Abstract
Purpose
Patients diagnosed with cancer might experience changes in intimacy and sexuality due to the illness itself, treatment, or psychological and social factors. Healthcare professionals (HCPs) often feel reluctant to discuss these changes. This study aimed to provide an overview of the feasibility and effectiveness of communication tools that support communication regarding changes in intimacy or sexuality among patients with cancer.
Methods
This is a systematic review. Databases are PubMed, Embase, CINAHL, PsycInfo, Web of Science and Cochrane Library from inception to June 2023. The Mixed Methods Appraisal Tool was used to assess included studies. Data were summarized in data charting forms.
Results
In total 35 studies were included, published between 2001 and 2023. Most had a quantitative design and moderate methodological quality. In 11 studies, the PLISSIT model (Permission, Limited Information, Specific Suggestions, Intensive Therapy) was used. Tools were integrated in counselling sessions or training programmes for individual patients, couples, groups of patients, or HCPs. All tools were considered feasible by patients or HCPs. Twenty studies reported significant improvement in sexual functioning, quality of life, quality of care or combined outcomes.
Conclusion
Tools to support communication about changes in intimacy and sexuality among patients with cancer seem feasible and effective. The most commonly used tool, the PLISSIT model, proved to be feasible for HCPs and to have a positive effect on patients’ and partners’ sexual functioning and quality of life. Giving attention to changes in intimacy and sexuality seems to be important in itself, regardless of the communication tool or approach used.
Similar content being viewed by others
Introduction
Cancer and its treatment may cause changes regarding intimacy and sexuality in patients [1,2,3]. Sexuality can be described as a central aspect of human beings that encompasses sexual self-concept, sexual functioning and sexual relationships [1, 4, 5]. In addition, sexuality can refer to sexual health, sexual pleasure, sexual awareness, self-esteem and sexual orientation [5,6,7,8,9]. Intimacy can be defined as an interactive process that occurs when a person discloses self-relevant feelings or information, resulting in feeling understood, cared for and accepted by the reaction of the other individual involved in the interaction [10, 11]. Moreover, intimacy is characterized as a quality of an interpersonal relationship in which individuals have reciprocal feelings of trust, connectedness, caring and emotional closeness and are able to openly communicate their thoughts and feelings with each other [12]. Intimate relationships can involve both emotional intimacy (e.g. sharing thoughts and feelings) and physical intimacy (e.g. touching and closeness) [12].
Changes in intimacy and sexuality can arise due to the cancer itself, the treatment or psychological and social factors such as anxiety or distress [13]. For instance, cancer treatment might cause problems with sexual desire and arousal problems [14,15,16]. Changes in sexuality can persist for years and can be extremely distressing for patients with cancer and their intimate partners [17].
Patients with cancer or patients who survived cancer have reported a need for information regarding changes in intimacy and sexuality [6]. Addressing sexual health adequately and timely, e.g. before, during and after treatment, may be crucial in identifying sexual problems and might ensure appropriate treatment and support [18, 19]. Discussing these issues can alleviate anxiety and psychological distress [20,21,22] and may improve the quality of sexual or intimate life [18, 22, 23]. In addition, failure to address the need for information can be associated with increased psychological morbidity, including depression and relational dissatisfaction, as well as a reduction in self-efficacy and overall quality of life [24].
Though these are important issues, healthcare professionals often feel reluctant to discuss changes in intimacy and sexuality, and they frequently remain unaddressed in cancer care [2, 17, 25,26,27,28]. Several barriers faced by healthcare professionals have been recognized, such as a lack of time, lack of privacy [29], feeling uncomfortable discussing the topic, the patient’s advanced age [30] and a lack of skills, training and knowledge [1, 22, 27, 31].
Research suggests that communication tools may help overcome barriers and help healthcare professionals to initiate a conversation with patients about changes in intimacy and sexual concerns [32,33,34,35]. These tools can consist of models, guides or training that support communication with patients about intimacy and sexuality. In a previously conducted narrative review, several specific tools were identified that address sexual health issues in terminally ill patients, including the stepwise PLISSIT model (Permission, Limited Information, Specific Suggestions, Intensive Therapy) [22]. However, this study did not address the effectiveness or feasibility of the identified tools [22]. Consequently, the question of which tools are effective and feasible for addressing changes in intimacy and sexuality remains unanswered.
In order to answer this question, we sought to provide an overview of the feasibility and effectiveness of tools that support communication regarding changes in intimacy or sexuality with patients with cancer in inpatient and outpatient care. We address the following review questions in this review:
-
1)
What evidence exists for the feasibility of these tools, from the perspectives of the professionals and patients involved?
-
2)
What evidence exists for the effectiveness of tools that support communication about concerns and needs regarding intimacy or sexuality with patients with cancer?
-
3)
What differences are found between patients with advanced cancer, patients with early stage cancer and cancer survivors in the feasibility and effectiveness of these communication tools?
Methods
Design
We conducted a systematic review to identify studies that focused on tools that support communication between patients and healthcare professionals about concerns regarding intimacy or sexuality. The review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [36], and the protocol is registered in PROSPERO (CRD42021283852).
Search strategy
A comprehensive search was performed in collaboration with a medical librarian (LS) in the bibliographic databases PubMed, Embase.com, Cinahl (Ebsco), APA PsycInfo (Ebsco), the Web of Science Core Collection and the Cochrane Library (Wiley) from inception to 26 June 2023. The search strategy consisted of free-text terms and controlled vocabulary for ‘cancer’ and ‘sexuality’ or ‘intimacy’ and ‘communication’. A search filter was used to exclude children. No language or time restrictions were included in the search strategy. In addition, the reference lists of all included studies were screened for relevant records. Duplicate articles were excluded (LS) using Endnote X20.01 (Clarivate™). The full search strategies are provided in Supplemental Material III.
Eligibility criteria
We included all types of empirical quantitative, qualitative or mixed-methods studies that focus on the following:
-
Tools (including models, guides, educational programmes or interventions) that promote and/or support communication between healthcare professionals and patients about concerns and needs regarding intimacy and sexuality.
-
Adult patients (18 years of age or older) with any type and stage of cancer, including cancer survivors.
-
Inpatient or outpatient settings.
-
Outcomes regarding the effectiveness or feasibility of the aforementioned communication tools. More specifically, these were outcomes directly related to sexuality, quality of life (i.e. physical, psychological, social or spiritual aspects) or quality of care (i.e. perceived quality of care or perceived satisfaction with communication). Outcomes regarding feasibility included perceptions and experiences related to usability, willingness to participate, duration of the applied intervention and lost to follow-up.
In the first selection procedure we came upon studies that included mixed populations (patients with various diseases). In addition to the above criteria and after discussion in the research group, we decided to exclude studies that involved mixed populations if it was not possible to extract data for only patients with cancer.
Study selection
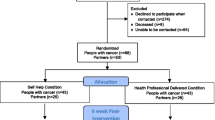
Titles and abstracts were independently screened for potential eligibility by two reviewers (IJ and SA or CR or JR), using the systematic review software Rayyan (2016). Subsequently, two authors (IJ and SA or CR or JR) screened the full texts for eligibility. Any disagreement between authors was resolved by discussion with two other researchers (CE, AF). The study selection procedure and results can be found in the flow diagram in Fig. 1.
PRISMA flowchart [36]
Quality assessment
The methodological quality of the included studies was assessed independently by two reviewers (SA and CR or JR or IJ) using the Mixed Methods Appraisal Tool version 2018 (MMAT) [37]. The MMAT tool is designed to appraise the methodological quality of quantitative, qualitative and mixed-method studies [37]. Each study was evaluated using five quality items, depending on the study design. The items were rated by answering ‘Yes’ (green), ‘No’ (red) or ‘Can’t tell’ (orange). The latter category meant that the paper did not report enough information to answer ‘Yes’ or ‘No’. We did not contact authors for additional clarification; however, we did look for subsequent papers that might provide an answer. Any disagreement between reviewers was resolved by discussion and with the involvement of an additional reviewer (IJ). MMAT scores are presented as global scores (Supplemental I) and are indicated by stars (*) in the tables. The stars correspond to the number of questions answered with ‘Yes’ (Table 1).
Data extraction
Three researchers (SA, CR, IJ) independently extracted data from the included studies in a predefined form. The following study characteristics were extracted: year of publication, country, study design, study population (including number of participants and age) and communication tool. For feasibility, where applicable, we extracted data on usage, willingness to participate, lost to follow-up and duration of the intervention. For effectiveness, we extracted data on outcomes related to intimacy and sexuality, quality of life and quality of care that were measured in patients, their partners or healthcare professionals.
Data synthesis
We decided beforehand not to do a meta-analysis because of expected heterogeneity in design and outcomes. Instead, we synthesized outcomes using a narrative approach and predesigned data charting forms. Data were extracted independently by two researchers (SA and CR or SA and IJ). The data charting forms were discussed with two other researchers (CE and AF). After several discussion rounds, all researchers agreed upon the finalized version of the charting tables.
Results
Results of the selection process
The literature search generated a total of 11,269 references. After removing duplicates, 6472 records were screened for eligibility based on title and abstract (Fig. 1). We excluded 6295 records, mainly because these studies did not focus on adult patients with cancer or did not include a tool supporting communication between healthcare professionals and patients. Five studies were excluded because they were written in Chinese or Korean and we were unable to read and assess the full text [70,71,72,73,74]. After reading the full text of 177 remaining references, we included 35 articles, published between 2001 and 2023. Of these, four articles concerned the same study, but were reporting different outcomes. Therefore, they were included as separate studies.
In total, 2567 patients (number per study ranging from 7 to 318), 677 partners (ranging from 7 to 189) and 423 healthcare professionals (ranging from 7 to 140), the majority being nurses (n = 215), were included in the studies. Most of the included patients in these studies were female (n = 2234, 87.0%). The mean age of the participating patients ranged from 34.2 to 62.7 years and of participating partners from 47.4 to 61.6 years (see Table 1). The country with the most studies was Iran (n = 9), followed by the USA (n = 5).
Methodological quality of the studies
The designs used and evaluated, as identified by the MMAT tool [37], were randomized controlled trials (RCTs) (n = 15), quantitative non-randomized studies (n = 12), qualitative studies (n = 2) and mixed methods studies (n = 6). Quality assessment scores using the MMAT tool ranged from 0 to 5 out of 5 (Supplemental I). Only two RCTs had maximum scores (5 out of 5 items present). Six of the 35 studies had low scores (0 or 1 out of 5 items); two were RCTs and four were mixed methods studies.
Tools supporting communication about intimacy and sexuality
Various tools were described in the 35 included studies, (see Table 1). The most commonly used tool was the specific, stepwise model PLISSIT [39, 48,49,50, 54, 61, 66, 75]. Two studies used the Extended PLISSIT model (EX-PLISSIT), which differs from the original PLISSIT model in that it is feedback-oriented while PLISSIT is a linear model [59, 68]. Other tools used were BETTER (Bring up the topic, Explain, Telling, Timing, Education, Recording), EASSi (Engagement, Assessment, Support and Signposting) or self-developed tools. Tools were applied in counselling sessions, educational programmes, intervention programmes and nurse-led interventions (see Supplemental II).
Thirteen of the 35 studies focused on tools that support communication with individual patients with cancer or cancer survivors. Nine studies used communication tools for couples (patients with cancer and their intimate partner). Five studies focused on the use of communication tools for groups of patients and two studies used communication tools for both individual patients and couples or groups. Communication tools for healthcare professionals, predominantly nurses and nurse specialists, were used in six studies. These tools were applied in training sessions for healthcare professionals to equip them for conversations with their patients (Supplemental II).
Feasibility of communication tools
In 33 studies, feasibility was assessed with regard to duration, usability, willingness to participate and lost to follow-up (see Table 2).
Duration of the intervention
The duration of the intervention programme for the tools, such as counselling sessions, home visits or educational programmes, ranged from one single session to eight sessions, with each session ranging from 30 up to 120 min (see Table 2).
Usability
Ten studies reported outcomes relating to usability. Overall, patients, partners and healthcare professionals experienced tools as useful in increasing awareness about the topic, valuable and helpful in addressing intimacy and sexuality, and simple to use. In one study, healthcare professionals considered the tablet-based Engagement, Assessment, Support and Signposting tool (EASSi) as less suitable when patients were medically unstable, were attending the appointments with a family member (other than their partner), or when patients were not concerned about sexual issues [19].
Willingness to participate
Data on willingness to participate could be extracted from 24 studies. Rates varied from 19% in two studies [49, 55] to 100% in two studies [41, 57]. Of the two studies where willingness to participate was 100%, one study involved a clinical nurse specialist intervention in individual patients [57] and the other study involved a problem-solving approach for groups of patients [41]. Both high and low rates of willingness to participate were found in individual (19% to 100%) and group interventions (19% to 100%). Two studies among healthcare professionals reported on willingness to participate (56.7% and 87.5%) [34, 40].
Lost to follow-up
In 25 studies, lost to follow-up or compliance rate was reported, indicating the willingness to continue participation in the programme or comply with the intervention. Lost to follow-up rates ranged from 1.7% in a study among couples to 57% in a study applying PLISSIT in individual patients. Lost to follow-up varied in studies with individual patients (2.0% to 57.0%), in couples (1.7% to 35.7%) and in groups of patients (10.0% to 21.7%).
Effectiveness of communication tools related to intimacy and sexuality
Of the 35 publications, 34 reported outcomes that indicate effectiveness i.e. outcomes related to intimacy and sexuality, quality of life or quality of care.
Outcomes related to intimacy and sexuality
Twenty-two studies reported on outcomes related to intimacy and sexuality, i.e. sexual function, sexual distress, sexual concerns, sexual communication, sexual behaviour and sexual satisfaction (see Table 3). Besides sexual functioning, some studies also measured outcomes related to intimacy and sexuality, such as sexual self-confidence, sexual concerns, sexual beliefs and relationship satisfaction.
Sexual function was assessed with the Female Sexual Function Index (FSFI, 13 studies), the Changes in Sexual Functioning Questionnaire (CSFQ-14, one study), the International Index of Erectile Function (IIEF, two studies), the Lasry Sexual Functioning Scale (LSFS, one study), the Patient-Reported Outcomes Measurement Information System Sexual Function and Satisfaction (PROMIS SexFS, one study), the Sexual Health Inventory for Men (SHIM, one study), or a self-developed questionnaire consisting of several items related to sexual function (one study). A statistically significant improvement was found over time in the patient’s sexual functioning in 11 studies, mostly in studies among individual patients. Of these, five studies based their intervention on PLISSIT [38, 48, 50, 54, 59]. One study among couples indicated improvement in female sexual functioning and little improvement in male sexual functioning, without providing information about significance [62]. Six studies did not find a significant difference over time [39, 43, 47, 56, 57, 61].
Sexual distress among individual patients was assessed in two studies, using the Index of Sexual Satisfaction and the Female Sexual Distress Scale-Revised (FSDS-R). Both studies reported a decrease in sexual distress [54, 62]. Of these studies, one study applied PLISSIT-based counselling among individuals [54] and the other study applied a phone-based intervention among couples [62].
Relationship satisfaction was assessed in four studies with the (Brief) Dyadic Adjustment Scale [43, 48, 60, 62] and in one study with the Chinese version of the Revised Dyadic Adjustment Scale (CR-DAY) [56]. Relationship satisfaction significantly improved in one study that used PLISSIT counselling among individuals [48], in one study that applied individual counselling based on the BETTER model [60], and in one study that used a psychosocial intervention among couples [56]. One study, which used a phone-based couple intervention discussing physical intimacy and sexual concerns, indicated a medium-sized effect on relationship satisfaction [62]. This was the only study that reported on intimacy and it indicated little improvement.
Outcomes related to quality of life
Nineteen studies reported on outcomes regarding quality of life. Besides overall quality of life (17 studies), studies also reported effects on other related outcomes (six studies), such as sexual quality of life, psychological well-being and body image (see Table 2).
Overall quality of life was assessed using various questionnaires. The assessment was made using the Sexual Quality of Life-Female (SCOL-F, five studies), followed by the European Organization for Research and Treatment for Cancer Quality of Life Questionnaire (EORTC-QLQ-C30, four studies), the World Health Organization Quality of Life Questionnaire-BREF (WHOQoL-BREF, two studies) and the Functional Assessment of Cancer Therapy-General (FACT-G, three studies), the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Breast (EORTC-QLQ-BR23, one study), the Medical Outcomes Study Health Survey Short Form (SF-12, one study), or a self-developed questionnaire (one study).
In total, seven studies reported a statistically significant improvement over time in overall quality of life [38, 42, 51, 54, 56, 57, 66]. Of these, three studies based their intervention on PLISSIT, which was applied to individual patients [38, 54, 66]. The remaining ten studies did not report a significant difference in overall quality of life. Among these studies, five based their intervention on PLISSIT among individuals (one study) [49], couples (two studies) [50, 61] and groups (three studies) [39, 46, 59].
Psychological well-being was assessed in four studies using the Hospital Anxiety and Depression Scale (HADS, three studies) and the Self-Rating Depression Scale (SDS, one study). A significant reduction in anxiety was found in one study using an educational intervention, based on the principles of social cognitive theory, among individual patients [63]. Another study among individuals with the same intervention reported a reduction in anxiety and depression symptoms, but did not report on significance [64]. Furthermore, in a group of patients receiving an education-based nursing intervention, a decrease in severity of depression was found as compared to the control group [46]. The remaining study, which applied couple-based PLISSIT counselling, did not find a significant difference in psychological well-being [61].
Also, one study that applied PLISSIT-based counselling among individuals [48] reported a significant reduction in treatment-related side effects and a significant improvement in body image, assessed with the Body Image Scale.
Outcomes related to quality of care
Eleven studies reported on outcomes regarding quality of care, i.e. satisfaction with communication or other outcomes related to quality of care (see Table 3).
Outcomes related to satisfaction with communication were reported in seven studies. Satisfaction with communication was assessed with the Dyadic Sexual Communication scale (two studies), self-developed items (two studies), audio recordings (two studies) and the Olson Martial Quality Questionnaire (one study). A statistically significant improvement in communication after the intervention was found in only one study, which used a self-developed nurse-led programme among couples [69]. Four studies indicated an improvement in communication, but did not report any information regarding significance [34, 62, 64, 68]. Of these four studies, one study applied PLISSIT in training for healthcare professionals and indicated an increase in discussions of sexual health and improvement of communication behaviours after the intervention [34]. Furthermore, one study reported that there was no significant difference in sexual communication after applying PLISSIT-based counselling among couples [61].
Sexual attitudes were assessed with the Sexual Attitudes and Beliefs Survey (SABS) (two studies) [40, 58] and a patient survey (one study) [19]. Only one study reported a significant improvement after the intervention, which consisted of an eLearning resource for healthcare professionals; it stated that healthcare professionals experienced fewer barriers to providing sexual support [40].
Also, one study among individuals reported on referrals. It found no significant effects of the screening-tool for sexual health on numbers of referrals to a sexual counsellor or pelvic floor physiotherapist, based on patients’ medical records [65].
Differences in feasibility and effectiveness of communication tools between early stage cancer, advanced cancer and cancer survivors
Of the 35 publications, eight studies focused on cancer survivors [38, 39, 47, 50, 51, 54, 59, 65]. The interventions included in these studies were PLISSIT-based in four studies [39, 50, 54, 59] and based on other tools in the remaining four studies [38, 47, 51, 65]. Furthermore, five of these eight studies involved individual cancer survivors [38, 47, 51, 54, 65], two studies involved groups of patients [39, 59] and one study focused on couples [50]. Willingness to participate was reported in six studies and varied from 40.0% (individual patients) to 90.2% (group of patients) [38, 39, 47, 51, 54, 59]. Lost to follow-up ranged from 3.0 to 57.0% (both were studies of individual patients) [38, 54].
Of these eight studies focussing on cancer survivors, seven studies assessed sexual functioning, predominantly with the Female Sexual Function Index (FSFI). Sexual functioning significantly improved in five studies [38, 50, 51, 54, 59]. Quality of life was assessed in seven studies with different questionnaires; improvement was reported in three studies [38, 51, 54].
None of the studies compared cancer survivors with patients with cancer (early stage or advanced cancer).
Discussion
This review considered 35 studies on the feasibility and effectiveness of tools to support communication about changes in intimacy and sexuality among patients with cancer or cancer survivors. In 11 studies, the stepwise PLISSIT model was used, while a total of 15 other tools were described in the other studies. The tools were considered feasible and practical and most appeared to be effective in improving sexual functioning, quality of life and quality of care.
Based on the 35 studies, it is not possible to identify any variation in terms of feasibility and effectiveness between patients with early stage cancer and those with advanced cancer. However, previous research has shown that patients with early stage cancer can have different needs compared to patients with advanced cancer [76, 77].
The overall methodological quality of the 35 studies, as assessed with the MMAT tool, varied from low (none of the criteria were met) to high (all criteria were met). The five studies where the methodological quality was assessed as high (four or five criteria were met) used counselling based on PLISSIT, BETTER or Schover’s sexual assessment method and found statistically significant differences in sexual functioning when applied in individual patients [51, 60, 66] or groups of patients [59].
Although our review revealed a broad range of feasible and effective tools, previous research highlighted the reluctance that healthcare professionals might experience when addressing issues related to sexuality and intimacy, resulting in unaddressed issues during care for patients with cancer [17, 25, 26, 28]. Furthermore, earlier research demonstrated that communication tools can be beneficial for healthcare professionals in overcoming barriers and initiating conversations on these sensitive subjects [32,33,34]. However, due to the wide range of communication tools available and the flexibility in their application, nursing staff or other professionals might find it hard to choose a specific tool. The choice could be based on how often a tool has already been researched and found to be proven effective. This systematic review demonstrates that the PLISSIT-model stands out as both the most commonly researched tool and as an effective method for addressing intimacy and sexuality. Therefore, based on this review, the PLISSIT-model can be recommended.
Additionally, this review shows that of the 35 included studies, only one study addressed effects on intimacy; it indicated little improvement. Most of the research focuses on sexuality among patients with cancer [15, 16, 78]. Studies that focus on outcomes related to sexuality might have adopted an inclusive view that considers sexuality as a fundamental aspect of human being, occasionally encompassing intimacy within its scope [5]. Nonetheless, it is important to recognize that intimacy can be defined as an interactive process in its own right [10, 11].
Another noteworthy finding is that 12 of the studies included in our review were conducted in non-Western countries such as Iran, Turkey, Yemen and Egypt. Various non-Western cultural and religious perspectives might hinder open conversations regarding sexuality [79, 80]. However, none of these studies explicitly address cultural or religious factors. Nevertheless, it is recommended for healthcare professionals to be aware of cultural and religious aspects in their communication, especially in communication about the end of life [81].
Methodological considerations
A strength of this systematic review is that we used multiple relevant literature databases in the search process. An additional strength is that we performed a methodological appraisal of the studies that were included. The MMAT tool enabled us to assess both quantitative and qualitative research designs.
A limitation of this review is the fact that the included studies considered various outcomes and used a variety of questionnaires to assess the outcomes. Most used questionnaires are previously validated, such as FSFI, EORT-QLQ and HADS. However, because of the various outcomes and variety of questionnaires, we were unable to conduct a meta-analysis. Nevertheless, it was evident that the overall use of communication tools proved to be effective.
Another limitation of this review is that we had to exclude five articles that were written in Korean or Chinese and that seemed to fulfil our inclusion criteria [70,71,72,73,74]. Four of these studies applied PLISSIT in their intervention [71,72,73,74] and one study used a Sexual Health Improvement Programme [70]. Results regarding sexual functioning could however be read from tables and abstracts; all reported significant improvement in sexual functioning, which seems to be in line with the findings of our review [70,71,72,73,74].
Conclusion
This systematic review shows that the use of tools that support communication about changes in intimacy and sexuality among individual patients with cancer or cancer survivors, couples or groups of patients is feasible and effective. Various communication tools were used in counselling, educational or nurse-led programmes. The most commonly used tool, the stepwise PLISSIT model, proved to be feasible for HCPs and to have a positive effect on patients’ and partners’ sexual functioning and quality of life. However, the specific communication tool or approach utilized seems to matter less than the very fact of paying attention to changes in intimacy and sexuality.
References
de Vocht H, Hordern A, Notter J, van de Wiel H (2011) Stepped skills: a team approach towards communication about sexuality and intimacy in cancer and palliative care. Australas Med J 4(11):610–619
Reese JB, Porter LS, Regan KR, Keefe FJ, Azad NS, Diaz LA Jr et al (2014) A randomized pilot trial of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer. Psychooncology 23(9):1005–1013
Reese JB, Zimmaro LA, Lepore SJ, Sorice KA, Handorf E, Daly MB et al (2020) Evaluating a couple-based intervention addressing sexual concerns for breast cancer survivors: study protocol for a randomized controlled trial. Trials 21(1):173
Woods NF (1987) Toward a holistic perspective of human sexuality: alterations in sexual health and nursing diagnoses. Holist Nurs Pract 1(4):1–11
WHO (2006) Defining sexual health: report of a technical consultation on sexual health. Available from: https://www.who.int/teams/sexual-and-reproductive-health-and-research/key-areas-of-work/sexual-health/defining-sexual-health. Assessed May 2023
Albers LF, van Belzen MA, van Batenburg C, Engelen V, Putter H, Pelger RCM, Elzevier HW (2020) Discussing sexuality in cancer care: towards personalized information for cancer patients and survivors. Support Care Cancer 28(9):4227–4233
Laumann EO, Paik A, Glasser DB, Kang JH, Wang T, Levinson B et al (2006) A cross-national study of subjective sexual well-being among older women and men: findings from the Global Study of Sexual Attitudes and Behaviors. Arch Sex Behav 35(2):145–161
Mitchell KR, Lewis R, O’Sullivan LF, Fortenberry JD (2021) What is sexual wellbeing and why does it matter for public health? Lancet Public Health 6(8):e608–e613
Muise A, Preyde M, Maitland SB, Milhausen RR (2010) Sexual identity and sexual well-being in female heterosexual university students. Arch Sex Behav 39(4):915–925
Perndorfer C, Soriano EC, Siegel SD, Laurenceau JP (2019) Everyday protective buffering predicts intimacy and fear of cancer recurrence in couples coping with early-stage breast cancer. Psychooncology 28(2):317–323
Duck S, Hay DF, Hobfoll SE, Ickes W, Montgomery BME (1988) Handbook of personal relationships: Theory, research and interventions. John Wiley & Sons
Timmerman GM (1991) A concept analysis of intimacy. Issues Ment Health Nurs 12(1):19–30
Alappattu M, Harrington SE, Hill A, Roscow A, Jeffrey A (2017) Oncology section EDGE task force on cancer: a systematic review of patient-reported measures for sexual dysfunction. Rehabil Oncol 35(3):137–143
Schover LR, van der Kaaij M, van Dorst E, Creutzberg C, Huyghe E, Kiserud CE (2014) Sexual dysfunction and infertility as late effects of cancer treatment. EJC Suppl 12(1):41–53
Schover LR (2019) Sexual quality of life in men and women after cancer. Climacteric 22(6):553–557
Sadovsky R, Basson R, Krychman M, Morales AM, Schover L, Wang R, Incrocci L (2010) Cancer and sexual problems. J Sex Med 7(1 Pt 2):349–373
Schover LR, Yuan Y, Fellman BM, Odensky E, Lewis PE, Martinetti P (2013) Efficacy trial of an Internet-based intervention for cancer-related female sexual dysfunction. J Natl Compr Canc Netw 11(11):1389–1397
Flynn KE, Reese JB, Jeffery DD, Abernethy AP, Lin L, Shelby RA et al (2012) Patient experiences with communication about sex during and after treatment for cancer. Psychooncology 21(6):594–601
McCaughan E, Flannagan C, Parahoo K, Connaghan J, Maguire R, Steele M et al (2020) The tablet-based, engagement, assessment, support, and sign-posting (EASSi) tool for facilitating and structuring sexual well-being conversations in routine prostate cancer care: mixed-methods study. JMIR Cancer 6(2):e20137
Reese JB, Keefe FJ, Somers TJ, Abernethy AP (2010) Coping with sexual concerns after cancer: the use of flexible coping. Support Care Cancer 18(7):785–800
Ussher JM, Perz J, Gilbert E (2012) Changes to sexual well-being and intimacy after breast cancer. Cancer Nurs 35(6):456–465
Wang K, Ariello K, Choi M, Turner A, Wan BA, Yee C et al (2018) Sexual healthcare for cancer patients receiving palliative care: a narrative review. Ann Palliat Med 7(2):256–264
Winterling J, Lampic C, Wettergren L (2020) Fex-Talk: a short educational intervention intended to enhance nurses’ readiness to discuss fertility and sexuality with cancer patients. J Cancer Educ 35(3):538–544
Sporn NJ, Smith KB, Pirl WF, Lennes IT, Hyland KA, Park ER (2015) Sexual health communication between cancer survivors and providers: how frequently does it occur and which providers are preferred? Psychooncology 24(9):1167–1173
Cox A, Jenkins V, Catt S, Langridge C, Fallowfield L (2006) Information needs and experiences: an audit of UK cancer patients. Eur J Oncol Nurs 10(4):263–272
Taylor S, Harley C, Takeuchi E, Brown J, Velikova G (2013) Detecting and discussing sexual problems during chemotherapy for breast cancer. Breast J 19(5):566–567
Jonsdottir JI, Zoëga S, Saevarsdottir T, Sverrisdottir A, Thorsdottir T, Einarsson GV et al (2016) Changes in attitudes, practices and barriers among oncology health care professionals regarding sexual health care: outcomes from a 2-year educational intervention at a University Hospital. Eur J Oncol Nurs 21:24–30
Scanlon M, Blaes A, Geller M, Majhail NS, Lindgren B, Haddad T (2012) Patient satisfaction with physician discussions of treatment impact on fertility, menopause and sexual health among pre-menopausal women with cancer. J Cancer 3:217–225
Hautamäki K, Miettinen M, Kellokumpu-Lehtinen PL, Aalto P, Lehto J (2007) Opening communication with cancer patients about sexuality-related issues. Cancer Nurs 30(5):399–404
Krouwel EM, Albers LF, Nicolai MPJ, Putter H, Osanto S, Pelger RCM, Elzevier HW (2020) Discussing sexual health in the medical oncologist’s practice: exploring current practice and challenges. J Cancer Educ 35(6):1072–1088
Eeltink CM, Witte BI, Stringer J, Liptrott S, Babic A, Greenfield DM et al (2018) Health-care professionals’ perspective on discussing sexual issues in adult patients after haematopoietic cell transplantation. Bone Marrow Transplant 53(3):235–245
Hordern A (2008) Intimacy and sexuality after cancer: a critical review of the literature. Cancer Nurs 31(2):E9-17
Hordern AJ, Street AF (2007) Constructions of sexuality and intimacy after cancer: patient and health professional perspectives. Soc Sci Med 64(8):1704–1718
Reese JB, Lepore SJ, Daly MB, Handorf E, Sorice KA, Porter LS et al (2019) A brief intervention to enhance breast cancer clinicians’ communication about sexual health: Feasibility, acceptability, and preliminary outcomes. Psychooncology 28(4):872–879
Hordern AJ, Street AF (2007) Communicating about patient sexuality and intimacy after cancer: mismatched expectations and unmet needs. Med J Aust 186(5):224–227
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P et al (2018) The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf 34:285–291
Åkeflo L, Dunberger G, Elmerstig E, Skokic V, Steineck G, Bergmark K (2022) Sexual health and wellbeing among female pelvic cancer survivors following individualized interventions in a nurse-led clinic. Support Care Cancer 30(11):8981–8996
de Almeida NG, Knobf TM, de Oliveira MR, Salvetti MG, Oriá MOB, Fialho AVM (2020) A pilot intervention study to improve sexuality outcomes in breast cancer survivors. Asia Pac J Oncol Nurs 7(2):161–166
Bingham SL, Semple CJ, Flannagan C, Dunwoody L (2022) Enhancing healthcare professional-led sexual support in cancer care: acceptability and usability of an eLearning resource and its impact on attitudes towards providing sexual support. Psychooncology 31(9):1555–1563
Bokaie M, Firouzabadi O, Joulaee A (2022) The effectiveness of group problem-solving therapy on women’s sexual function and satisfaction after mastectomy surgery. BMC Womens Health 22(1):50
Bokaie M, Hejazi NS, Jafari M, Shabani M (2023) Effect of online solution-focused counseling on the sexual quality of life of women with a history of breast cancer: a clinical trial. BMC Womens Health 23(1):326
Chambers SK, Occhipinti S, Schover L, Nielsen L, Zajdlewicz L, Clutton S et al (2015) A randomised controlled trial of a couples-based sexuality intervention for men with localised prostate cancer and their female partners. Psychooncology 24(7):748–756
Chow KM, Chan CW, Chan JC, Choi KK, Siu KY (2014) A feasibility study of a psychoeducational intervention program for gynecological cancer patients. Eur J Oncol Nurs 18(4):385–392
Cullen K, Fergus K (2021) Acceptability of an online relational intimacy and sexual enhancement (iRISE) intervention after breast cancer. J Marital Fam Ther 47(2):515–532
Du J, Tian Y, Dan X, He Y (2020) The effect of empowerment education-based nursing intervention on the postoperative sexual function and depression state of cervical cancer patients of reproductive age. Int J Clin Exp Med 13(6):4052–4061
DuHamel K, Schuler T, Nelson C, Philip E, Temple L, Schover L et al (2016) The sexual health of female rectal and anal cancer survivors: results of a pilot randomized psycho-educational intervention trial. J Cancer Surviv 10(3):553–563
El-SayedSaboula N, Shahin MA (2015) Effectiveness of application of PLISSIT Counseling Model on Sexuality for Breast Cancer’s Women Undergoing Treatment. Am J Nurs Sci 4(4):218–230
Esmkhani M, Kharaghani R, Shakibazadeh E, Faghihzadeh S, Korte J, Khoei E (2021) Comparison of the Effects of the PLISSIT Model Versus the Sexual Health Model on Quality of Life Among Women with Breast Cancer. Sex Disabil 39:1–12
Faghani S, Ghaffari F (2016) Effects of sexual rehabilitation using the PLISSIT model on quality of sexual life and sexual functioning in post-mastectomy breast cancer survivors. Asian Pac J Cancer Prev 17(11):4845–4851
Fatehi S, Maasoumi R, Atashsokhan G, Hamidzadeh A, Janbabaei G, Mirrezaie SM (2019) The effects of psychosexual counseling on sexual quality of life and function in Iranian breast cancer survivors: a randomized controlled trial. Breast Cancer Res Treat 175(1):171–179
Jonsdottir JI, Vilhjalmsson R, Svavarsdottir EK (2021) The benefit of a couple-based intervention among women in active cancer treatment on sexual concerns: a quasi-experimental study. Cancer Nurs 44(6):E589–E599
Jonsdottir JI, Vilhjalmsson R, Svavarsdottir EK (2021) Effectiveness of a couple-based intervention on sexuality and intimacy among women in active cancer treatment: a quasi-experimental study. Eur J Oncol Nurs 52:101975
Keshavarz Z, Karimi E, Golezar S, Ozgoli G, Nasiri M (2021) The effect of PLISSIT based counseling model on sexual function, quality of life, and sexual distress in women surviving breast cancer: a single-group pretest-posttest trial. BMC Womens Health 21(1):417
Khoei EM, Kharaghani R, Shakibazadeh E, Faghihzadeh S, Aghajani N, Korte JE, Esmkhani M (2022) Sexual health outcomes of PLISSIT-based counseling versus grouped sexuality education among Iranian women with breast cancer: a randomized clinical trial. Sex Relatsh Ther 37(4):557–568
Li M, Chan CWH, Chan D, Li X, Zhang M, Zhang H et al (2023) The effectiveness of WeChat couple-based psychosocial support for gynaecological cancer: a randomised controlled trial. BJOG 130(6):599–609
Maughan K, Clarke C (2001) The effect of a clinical nurse specialist in gynaecological oncology on quality of life and sexuality. J Clin Nurs 10(2):221–229
McCaughan EM, Flannagan C, Parahoo K, Bingham SL, Brady N, Connaghan J et al (2021) Effects of a brief e-learning resource on sexual attitudes and beliefs of healthcare professionals working in prostate cancer care: a pilot study. Int J Environ Res Public Health 18(19):10045
Mohammadi Z, Maasoumi R, Vosoughi N, Eftekhar T, Soleimani M, Montazeri A (2022) The effect of the EX-PLISSIT model-based psychosexual counseling on improving sexual function and sexual quality of life in gynecologic cancer survivors: a randomized controlled clinical trial. Support Care Cancer 30(11):9117–9126
Olcer ZO, Oskay U (2022) Effects of the better model based counseling on sexuality of women with breast cancer. Int J Sex Health 34(1):41–54
Perz J, Ussher JM (2015) A randomized trial of a minimal intervention for sexual concerns after cancer: a comparison of self-help and professionally delivered modalities. BMC Cancer 15:629
Reese JB, Porter LS, Somers TJ, Keefe FJ (2012) Pilot feasibility study of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer. J Sex Marital Ther 38(5):402–417
Reese JB, Sorice KA, Pollard W, Handorf E, Beach MC, Daly MB et al (2021) Efficacy of a multimedia intervention in facilitating breast cancer patients’ clinical communication about sexual health: results of a randomized controlled trial. Psychooncology 30(5):681–690
Reese JB, Bober SL, Sorice KA, Handorf E, Chu CS, Middleton D et al (2023) Starting the Conversation: randomized pilot trial of an intervention to promote effective clinical communication about sexual health for gynecologic cancer survivors. J Cancer Surviv. https://doi.org/10.1007/s11764-022-01327-4
Roberts K, Chong T, Hollands E, Tan J, Mohan G, Cohen PA (2020) Screening for sexual health concerns in survivors of gynecological cancer. Support Care Cancer 28(2):599–605
HakamiShalamzai K, Asghari Pour N, Jamali J, TaghizadehKermani A, Babazadeh R (2022) The effect of sexual counseling based on BETTER and PLISSIT model on quality of sexual life in women with breast cancer after mastectomy. J Midwifery Reprod Health 10(4):3490–3498
Taleb FR, Sameh WM, Tolba KG, Hegazi SA, Altaheri AT (2023) The effect of nursing interventions on urinary, bowel and sexual dysfunction among post-radical prostatectomy patients. Int J Urol Nurs 17(1):70–77
Wang JMH, Hart M, Jain P, Fox C, Roelfsema L, de Dios DV et al (2022) Relationships, body image, and intimacy: a pilot to increase sexual health conversations between radiation therapists and cancer patients in Ontario. J Med Imaging Radiat Sci 53(2):264–272
Zhang L, Gu W, Zhang L, Miao R, Jing X, Zhi S et al (2022) The effects of a nurse-led couples intervention on marital quality of couples with gynecological cancer: a clinical randomized controlled trial. Gynecol Oncol 165(3):629–636
Jang SY (2021) Development and evaluation of a sexual health improvement program for women with gynecologic cancer. Asian Oncol Nurs 21(3):163–172
Chun N (2011) Effectiveness of PLISSIT model sexual program on female sexual function for women with gynecologic cancer. J Korean Acad Nurs 41(4):471–480
DAI Yunyun XY, CHEN Yangguang, LI Xiaomei, JIANG Qunfeng, GAO Yan (2019) Effect of PLISSIT intervention model on improving quality of sexual life and sexual function of cervical cancer patients. Chin Nurs Res 33(15):2586–9
Nho JH (2013) Effect of PLISSIT model sexual health enhancement program for women with gynecologic cancer and their husbands. J Korean Acad Nurs 43(5):681–689
Woo SJ, Lee ES, Kim HR (2017) Effectiveness of a sexual health program for men with rectal cancer resection. kjan. 29(3):225–234
Khoei EM, Kharaghani R, Shakibazadeh E, Faghihzadeh S, Aghajani N, Korte JE, Esmkhani M (2020) Sexual health outcomes of plissit-based counseling versus grouped sexuality education among iranian women with breast cancer: a randomized clinical trial. Sex Relat Ther 37(4):557–568
Chou YH, Chia-Rong Hsieh V, Chen X, Huang TY, Shieh SH (2020) Unmet supportive care needs of survival patients with breast cancer in different cancer stages and treatment phases. Taiwan J Obstet Gynecol 59(2):231–236
Bonacchi A, Di Miceli S, Lippi D, Muraca MG, Miccinesi G (2018) Unmet needs of Italian cancer patients in different stages of the disease and care process. Tumori 104(4):285–291
Eeltink C (2022) Sexuality in patients with hematological malignancies: from a patient, partner and health-care professional perspective. VU University Medical Center, Amsterdam
Ben Thabet J, Charfeddine F, Charfi N, Baati I, Zouari L, Zouari N, Maâlej M (2015) Sexuality of tunisian women: involvement of religion and culture. Encephale 41(2):144–150
Dune T, Ayika D, Thepsourinthone J, Mapedzahama V, Mengesha Z (2021) The role of culture and religion on sexual and reproductive health indicators and help-seeking attitudes amongst 1.5 generation migrants in Australia: a quantitative pilot study. Int J Environ Res Public Health 18(3):1341
Brooks LA, Bloomer MJ, Manias E (2019) Culturally sensitive communication at the end-of-life in the intensive care unit: a systematic review. Aust Crit Care 32(6):516–523
Funding
Financial support for this study was provided entirely by a grant from the Netherlands Organization for Health Research and Development (ZonMw) (Grant number: 80–84400-98–711). The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing and publishing the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arends, S.A.M., van Rossum, C.E., Eeltink, C.M. et al. Feasibility and effectiveness of communication tools for addressing intimacy and sexuality in patients with cancer: a systematic review. Support Care Cancer 32, 109 (2024). https://doi.org/10.1007/s00520-024-08308-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08308-6