Abstract
Purpose
To evaluate the prevalence of dysphagia in survivors of head and neck cancer (sHNC) and to identify the predictors contributing to the development of dysphagia.
Methods
We enrolled 62 sHNC in a cross-sectional study to check the prevalence of dysphagia in sHNC and to evaluate which factors were influencing the presence of this side effect. Besides dysphagia, sociodemographic and clinical characteristics, oral symptoms, maximal mouth opening (MMO), sleep quality and physical condition were evaluated, and a linear regression analysis was performed to verify which of these outcomes impact dysphagia.
Results
Among all the sHNC, 85.5% presented dysphagia. The linear regression analysis confirmed that 44.9% of the variance in dysphagia was determined by coughing, MMO and sleep quality, being MMO the most powerful predictor, followed by coughing and sleep quality.
Conclusion
Dysphagia affected the great majority of sHNC. Moreover, symptoms as coughing, reduced MMO and sleep disorders may act as predictors contributing to the development of dysphagia. Our results emphasize the importance of an early and proper identification of the symptoms as well as an adequate treatment strategy to address the cluster of symptoms that sHNC undergo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dysphagia, defined as limited swallowing function, affects more than half (54.9%) of survivors of head and neck cancer (sHNC) [1]. Beyond the physical limitations of swallowing, dysphagia poses a substantial risk of complications that can significantly affect the overall health and well-being of sHNC. The key challenges associated with dysphagia include medication nonadherence [2], malnutrition [3], dehydration [2], and an increased susceptibility to pneumonia [4]. Dealing with dysphagia and its associated complications can also evoke feelings of depression and anxiety, while eating and communication disorders may lead to social isolation [5]. Thus, the impact of dysphagia on sHNC extends far beyond the immediate physical consequences, affecting their overall quality of life (QoL).
Consequently, dysphagia should be considered a ‘vital sign’ beyond swallowing dysfunction. Head and neck cancer (HNC) guidelines recommend the use of multidisciplinary teams to monitor and optimize dysphagia outcomes and intervene when necessary [2]. Despite this recommendation, health care professionals lack the tools to identify patients who are at risk of suffering dysphagia due to a lack of understanding of which potential outcomes may influence this troubling side effect of cancer and its treatment.
On the one hand, relationships among trismus (i.e., impaired mouth opening), QoL, and dysphagia in large populations of sHNC have been previously shown [6]. On the other hand, Petersson and colleagues [7] investigated whether radiation-derived dysphagia could be predicted by tumour and patient characteristics such as feeding tube use, weight factors, trismus, and saliva secretion in sHNC. Furthermore, Ortiz-Comino [8] and colleagues found that pain perceived in the cervical and shoulder regions, perception of physical fitness, and fatigue were predictors of QoL among sHNC. Finally, Pezdirec and colleagues [9] found a significant relationship between dysphagia and some of the treatment-derived side effects (impaired mouth opening, sticky saliva, and persistent cough, among others), radiotherapy (RT), and symptoms of gastroesophageal reflux, but after multiple regression modelling, only persistent cough remained significant. However, the interplay between dysphagia and outcomes related to oral symptoms and mouth opening, sleep quality, physical condition and treatment modality has not yet been characterized in this population.
Sleep disturbances have been found to be prevalent in sHNC, and these can have a significant impact on swallowing function [10]. Moreover, the relationship between sleep disorders and dysphagia resulting from HNC becomes even more significant when considering the marked sequelae of xerostomia and sticky saliva following treatment for oropharyngeal cancers [11]. Disrupted sleep patterns and poor sleep quality can lead to fatigue, decreased muscle coordination, and weakened muscle tone in the oropharyngeal area, all of which can exacerbate swallowing difficulties [12]. Additionally, sleep disorders may contribute to inflammation and tissue damage in the upper aerodigestive tract, further compromising the swallowing process [13]. Therefore, addressing and managing sleep disorders in sHNC may play a crucial role in improving dysphagia outcomes and overall QoL.
Likewise, patients with dysphagia may not be able to swallow certain foods or drinks, which can lead to a restricted diet; the resulting poor nutritional status may worsen when the swallowing-related muscles are affected by sarcopenia, aggravating dysphagia. Furthermore, the loss of skeletal muscle mass (SMM) and physical function that accompany sarcopenia leads to a vicious cycle, further worsening the swallowing ability of sHNC [14].
Prior research involving sHNC has shown a direct relationship between a more complex treatment (higher radiation doses or concurrent chemotherapy-radiotherapy) and greater dysphagia [15]; In contrast, Jia and colleagues did not find a significant relationship between dysphagia and treatment modality (surgery and/or adjuvant treatment) [6].
To date, no studies have evaluated the complex relationships among dysphagia, oral symptoms, maximal mouth opening (MMO), sleep quality, and physical condition. The purpose of this study was to evaluate the prevalence of dysphagia in sHNC and to identify the predictors contributing to the development of dysphagia by analysing whether a 10-question symptom-specific measure of dysphagia symptoms [(Eating Assesment Tool (EAT-10)] correlated with a worsening in oral symptoms, MMO, or sleep quality; an increased risk of physical deconditioning; and a more complex treatment modality in sHNC. The results of this study may emphasize the importance of recognizing predictors of dysphagia and reinforce the importance of early and accurate identification and treatment in this population.
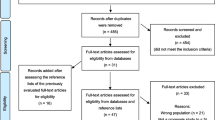
Methods
Study design and setting
This cross-sectional study followed the STROBE statement checklist recommendations [16] (Online resource) and was approved by the Biomedical Investigation Ethics Committee, Granada, Spain (0045-N-16 and 1552-N-18) and performed according to the Declaration of Helsinki. Participants were recruited between 2018 and 2022 at the Virgen de las Nieves University Hospital and San Cecilio University Hospital (Granada, Spain). The assessments were carried out at the facilities of the research group Cuídate (Physical Therapy Department, University of Granada, Spain).
Participants
sHNC were enrolled if they met the following inclusion criteria: diagnosis of a cancer located in the upper aerodigestive tract, 18 years of age or older, oncological treatment completed, in complete remission, and Spanish speaking; the exclusion criteria were cognitive or social characteristics that would hinder understanding and completing the assessment, presence of metastases, and refusal to participate. All participants signed an informed consent statement before participation.
Measures
Once sHNC had been recruited, all measurements were obtained by the research staff in a single visit.
Sociodemographic and clinical variables
Sociodemographic characteristics were obtained by standard questions and included age, gender, alcohol and tobacco consumption, civil status and education level. Clinical variables were collected from the medical records and included primary tumour location, tumour stage at diagnosis, time since diagnosis and treatment modality.
Dysphagia
The perception of swallowing dysfunction was measured with the EAT-10. This is a validated symptom-specific self-report questionnaire consisting of 10 items scored on a 0–4 scale (0 = no impairment; 4 = a severe problem). The total score ranges from 0 to 40, with ≥ 3 points considered indicative of dysphagia (Cronbach’s alpha = 0.96) [17].
Oral symptoms: coughing and sticky saliva
Coughing and sticky saliva were evaluated with the European Organization for Research and Treatment of Cancer Quality of Life specific module for head and neck (EORTC QLQ-H&N35) [18]. We used these two symptom items related to coughing and sticky saliva perception scored on a 4-point Likert scale from 1 (not at all) to 4 (very much); a higher score indicates a higher level of symptomatology. This questionnaire has been previously validated in the HNC population (Cronbach’s alpha > 0.70) [19].
These two items were chosen because they were relevant to the aim of this study according to previous studies that have highlighted unmet needs in the HNC population related to QoL after oncological treatment [11].
Maximal mouth opening
MMO was measured in millimetres (mm) using a sliding calliper. sHNC who used a dental prosthesis were instructed to wear their prosthesis during the measurements. Patients were asked to stand and to open their mouth as wide as possible, and then the distance between the upper and lower central incisors (of their own dentition or prosthesis) was measured. An MMO of ≤ 35 mm is used as the cut-off point for trismus in the HNC population [20] and has good reliability (intraclass correlation coefficient [ICC] = 0.95–0.96) [21].
Sleep quality
Sleep quality was evaluated using the self-reported Pittsburgh Sleep Quality Index (PSQI). The PSQI global score ranges from 0 to 21 and discriminates good sleepers from poor sleepers, with a higher score indicating worse sleep quality. A global score ≥ 5 points indicates poor sleep quality and has shown consistency and validity in cancer research (Cronbach’s alpha = 0.77–0.81) [22].
Physical condition: physical functioning and skeletal muscle mass
Physical functioning was evaluated with a subscale of the European Organization for Research and Treatment of Cancer Quality of Life Core-30 version 3.0 (EORTC QLQ-C30). This subscale is composed of five items related to difficulties in daily activities. The items are scored on a 4-point Likert scale from 1 (not at all) to 4 (very much), with higher scores indicating higher levels of physical functioning. This questionnaire has been validated in the HNC population (Cronbach’s alpha > 0.70) [19].
We hypothesized that this physical functioning domain should be part of the comprehensive assessment, as HNC patients present QoL impairment with regard to physical limitations [11].
A bioelectrical impedance analysis (BIA) was performed using InBody 720 (InBody Corp. Seoul, Korea) to evaluate SMM (kg). This machine uses a tetrapolar eight-point tactile electrode system, where participants must stand barefoot on the feet electrodes and with their hands gripping the hand electrodes, with the arms abducted along the trunk. In addition, they were instructed to not alter their normal activity and to not eat just before the test. The BIA method is a valid tool for estimating SMM [23].
Statistical analyses
Continuous variables are presented as the mean ± standard deviation (95% confidence interval), and categorical data are represented as frequencies and percentages. The Kolmogorov‒Smirnov test was performed to assess whether the variables were normally distributed.
To minimize the potential bias arising from missing data, multiple imputation was employed for missing data. We assumed that the data were missing at random conditional on measured characteristics, and excluding participants with any missing data can introduce bias and decrease statistical power. A total of 25 different imputed databases were generated, which included multiple estimates for the missing data. The pooled data were subsequently utilized for analysis [24]. Then, a bivariate correlation analysis was performed to examine the correlations among dysphagia, coughing, sticky saliva, MMO, sleep quality, physical functioning, SMM and treatment modality using the Pearson or Spearman correlation coefficient depending on the normality of the variables. The correlation coefficients were categorized according to the Cohen criteria (> 0.5, large; 0.5–0.3, moderate; < 0.3–0.1, small; and < 0.1, insubstantial) [25]. Subsequently, a partial correlation analysis was performed adjusting for three sociodemographic and clinical covariates one by one (age, tumour stage and time since diagnosis), and semipartial correlations were also obtained to examine the specific contribution of each independent variable.
The variables significantly correlated with dysphagia and with a correlation coefficient ≤ 0.7 between each other were entered in a linear regression analysis (stepwise method) to determine the association between potential predictors (independent variables) and dysphagia (dependent variable). Multicollinearity between independent variables was assessed using the variance inflation factor (VIF) and tolerance; if the VIF and tolerance were > 10 and < 0.2, respectively, multicollinearity existed [26]. Furthermore, the regression model was adjusted for age, tumour stage and time since diagnosis. Finally, based on clinical and statistical criteria, the mediation effect of sticky saliva, MMO, and sleep quality on the association between coughing, MMO, sleep quality, and treatment modality with dysphagia was assessed with the PROCESS macro for IBM SPSS Statistics. Statistical significance was defined as p < 0.05. All statistical analyses were performed using the software IBM SPSS Statistics version 28.0 (IBM, Armonk, NY), and the graph was made using RStudio (R 4.3.1 software).
Results
Study population
A total of 62 sHNC with a mean age of 60.69 ± 11.08 years participated in the study, of whom 69.4% (n = 43) were men. The most common primary tumour location was the oropharynx and oral cavity (37.1%, n = 23), and the most common treatment modality was a combination of RT, surgery and chemotherapy (41.9%, n = 26), followed by RT plus chemotherapy (29%, n = 18) and RT plus surgery (24.2%, n = 15). Among all the sHNC, 85.5% (n = 53) presented dysphagia (EAT-10 ≥ 3). Table 1 details all the sociodemographic and clinical characteristics of the sample.
Association between dysphagia and oral symptoms, MMO, sleep quality, physical condition, and treatment modality
Figure 1 shows that a higher level of dysphagia was correlated with worse coughing (r = 0.352, p = 0.005), worse sticky saliva (r = 0.446, p < 0.001), worse sleep quality (r = 0.315, p = 0.013), worse physical functioning (r = -0.381, p = 0.002) and more complex treatment modality (r = 0.308, p = 0.015). Moreover, a higher level of dysphagia was correlated with a lower MMO (r = -0.519, p < 0.001). No significant correlation between dysphagia and SMM was noted (r = -0.239, p = 0.066).
Correlation matrix between dysphagia, coughing, sticky saliva, maximal mouth opening (MMO), sleep quality, physical functioning, skeletal muscle mass (SMM) and treatment modality. The blue and red colour gradient represents the strength of the correlation coefficient (Pearson for all variables except Spearman for treatment variable). *p < 0.05; **p < 0.01
Partial and semipartial correlations
After adjusting for age, higher dysphagia correlated with lower SMM (r = -0.266, p = 0.043). After adjusting for tumour stage, higher dysphagia correlated with lower SMM (r = -0.289; p = 0.036), and treatment modality lost its significant correlation with dysphagia (r = 0.258, p = 0.062). The statistically significant associations with all other independent variables remained the same after adjusting for both age and tumour stage. All the associations persisted after adjustment for time since diagnosis.
Semipartial correlations for each predictor variable showed that MMO explained 27.04% of dysphagia variance (r = -0.520), coughing explained 11.08% (r = 0.333) and sleep quality explained 7.95% (r = 0.282).
Multiple regression model
Although coughing, sticky saliva, MMO, sleep quality, physical functioning and treatment modality were significantly correlated with dysphagia (p < 0.05), linear regression analysis confirmed that 44.9% of the variance in dysphagia was determined by coughing, MMO and sleep quality (adjusted r2 = 44.9%, F = 17.284, p < 0.001). MMO was the most powerful predictor for dysphagia, followed by coughing and sleep quality. For every unit decrease in MMO measurement, the expected value of EAT-10 increased by 0.520 units; for every unit increase in coughing (EORTC QLQ-H&N35), the expected value of EAT-10 increased by 0.334 units; and for every unit increase in PSQI global score, the expected value of EAT-10 increased by 0.283 units (Table 2).
The multicollinearity analysis in the regression model showed no correlation among MMO (VIF = 1.000, tolerance = 1.000) coughing (VIF = 1.008, tolerance = 0.992) and sleep quality (VIF = 1.008, tolerance = 0.993).
The regression model was not modified after adjusting for age, tumour stage and time since diagnosis.
Figure 2 represents the mediating effects of MMO, sticky saliva and sleep quality on the association between treatment modality, MMO, coughing and sleep quality, as appropriate. As shown, the influence of treatment modality on dysphagia was partially explained through a reduction in MMO (indirect effect ranging from 0.56 to 3.73; p < 0.05) (Fig. 2_a). A similar significant indirect effect of sticky saliva was found in the relationship between MMO and dysphagia (-0.22 to -0.02; p < 0.05) (Fig. 2_b) and between sleep quality and dysphagia (0.09 to 0.73; p < 0.05) (Fig. 2_e).
Discussion
The goal of this study was to examine potential predictors of dysphagia in sHNC and the associations between these outcomes. According to the Cohen criteria, a substantial association between dysphagia and MMO was found, whereas moderate associations were found between dysphagia and coughing, sticky saliva, sleep quality, physical functioning, and treatment modality; only three of these outcomes (MMO, coughing and sleep quality) could partly explain this swallowing dysfunction. Dysphagia is one of the main RT-induced side effects, among other acute and chronic side effects of oncological treatment due to the traumatizing impact on the tissues surrounding the upper aerodigestive tract [1], especially when surgery, RT, and chemotherapy coexist [27].
Our study population was 60.69 years old on average and had been diagnosed with cancer for a mean of 32.6 months, and the great majority (85.5%; 53 participants) presented dysphagia as detected by the EAT-10; results that concord with a previous cross-sectional study [28]. Moreover, our study population presented oral symptoms such as coughing and sticky saliva (items extracted from the EORTC QLQ-H&N35 questionnaire). These symptoms, added to the sensory deterioration due to oncological treatment may induce an inefficient cough reflex and thus increase the risk of dysphagia [29]. Consistent with our results, Nguyen and colleagues [30] found that only 40% of patients with HNC with dysphagia have an effective cough response to aspirated material, and, as described by Beetz and colleagues, [31] 43% of patients with HNC reported moderate to severe sticky saliva at 6 months after treatment with primary chemoradiotherapy. Another symptom presented by our population was trismus, a side effect commonly suffered by sHNC [32]; poor sleep quality occurs in approximately one-third of patients with HNC after treatment [33] and continues in the long term [34]. Finally, the studied population also presented low levels of physical functioning (evaluated through the related subscale from the EORTC QLQ-C30) and poor SMM [35], which is considered common in survivors with cancer and specifically in sHNC [36]. Decreasing weight and SMM are usually linked to malnutrition among sHNC, even in patients who are able to maintain a normal weight, which could be related to severe dysphagia [7]. Moreover, those who perform more leisure-time exercise have a lower risk of dysphagia [37], as leisure activities are usually associated with higher tongue pressure, suggesting that interacting with others may be one way of maintaining oral function [38].
The association between dysphagia and MMO was the strongest in our study. Impaired MMO is usually associated with radiation fibrosis syndrome [39]. In the HNC population, the prevalence of trismus ranges from 6 to 79% [40]. This symptom is one of the most common symptoms presented in sHNC, affecting up to 40% of patients after oncological treatment [40]. As mouth opening is crucial to the oral phase of swallowing, its decrease could indeed induce dysphagia [27]; in addition, limited MMO may cause difficulties in proper food mastication, which is linked to aspiration problems due to compromised airway clearance with poor bolus organization [41].
To date, no studies have evaluated the association between dysphagia and sleep quality, but if symptoms such as coughing and sticky saliva occur at night, it could be possible that sleep quality may also deteriorate. Considering the mediation effect of sticky saliva on the association between sleep quality and dysphagia, it seems logical explore further the aforementioned mediation in poor sleepers (see Fig. 2_e).
Finally, SMM only correlated negatively with dysphagia when adjusting for either age or tumour stage in this study, a result concordant with previous studies that associate ageing processes with the loss of SMM or even sarcopenia [42]; similarly, a greater tumour stage is usually associated with more aggressive treatments that could worsen SMM, affecting the swallowing process. Although there is some disagreement on the effects of the treatment modality on the perception of dysphagia, our results demonstrate a moderate association between dysphagia and treatment modality, but the latter was not predictor contributing the development of dysphagia after our multiple regression modelling. This could be due to the true association between treatment modality with dysphagia is mediated significantly by MMO (see Fig. 2_a). We included this variable in our study because oncological treatment has been shown to induce secondary side effects over the cranio-cervical region [43], which could secondarily worsen the swallowing process. Finally, after adjusting for tumour stage, treatment modality did not correlate with dysphagia.
Moreover, our results revealed that MMO, coughing, and sleep disorders explains 44.9% of the variability of the overall problem, acting as predictors of dysphagia presented by sHNC, with MMO being the most powerful predictor in our model. All predictors found in this study were independently associated with dysphagia, as no collinearity was found between them when analysed.
As stated previously, MMO impairments are widely present in sHNC [40], and their decrease could directly be associated with dysphagia [27]. Similarly, cough could be related to hyposensitivity of the larynx, producing a microaspiration in the trachea after surgery/irradiation. On the other hand, gastroesophageal reflux is known to be associated with obstructive apnoea [44], and this fact could play an important role in the development of sleep disorders in our population [45]. To date, no studies have stated that sleep quality perception is a predictor of dysphagia in sHNC, but the loss of restful sleep could induce sHNC to have a higher perception of fatigue during the day [46], and this fact could increase the risk of perceiving dysphagia.
Identifying independent factors associated with dysphagia is crucial to guide health care professionals in the identification of patients at higher risk of dysphagia, so that interventions focused on these outcomes (i.e., MMO, coughing and sleep quality) may prevent their worsening and thus the risk of aspiration, as previously mentioned.
The study limitations are as follows. First, the heterogeneity of the tumour locations and the different stages of the disease and treatment modalities used in the studied population. It would be desirable to increase the sample size to conduct a subgroup analysis to determine the stability of the cluster in different tumour locations or treatment modalities. Moreover, due to the cross-sectional design, we did not perform a follow-up assessment of the patients, which would have been important to analyse changes in the outcomes evaluated at different time points. Longitudinal research with the inclusion of a follow-up registry will enhance the knowledge about dysphagia over the survivorship period. Finally, this study reports solely on patient-reported swallowing dysfunction instead of using the gold standard method for evaluating dysphagia (i.e., videofluoroscopy), which could have helped us to explore objectively how patients are impacted by their problems [1] and link it to subjective outcomes.
Despite the described limitations, our results provide evidence of a combination of symptoms that may be considered to better address the dysphagia perceived by sHNC with specific treatments developed by health care professionals. Due to the existence of multiple types of HNC and different matching treatments and/or supportive treatments (such as tracheal intubation), it is crucial to find specific management strategies that can more effectively regulate and control symptoms to improve sHNC’ QoL through the start-up of dysphagia prevention programs that would benefit patients and caregivers. This preliminary study may help researchers and clinicians to better understand the clusters of symptoms that occur during the survivorship phase in HNC.
Conclusion
Dysphagia affected the great majority (85.5%) of sHNC in the present study. Moreover, coughing, reduced MMO and sleep disorders may act as predictors contributing to the development of dysphagia. Our results emphasize the importance of an early and proper identification of the symptoms as well as an adequate treatment strategy to address the cluster of symptoms that sHNC undergo.
References
Zebralla V, Wichmann G, Pirlich M et al (2021) Dysphagia, voice problems, and pain in head and neck cancer patients. Eur Arch Oto-Rhino-Laryngology 278:3985–3994. https://doi.org/10.1007/s00405-020-06584-6
Kuhn MA, Gillespie MB, Ishman SL et al (2023) Expert Consensus Statement: Management of Dysphagia in Head and Neck Cancer Patients. Otolaryngol - Head Neck Surg (United States) 168:571–592. https://doi.org/10.1002/ohn.302
Simon SR, Pilz W, Hoebers FJP et al (2021) Malnutrition screening in head and neck cancer patients with oropharyngeal dysphagia. Clin Nutr ESPEN 44:348–355. https://doi.org/10.1016/j.clnesp.2021.05.019
Reddy PD, Yan F, Nguyen SA, Nathan CAO (2021) Factors Influencing the Development of Pneumonia in Patients With Head and Neck Cancer: A Meta-analysis. Otolaryngol - Head Neck Surg (United States) 164:234–243. https://doi.org/10.1177/0194599820938011
Eastburn K, Lyu L, Harrison C et al (2022) Association Between Patient-Reported Symptoms of Dysphagia and Psychological Distress in Head and Neck Cancer Survivors. Oncol Nurs Forum 49:81–89. https://doi.org/10.1188/22.ONF.81-89
Jia Z, Li J, Harrison C et al (2022) Association of Trismus With Quality of Life and Swallowing in Survivors of Head and Neck Cancer. Otolaryngol - Head Neck Surg (United States) 166:676–683. https://doi.org/10.1177/01945998211026848
Petersson K, Finizia C, Tuomi L (2021) Predictors of severe dysphagia following radiotherapy for head and neck cancer. Laryngoscope Investig Otolaryngol 6:1395–1405. https://doi.org/10.1002/lio2.676
Ortiz-Comino L, Galiano-Castillo N, Postigo-Martín EP et al (2022) Factors Influencing Quality of Life in Survivors of Head and Neck Cancer: A Preliminary Study. Semin Oncol Nurs 38:151256. https://doi.org/10.1016/j.soncn.2022.151256
Pezdirec M, Strojan P, Boltezar IH (2019) Swallowing disorders after treatment for head and neck cancer. Radiol Oncol 53:225–230. https://doi.org/10.2478/raon-2019-0028
Muñoz-Vigueras N, Obeso-Benítez P, Jerviz-Guía V et al (2023) Smartphone-based follow-up of upper airway symptoms in head and neck cancer survivors one year after radiation therapy. Int J Lang Commun Disord 58:270–278. https://doi.org/10.1111/1460-6984.12782
Patton LL, Helgeson ES, Brennan MT et al (2023) Oral health-related quality of life after radiation therapy for head and neck cancer: the OraRad study. Support Care Cancer 31:1–14. https://doi.org/10.1007/s00520-023-07750-2
Pizzorni N, Radovanovic D, Pecis M et al (2021) Dysphagia symptoms in obstructive sleep apnea: prevalence and clinical correlates. Respir Res 22:1–10. https://doi.org/10.1186/s12931-021-01702-2
Irwin M, Olmstead R, Carrol JE (2016) Sleep Disturbance, Sleep Duration, and Inflammation. Biol Psychiatry 80:40–52. https://doi.org/10.1016/j.biopsych.2015.05.014.Sleep
Karavolia E, van Rijn-Dekker MI, Van den Bosch L et al (2022) Impact of sarcopenia on acute radiation-induced toxicity in head and neck cancer patients. Radiother Oncol 170:122–128. https://doi.org/10.1016/j.radonc.2022.03.009
Alexidis P, Bangeas P, Efthymiadis K et al (2022) Investigating factors associated to dysphagia and need for percutaneous endoscopic gastrostomy in patients with head and neck cancer receiving radiation therapy. J Cancer 13:1523–1529. https://doi.org/10.7150/jca.69130
Vandenbroucke JP, von Elm E, Altman DG et al (2014) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int J Surg 12:1500–1524. https://doi.org/10.1016/j.ijsu.2014.07.014
Belafsky PC, Pryor JC, Allen J et al (2014) Validity and Reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol 117:919–924. https://doi.org/10.1177/000348940811701210
Singer S, Arraras JI, Chie WC et al (2013) Performance of the EORTC questionnaire for the assessment of quality of life in head and neck cancer patients EORTC QLQ-H&N35: A methodological review. Qual Life Res 22:1927–1941. https://doi.org/10.1007/s11136-012-0325-1
Singer S, Wollbrück D, Wulke C et al (2009) Validation of the EORTC QLQ-C30 and EORTC QLQ-H&N35 in patients with laryngeal cancer after surgery. Head Neck 31:64–76. https://doi.org/10.1002/hed.20938
van der Geer SJ, van Rijn PV, Kamstra JI et al (2019) Criterion for trismus in head and neck cancer patients: a verification study. Support Care Cancer 27:1129–1137. https://doi.org/10.1007/s00520-018-4402-z
Beltran-Alacreu H, López-De-Uralde-Villanueva I, Paris-Alemany A et al (2014) Intra-rater and inter-rater reliability of mandibular range of motion measures considering a neutral craniocervical position. J Phys Ther Sci 26:915–920. https://doi.org/10.1589/jpts.26.915
Beck SL, Schwartz AL, Towsley G et al (2004) Psychometric evaluation of the Pittsburgh sleep quality index in cancer patients. J Pain Symptom Manage 27:140–148. https://doi.org/10.1016/j.jpainsymman.2003.12.002
Janssen I, Heymsfield SB, Baumgartner RN, Ross R (2000) Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol 89:465–471. https://doi.org/10.1152/jappl.2000.89.2.465
Madley-Dowd P, Hughes R, Tilling K, Heron J (2019) The proportion of missing data should not be used to guide decisions on multiple imputation. J Clin Epidemiol 110:63–73. https://doi.org/10.1016/j.jclinepi.2019.02.016
Cohen J (1992) A power primer. Psychol Bull 112:155–159. https://doi.org/10.1037/0033-2909.112.1.155
Kim JH (2019) Multicollinearity and misleading statistical results. Korean J Anesthesiol 72:558–569. https://doi.org/10.4097/kja.19087
Kraaijenga SAC, Oskam IM, Van Der Molen L et al (2015) Evaluation of long term (10-years+) dysphagia and trismus in patients treated with concurrent chemo-radiotherapy for advanced head and neck cancer. Oral Oncol 51:787–794. https://doi.org/10.1016/j.oraloncology.2015.05.003
Hansen T, Kjaersgaard A (2020) Item analysis of the Eating Assessment Tool (EAT-10) by the Rasch model: A secondary analysis of cross-sectional survey data obtained among community-dwelling elders. Health Qual Life Outcomes 18:1–14. https://doi.org/10.1186/s12955-020-01384-2
Mootassim-Billah S, Van Nuffelen G, Schoentgen J et al (2021) Assessment of cough in head and neck cancer patients at risk for dysphagia—An overview. Cancer Rep 4:1–10. https://doi.org/10.1002/cnr2.1395
Nguyen NP, Moltz CC, Frank C et al (2007) Effectiveness of the cough reflex in patients with aspiration following radiation for head and neck cancer. Lung 185:243–248. https://doi.org/10.1007/s00408-007-9016-z
Beetz I, Schilstra C, Burlage FR et al (2012) Development of NTCP models for head and neck cancer patients treated with three-dimensional conformal radiotherapy for xerostomia and sticky saliva: The role of dosimetric and clinical factors. Radiother Oncol 105:86–93. https://doi.org/10.1016/j.radonc.2011.05.010
Watters AL, Cope S, Keller MN et al (2019) Prevalence of trismus in patients with head and neck cancer: A systematic review with meta-analysis. Head Neck 41:3408–3421. https://doi.org/10.1002/hed.25836
Santoso AMM, Jansen F, Lissenberg-Witte BI et al (2021) Sleep quality trajectories from head and neck cancer diagnosis to six months after treatment. Oral Oncol 115:105211. https://doi.org/10.1016/j.oraloncology.2021.105211
Li N, Otomaru T, Taniguchi H (2017) Sleep quality in long-term survivors of head and neck cancer: preliminary findings. Support Care Cancer 25:3741–3748. https://doi.org/10.1007/s00520-017-3804-7
Wakabayashi H, Takahashi R, Watanabe N et al (2017) Prevalence of sarcopaenia and its association with dysphagia in cancer patients who require rehabilitation. J Rehabil Med 49:682–685. https://doi.org/10.2340/16501977-2253
Meerkerk CDA, Chargi N, de Jong PA et al (2022) Low skeletal muscle mass predicts frailty in elderly head and neck cancer patients. Eur Arch Oto-Rhino-Laryngology 279:967–977. https://doi.org/10.1007/s00405-021-06835-0
Maehara T, Nishimura R, Yoshitake A et al (2023) Association of daily physical activity and leisure-time exercise with dysphagia risk in community-dwelling older adults: a cross-sectional study. Sci Rep 13:10893. https://doi.org/10.1038/s41598-023-37605-z
Nagayoshi M, Higashi M, Takamura N et al (2017) Social networks, leisure activities and maximum tongue pressure: Cross-sectional associations in the Nagasaki Islands Study. BMJ Open 7:1–10. https://doi.org/10.1136/bmjopen-2016-014878
Ramia P, Bodgi L, Mahmoud D et al (2022) Radiation-Induced Fibrosis in Patients with Head and Neck Cancer: A Review of Pathogenesis and Clinical Outcomes. Clin Med Insights Oncol 16:11795549211036898. https://doi.org/10.1177/11795549211036898
Pauli N, Johnson J, Finizia C, Andréll P (2013) The incidence of trismus and long-term impact on health-related quality of life in patients with head and neck cancer. Acta Oncol 52:1137–1145. https://doi.org/10.3109/0284186X.2012.744466
Bensadoun RJ, Riesenbeck D, Lockhart PB et al (2010) A systematic review of trismus induced by cancer therapies in head and neck cancer patients. Support Care Cancer 18:1033–1038. https://doi.org/10.1007/s00520-010-0847-4
Nishida T, Yamabe K, Honda S (2020) Dysphagia is associated with oral, physical, cognitive and psychological frailty in Japanese community-dwelling elderly persons. Gerodontology 37:185–190. https://doi.org/10.1111/ger.12455
Brook I (2020) Late side effects of radiation treatment for head and neck cancer. Radiat Oncol J 38:84–92. https://doi.org/10.3857/ROJ.2020.00213
El Hage Chehade N, Fu Y, Ghoneim S et al (2023) Association between obstructive sleep apnea and gastroesophageal reflux disease: A systematic review and meta-analysis. J Gastroenterol Hepatol 38(8):1244–1251. https://doi.org/10.1111/jgh.16245
Kang HH, Lim C-H, Oh JH et al (2021) The Influence of Gastroesophageal Reflux Disease on Daytime Sleepiness and Depressive Symptom in Patients With Obstructive Sleep Apnea. J Neurogastroenterol Motil 27:215–222. https://doi.org/10.5056/jnm20071
Roscoe JA, Kaufman ME, Matteson-Rusby SE et al (2007) Cancer-Related Fatigue and Sleep Disorders. Oncologist 12:35–42. https://doi.org/10.1634/theoncologist.12-s1-35
Acknowledgements
Authors are grateful to all participants who made this work possible. We are also grateful to the staff of American Journal Experts for their assistance with the English language.
Funding
Funding for open access publishing: Universidad de Granada/CBUA. This work was supported by the Consejería de Salud, Junta de Andalucía (PI-0187–2021 and PI-0171–2020) and co-funded by European Regional Development Fund (ERDF-FEDER).
Author information
Authors and Affiliations
Contributions
A.M.R.M. was a coordinator responsible in the patient’s recruitment. N.G.C., L.O.C., C.F.L., M.A.F.G. and M.D.L.F were responsible for data acquisition, data control and writing of the manuscript draft. C.F.L., N.G.C. and M.L.L. were responsible for study supervision. N.G.C., M.D.L.F. and M.L.L. performed data curation, formal analysis, validation, and visualisation of the study data. All authors critically revised the manuscript. C.F.L. and N.G.C. were responsible for the study financing and project coordination. A.M.R.F, L.O.C., M.A.F.G. and M.L.L critically revised the manuscript for intellectual content. All authors have approved the final version of this manuscript to be submitted. The authors have no relevant financial or non-financial interests to disclose. This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Biomedical Investigation Ethics Committee, Granada, Spain (CEi-GRANADA Ref: 0045-N-16 and 1552-N-18). Moreover, informed consent was obtained from all individual participants included in the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
López-Fernández, M.D., Fernández-Lao, C., Ruíz-Martínez, A.M. et al. Exploring predictors of dysphagia in survivors of head and neck cancer: A cross-sectional study. Support Care Cancer 32, 162 (2024). https://doi.org/10.1007/s00520-024-08358-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08358-w