Abstract
Purpose
Patients with cancer may experience pain from cancer itself or its treatment. Additionally, chronic pain (CP) predating a patient’s cancer diagnosis may make the etiology of pain less clear and the management of pain more complex. In this brief report, we investigated differences in biopsychosocial characteristics, pain severity, and opioid consumption, comparing groups of cancer patients with and without a history of CP who presented to the emergency department (ED) with a complaint of cancer-related pain.
Methods
This secondary analysis of a prospective cohort study included patients with cancer who presented to the ED with a complaint of pain (≥ 4/10). Sociodemographic, clinical, psychological, and pain characteristics were assessed in the ED and subsequent hospitalization. Mann-Whitney U-, T-, and Chi-square tests were used to compare differences between patients with and without pre-existing CP before cancer.
Results
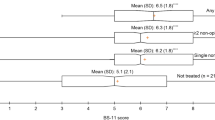
Patients with pre-existing CP had lower income (p = 0.21) and less formal education (p = 0.25) and were more likely to have a diagnosis of depression or substance use disorder (p < 0.01). Patients with pre-existing CP reported significantly greater pain severity in the ED and during hospitalization compared to those without pre-existing CP (p < 0.05), despite receiving greater amounts of opioid analgesics (p = 0.036).
Conclusion
Identifying a history of pre-existing CP during intake may help identify patients with cancer with difficult to manage pain, who may particularly benefit from multimodal interventions and supportive care. In addition, referral of these patients for the management of co-occurring pain disorders may help decrease the usage of the ED for undertreated pain.


Similar content being viewed by others
References
Caterino JM, Adler D, Durham DD, Yeung SJ, Hudson MF, Bastani A, Bernstein SL, Baugh CW, Coyne CJ, Grudzen CR et al (2019) Analysis of diagnoses, symptoms, medications, and admissions among patients with cancer presenting to emergency departments. JAMA Netw Open 2(3):e190979
Rivera DR, Gallicchio L, Brown J, Liu B, Kyriacou DN, Shelburne N (2017) Trends in adult cancer-related emergency department utilization: an analysis of data from the nationwide emergency department sample. JAMA Oncol 3(10):e172450
Mayer DK, Travers D, Wyss A, Leak A, Waller A (2011) Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol 29(19):2683–2688
Roy M, Halbert B, Devlin S, Chiu D, Graue R, Zerillo JA (2021) From metrics to practice: identifying preventable emergency department visits for patients with cancer. Support Care Cancer 29(7):3571–3575
Hong AS, Sadeghi N, Harvey V, Lee SC, Halm EA (2019) Characteristics of emergency department visits and select predictors of hospitalization for adults with newly diagnosed cancer in a safety-net health system. J Oncol Pract 15(6):e490–e500
Valeberg BT, Miaskowski C, Hanestad BR, Bjordal K, Paul S, Rustøen T (2008) Demographic, clinical, and pain characteristics are associated with average pain severity groups in a sample of oncology outpatients. J Pain 9(10):873–882
Hasuo H, Ishiki H, Matsuoka H, Fukunaga M (2021) Clinical characteristics of myofascial pain syndrome with psychological stress in patients with cancer. J Palliat Med 24(5):697–704
Hasuo H, Sakai K (2021) Clinical characteristics of noncancer-related upper back pain on initiation of palliative care in patients with incurable cancer. Palliat Med Rep 2(1):335–339
Ruppert LM, Cohn ED, Keegan NM, Bacharach A, Woo S, Gillis T, Scher HI (2022) Spine pain and metastatic prostate cancer: defining the contribution of nonmalignant etiologies. JCO Oncol Pract 18(6):e938–e947
Jairam V, Yang DX, Yu JB, Park HS (2020) Emergency department visits for opioid overdoses among patients with cancer. J Natl Cancer Inst 112(9):938–943
Organization WH: WHO guidelines for the pharmacological and radiotherapeutic management of cancer pain in adults and adolescents. 2018.
Higgins C, Smith BH, Matthews K (2019) Evidence of opioid-induced hyperalgesia in clinical populations after chronic opioid exposure: a systematic review and meta-analysis. Br J Anaesth 122(6):e114–e126
Shah R, Chou LN, Kuo YF, Raji MA (2019) Long-term opioid therapy in older cancer survivors: a retrospective cohort study. J Am Geriatr Soc 67(5):945–952
Azizoddin DR, Schreiber K, Beck MR, Enzinger AC, Hruschak V, Darnall BD, Edwards RR, Allsop MJ, Tulsky JA, Boyer E, Mackey S (2021) Chronic pain severity, impact, and opioid use among patients with cancer: an analysis of biopsychosocial factors using the CHOIR learning health care system. Cancer 127(17):3254–3263
Belfer I, Schreiber KL, Shaffer JR, Shnol H, Blaney K, Morando A, Englert D, Greco C, Brufsky A, Ahrendt G et al (2013) Persistent postmastectomy pain in breast cancer survivors: analysis of clinical, demographic, and psychosocial factors. J Pain 14(10):1185–1195
Schreiber KL, Martel MO, Shnol H, Shaffer JR, Greco C, Viray N, Taylor LN, Mclaughlin M, Brufsky A, Ahrendt G et al (2013) Persistent pain in postmastectomy patients: comparison of psychophysical, medical, surgical, and psychosocial characteristics between patients with and without pain. Pain 154(5):660–668
Azizoddin DR, Beck M, Flowers KM, Wilson JM, Chai P, Johnsky L, Cremone G, Edwards R, Hasdianda A, Boyer E, Schreiber KL (2022) Psychological evaluation of patients with cancer presenting to the emergency department with pain: independent predictors of worse pain severity, interference, and higher hourly opioid administration. JCO Oncol Pract 18(10):e1648–e1660
Azizoddin DR, Wilson JM, Flowers KM, Beck M, Chai P, Enzinger AC, Edwards R, Miaskowski C, Tulsky JA, Schreiber KL (2023) Daily pain and opioid administration in hospitalized patients with cancer: the importance of psychological factors, recent surgery, and current opioid use. Pain 164(8):1820–1827
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (redcap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, Mcleod L, Delacqua G, Delacqua F, Kirby J, Duda SN (2019) The redcap consortium: building an international community of software platform partners. J Biomed Inform 95:103208
Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D (2011) Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment 18(3):263–283
Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S et al (2010) The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol 63(11):1179–1194
Sullivan MJL, Bishop SR, Pivik J (1995) The pain catastrophizing scale: development and validation. Psychol Assess 7(4):524–532
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24(4):385–396
Tan G, Jensen MP, Thornby JI, Shanti BF (2004) Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain 5(2):133–137
Bredal I, Smeby NA, Ottesen S, Warncke T, Schlichting E (2014) Chronic pain in breast cancer survivors: comparison of psychosocial, surgical, and medical characteristics between survivors with and without pain. J Pain Symptom Manage 48(5):852–862
Edwards RR, Mensing G, Cahalan C, Greenbaum S, Narang S, Belfer I, Schreiber KL, Campbell C, Wasan AD, Jamison RN (2013) Alteration in pain modulation in women with persistent pain after lumpectomy: influence of catastrophizing. J Pain Symptom Manage 46(1):30–42
Chen YK, Boden KA, Schreiber KL (2021) The role of regional anaesthesia and multimodal analgesia in the prevention of chronic postoperative pain: a narrative review. Anaesthesia 76 Suppl 1((Suppl 1)):8–17
Prego-Domínguez J, Khazaeipour Z, Mallah N, Takkouche B (2021) Socioeconomic status and occurrence of chronic pain: a meta-analysis. Rheumatology (Oxford) 60(3):1091–1105
Meints SM, Cortes A, Morais CA, Edwards RR (2019) Racial and ethnic differences in the experience and treatment of noncancer pain. Pain Manag 9(3):317–334
Kim HJ, Yang GS, Greenspan JD, Downton KD, Griffith KA, Renn CL, Dorsey SG (2017) Racial and ethnic differences in experimental pain sensitivity: systematic review and meta-analysis. Pain 158(2):194–211
Tait RC, Chibnall JT (2014) Racial/ethnic disparities in the assessment and treatment of pain: psychosocial perspectives. Am Psychol 69(2):131
Mackey LM, Blake C, Casey MB, Power CK, Victory R, Hearty C, Fullen BM (2019) The impact of health literacy on health outcomes in individuals with chronic pain: a cross-sectional study. Physiotherapy 105(3):346–353
Canjuga M, Läubli T, Bauer GF (2010) Can the job demand control model explain back and neck pain? Cross-sectional study in a representative sample of Swiss working population. Int J Ind Ergon 40(6):663–668
Yilmaz E, Dedli O (2012) Effect of physical and psychosocial factors on occupational low back pain. Health Sci J 6(1):598
Mystakidou K, Tsilika E, Parpa E, Katsouda E, Galanos A, Vlahos L (2006) Psychological distress of patients with advanced cancer: influence and contribution of pain severity and pain interference. Cancer Nurs 29(5):400–405
Deandrea S, Montanari M, Moja L, Apolone G (2008) Prevalence of undertreatment in cancer pain. A review of published literature. Ann Oncol 19(12):1985–1991
Anderson KO, Green CR, Payne R (2009) Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain 10(12):1187–1204
Campbell CM, Edwards RR (2012) Ethnic differences in pain and pain management. Pain Manag 2(3):219–230
Gorin S, Krebs P, Badr H, Janke EA, Jim HS, Spring B, Mohr DC, Berendsen MA, Jacobsen PB (2012) Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. J Clin Oncol 30(5):539–547
Tatrow K, Montgomery GH (2006) Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: a meta-analysis. J Behav Med 29(1):17–27
Somers TJ, Kelleher SA, Westbrook KW, Kimmick GG, Shelby RA, Abernethy AP, Keefe FJ (2016) A small randomized controlled pilot trial comparing mobile and traditional pain coping skills training protocols for cancer patients with pain. Pain Res Treat 2016:2473629
Katta MR, Valisekka SS, Agarwal P, Hameed M, Shivam S, Kaur J et al (2022) Non-pharmacological integrative therapies for chronic cancer pain. J Oncol Pharm Pract 28(8):1859–1868
Darnall BD, Roy A, Chen AL, Ziadni MS, Keane RT, You DS, Slater K, Poupore-King H, Mackey I, Kao MC et al (2021) Comparison of a single-session pain management skills intervention with a single-session health education intervention and 8 sessions of cognitive behavioral therapy in adults with chronic low back pain: a randomized clinical trial. JAMA Netw Open 4(8):e2113401
Acknowledgements
Mohammad Adrian Hasdianda, Lily Johnsky, and other research and healthcare staff in Brigham and Women’s Hospital Emergency Department, as well as all participants are acknowledged.
Funding
This study was supported by NIH R35 GM128691 (KLS), National Palliative Care Research Center (DRA), NIH NCI K08 CA266937 (DRA), NIH K23 DA044874, and DP2DA056107 (PRC).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by MB, KLS, MFl, and DRA. The first draft of the manuscript was written by MB and DRA, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by Mass General Brigham IRB (no.: Partners IRB 2019P002230 approved 09/10/2019). Participants provided informed consent to participate and study activities conformed to the 1964 Helsinki Declaration and following amendments.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Beck, M., Schreiber, K.L., Wilson, J.M. et al. A secondary analysis: the impact of pre-existing chronic pain among patients with cancer presenting to the emergency department with acute pain. Support Care Cancer 32, 129 (2024). https://doi.org/10.1007/s00520-024-08314-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08314-8