Abstract
Purpose
This study explored colorectal and endometrial cancer survivors’ experiences of participation in a wearable intervention and the dimensions that influenced intervention engagement and physical activity behaviour change.
Methods
Semi-structured interviews (n= 23) were conducted with intervention participants (mean age 65.8 (SD ±7.1) and analysed using thematic analysis.
Results
Four main themes were identified: (i) commitment, (ii) accountability and monitoring, (iii) routine, (iv) Fitbit as health coach. Those that assigned a higher priority to PA were more likely to schedule PA and be successful in PA change. Those less successful presented more barriers to change and engaged in more incidental PA. The Fitbit acting as health coach was the active ingredient of the intervention.
Conclusions
Commitment evidenced through prioritising PA was the foundational dimension that influenced PA engagement. Interventions that foster commitment to PA through increasing the value and importance of PA would be worthwhile. Wearables holds great promise in PA promotion and harnessing the technique of discrepancy between behaviour and goals is likely a valuable behaviour change technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In 2020, ~19.3 million new cancers were recorded worldwide and almost 10 million deaths [1]. In relation to the population in the present study, colorectal cancer (CRC) represents the third most diagnosed cancer (10%) and the second leading cause of cancer death (9.4%), and endometrial cancer is the tenth most diagnosed cancer and comprises 3% of all cancer cases globally [1].
Increased physical activity (PA) post-diagnosis has been demonstrated to reduce both cancer-specific mortality and all-cause mortality in both CRC [2, 3] and endometrial cancer survivors [4]. Despite the increasing evidence that PA improves cancer outcomes, most survivors [5] fail to meet the aerobic guidelines of at least 150 min of moderate-intensity-PA/per week [6].
Despite the evidence supporting the benefits of PA for cancer survivors, most studies have focused on group differences, whilst giving little attention to individual differences or to understanding the ‘active ingredients’ of interventions. To improve our understanding of the efficacious components of interventions and understand the broader dimensions associated with PA behaviour change (PABC), qualitative approaches are worthwhile [7].
Qualitative approaches capture the range of influences on behaviour and offer an in-depth perspective on individuals’ perceptions and experiences that may help to identify the salient dimensions that influence intervention engagement and PABC.
There is a relative dearth of research concerning the experiences of cancer survivors following participation in a PA intervention [8,9,10]. Grimmett et al. (2020) found that enjoyable and highly valued PA was associated with PA maintenance following intervention [8]. Low motivation and a lack of enjoyment typified those who were insufficiently active [8]. Midtgaard et al. (2012) [10] found that goal-setting and prioritising PA typified exercise maintenance. Kokts-Porietis et al. (2019) [9] found the barriers of time, lack of motivation and bad weather affected adherence to a home-based intervention in breast cancer survivors. Feedback via the wearable-tracker was a facilitator of PA adherence. However, wearables were experienced by some as a source of judgement and failure when tracker-feedback did not correspond to perceptions of PA achievement [9].
The present study originates from the WATAAP (Wearable Activity Technology and Action-Planning) intervention [11] to ascertain whether Fitbits, in conjunction with action-planning, and was effective in increasing moderate-vigorous PA (MVPA) in endometrial and CRC survivors. The WATAAP intervention produced a significant increase in MVPA [11] that was maintained at follow-up [12]. The aim of the present study was to identify the active ingredients and salient dimensions that influenced PABC and intervention engagement amongst intervention participants.
Methods
Participants
Eligible participants were cancer survivors who participated in the WATAAP intervention [13]. The full eligibility criteria and intervention have been described previously [11, 13]. The 12-week intervention consisted of three components: (i) the provision of a Fitbit AltaTM; (ii) two 2-h group sessions to include PA recommendations, goal-setting, action-planning, coping-planning and self-monitoring; and (iii) a 20-min phone call (week 8) to provide support and assist with coping-planning.
Procedure
The current study conformed to the Standards for Reporting Qualitative Research [14] (see online Supplemental File 1). The St. John of God Hospital Ethics Committee approved this study (#1102). Participants indicated their willingness to participate in an interview to discuss their experiences of the intervention at their final assessment. A research assistant (RA) contacted participants who expressed willingness and an interview date was arranged. Participants provided written, informed consent prior to the interview and were informed that pseudonyms would be used in any reporting of the data.
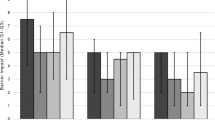
Semi-structured interviews (mean duration = 1.25 h) in May/June 2018 were conducted by two RAs (final year Psychology students) not involved in intervention delivery. The RAs were trained by the lead author (SH) who has a wealth of experience in qualitative data collection and analysis, and in PABC. Interviews took place within 3 months of trial completion at the participant’s home or at a mutually convenient location. An interview guide (Fig. 1) was utilised with questions concerning experience of the intervention, including the most and least useful aspects, and the factors influencing PABC. Interviews were digitally recorded and transcribed verbatim.
Data analysis
Data were analysed by the first author using reflexive thematic analysis [15] to generate themes. Analysis included deductive and inductive approaches; whilst a codebook was not adopted, and categories were not pre-determined, it is recognised that the interview guide focused primarily on experiences of the intervention and therefore analysis was not entirely inductive. Nevertheless, data was ‘open-coded’ to best represent the perceptions and experiences (in relation to the research aims) as conveyed by participants [16]. Thematic reflexive analysis involved several steps including (i) immersion and the careful reading of transcripts, (ii) attaching codes to salient text segments and (iii) the identification of themes at a broader level and examining whether codes may be combined to form an overarching theme. During these processes, inductive analysis was used to generate themes grounded in the data. Although it is recognised that data interpretation may be influenced by the researcher’s prior knowledge, an attempt was made to be open to new findings that may conflict with theory and previous research findings [17, 18]. The final step involved reviewing themes, cross-checking for overlap and finally defining and classifying themes. The analysis offered is one interpretation of the data and other interpretations are possible. Nevertheless, we aim to offer a credible and trustworthy interpretation that accurately captures the data. For example, we provide ‘thick description’ via the use of extensive quotations so that the reader can evaluate the interpretation [19].
Results
Twenty-three (70%) of invited participants completed an interview (mean age 65.8 ± 7.1 years). Table 1 displays participant demographics. The majority (n=18) were overweight (mean BMI of 28.8 ± 4.7). There were no significant differences in age, gender, cancer type, education, income or time since diagnosis between participants that entered the study compared to those who did not. Data analysis generated four main themes: commitment, accountability and monitoring, routine and Fitbit as health coachFootnote 1. Table 2 provides an overview of themes and their content.
Commitment
Commitment was underpinned by two sub-themes: prioritising PA and PA value. Participants who successfully increased MVPA were those who were committed to PA.
Prioritising PA
Commitment was expressed through prioritising health and PA: ‘I’m interested in my health…I’m invested’ (Graham, 67, > PA & MFootnote 2); and ‘exercise had become the most important thing to me, so I had to reorganise my life’ (Felicity, 67, > PA and M). Those who successfully increased PA prioritised PA: ‘I don’t accept busy…you deserve to be able to book a time in your diary [to do PA] to arrange your day around it’ (Lyn, 68, > PA & M). Kevin linked exercise with longevity, which underlined his commitment to PA: ‘I wasn’t prepared to die at 60…if I’ve got to do an-hour of exercise a day then that’s easy enough’ (Kevin, 60, > PA and M). Participants less successful did not prioritise PA: ‘I put being a good Samaritan ahead of walking 10,000 steps’ (Oscar, 68, > PA & DNM), and ‘I’m not prepared to give up the things I am doing…They are more fulfilling than walking around the block a couple of times’ (Leah, 71, < PA). Those who did not prioritise PA adopted a more casual approach concerning exercise achievement: ‘I try have a little goal everyday of what I am going to do…sometimes I do it and sometimes I don’t’ (Katherine, 62, < PA) and ‘It was sort of between 6 to 8000-steps. I didn’t push it…even if I got to 3500 or 4000 still felt pretty good’ (Joe, 72, <PA and increased at T3). Priority underpinned motivation: those who prioritised PA were more committed whilst those who did not expressed lower motivation and more barriers. For example, ‘I understand that it should be a priority to me, but I’m not motivated…I became too busy, then I got sick and then it was too hot’ (Mary, aged 77).
Valuing PA
Participants who valued PA appeared to be more committed: ‘I didn’t need convincing about the importance of exercise…I want to be able to do the things I want to do at the age of 70 and 80 and into my 90s’ (Andrea, 64, >PA and M). Conversely, participants that were sceptical of the guidelines or doubted the importance of PA valued PA less and were less committed to PA. For example, ‘The aim was to get to 10,000-steps…I thought “well why? Am I going to feel any fitter?”’ (Joe, 72, < PA) and ‘I’ve adopted the attitude of I am going reasonably well. I am not a star pupil, but I’m not the lowest in the class…I did 6000 and that’s good’ (Oscar, 68, > PA and DNM).
Accountability and monitoring
This theme included external accountability to the trial team for PA engagement, and more general monitoring which were perceived as helpful. Overall, participants that reported a reliance on external accountability for motivation tended to be less successful in PABC. For example, ‘It inspired me to get out because you’re accounting to someone about what you’re doing. I do need that’ (Leah, 71, <PA) and ‘I think some kind of monitoring…having some commitment and it’s an authority outside of you’ (Annette, 66, >PA but insufficiently active). The exception was Rebecca, who was one of the most successful participants yet almost entirely externally motivated: ‘I was motivated to do [PA] because it’s [trial co-ordinator’s] study…since I’ve finished the trial…there’s no motivation to keep exercising. It was the study keeping me motivated’ (Rebecca, 64, >PA and M).
Other participants reported that check-ins were motivational: ‘Maybe you’re more activated when someone is monitoring you’ (Christopher, 69, >PA and M) and ‘If I had a SMS or phone call to ask how it’s going or come have a review session that was a motivator’ (Graham, 67, >PA and M) or important for when encountering challenges: ‘I think the Fitbit, being aware of what I am doing, will be enough for me. Maybe if I knew there was a 3-monthly check-up would help me…when things go wrong like you get sick that’s when you need the motivation’ (Fiona, 67, >PA and M). Overall, most participants valued check-ins but most that successfully increased PA were not focused on external accountability for motivation.
Routine
Routine included sub-themes of incidental PA and influence of retirement on routine. Participants that established a PA routine were more likely to engage in and maintain adequate MVPA: ‘I do feel that if you have a set routine you are going to make more of an effort to do it’ (Julie, 67, > PA and M); ‘We have got a pattern now of walking every night’ (Andrea, 64, >PA and M). Rebecca referred to the importance of planned PA to achieve the step goal: ‘Having that routine was really important…250 steps per hour doesn’t get you to 10000 so I usually have a bigger walk 20-25 minutes early in the morning and then again’ (Rebecca, 64, >PA and M).
Incidental PA
Those who engaged in more incidental PA were less likely to increase MVPA: ‘I should do [PA] on a regular basis… but it’s disciplining myself’ (Katherine, 62, <PA); ‘I never managed to set the time I was going to do it in advance, so the activity tended to be incidental’ (Renee, 59, < PA). Annette also referred to more incidental PA: ‘When it comes to stuff like this, I will just on the spot do something so I will just run up the stairs…exercise has never been a huge thing for me’ (Annette, 66, >PA but insufficiently active).
Influence of retirement on routine
Participants recognised the importance of routine, yet many who were retired referred to a lack of daily structure: ‘I need to have a time… but I find it hard now I’m retired to be as patterned in anything’ (Rachel, 76, >PA and DNM). Further, in several cases, there was a resistance to planning and structure since retirement: ‘Maybe it has something to do with not wanting to be regimented, like you are at work…regimented by deadlines and goals…so I object to being regimented as there is no fun in it’ (Oscar, 68, >PA and DNM).
Fitbit as health coach
This theme summarises the finding that the Fitbit™ was the primary active ingredient to increase PA: ‘Well the Fitbit worked the best’ (Andrea, aged 64, >PA and M) and ‘The Fitbit was the motivator…it was kind of like everyday contact’ (Annette, 66 >PA and M) and Fitbit ‘was a motivator it was very powerful because it’s 24/7’ (Graham, 67, >PA and M). The Fitbit assisted in raising awareness of PA and sedentary behaviour through objective feedback and as a self-monitoring tool to achieve goals. The Fitbit did not work for all participants. Two participants that reduced MVPA had technical problems, for example ‘I couldn’t connect…the computer would say you need an update’ (Louisa, 76, <PA) and ‘My literacy is minimum…if I’d had a bit more training that would have helped’ (Mary, 77 <PA). Others referred to the unreliability of the Fitbit: ‘That was a major discourager…because I knew I could distort it by sweeping’ (Lyn, 68, >PA and M) or its inability to register PA:
If the Fitbit worked and I felt I was achieving something it might have encouraged me to do more exercise, but the Fitbit was a bigger disincentive…if you were doing short bursts, it would be very discouraging…it wasn’t recording even when I was making such an effort (Kath, 62, <PA)
Renee (59, <PA) recalled ‘I found that really frustrating…I would walk briskly (for) 7.5-minutes and it didn’t count…you get really annoyed when you do 9-minutes of vigorous activity, and it doesn’t count because it needs to be 10’. Fitbit as health coach contained three sub-themes: Prompts, self-monitoring and feedback, goal-setting and review.
Prompts
The Fitbit functioned as a prompt to decrease sedentary behaviour for most: ‘the bit most useful was the having to get up every 5-minutes…how easy it is to get 250-steps’ (Lyn, 68 >PA and M) and ‘Well the Fitbit was the tool to get your butt off the seat’ (Stephen, 44>PA and M).
Self-monitoring and feedback
The Fitbit provided self-monitoring and real-time feedback deemed motivational: ‘There were days where I wouldn’t look until 4pm and I would have only 3000 and I’d think I’ve got to go for an hour-long walk’ (Andrea, 64 >PA and M); ‘[The Fitbit] would say I had 8000 steps, so I would go around the block just to get 10000’ (Julie, 67 >PA and M). Participants who were more successful also reviewed their progress: ‘Fitbit would send you the weekly report and how you compared to last week. I looked at that and thought oh well this is what I’ve got to do’ (Julie, 67 >PA and M).
It is important to note that self-monitoring was the primary technique used by participants and that few engaged in or were willing to do formal action-planning despite action-planning being a core component of the intervention: ‘Action-planning doesn’t really work for me, I’m a list person…it has to something really simple and measurable…a tick on the calendar’ (Andrea, 64 >PA and M.). Most preferred to keep a diary as a self-monitoring tool: ‘I keep a diary…I would always write in my diary what I had done…walk lake, walk beach’ (Rachel, 76 >PA and DNM).
Goal-setting and review
For many, the Fitbit assisted with goal-setting: ‘I had a goal with the Fitbit I was able to keep going and maintain’ (Abigail, 67). Many set themselves a step goal ‘I just went with the 10000-steps’ (Rebecca, 64, >PA and M) or active minutes goal ‘I kept the goal of 150- minutes….my own goal was 210’ (Andrea, 64 >PA and M), and would review progress with the Fitbit: ‘I would do 3 or 4kms and it would only get about 4000-steps, and I thought yuck that’s not much so I would have to pick it up’ (Julie, 67, >PA and M) and ‘I always made the 150mins and nearly always met the 210’ (Andrea, 64, >PA and M). Those who increased MVPA assessed goal progress: ‘See yesterday was very light and I’ll compensate for that’ (Graham, 67 >PA and M). Conversely, those who were less successful set less challenging goals in order to feel a sense of achievement: ‘I set my goal low so I could always achieve, I set it at 7500-steps’ (Renee, 59 <PA) and ‘I looked at it and said I did 6000-steps today that’s terrific and if I only did 3500 that’s okay’ (Oscar, 68 >PA and DNM).
Discussion
This study provides an in-depth understanding of the salient dimensions that influence PABC amongst colorectal and endometrial cancer survivors in addition to the successful ingredients of the intervention. Key themes generated explained the active ingredients of the intervention (i.e., Fitbit as health coach) and the dimensions associated with PABC more generally: commitment, accountability/monitoring and routine.
The study found clear differences in priorities between participants that successfully increased and maintained MVPA compared to those that did not. A commitment to PA appeared to be the foundation to successful PABC. Those that did not prioritise PA expressed lower motivation and presented more barriers to exercise. Similar findings were identified in a study on successful PA maintenance, where cancer survivors prioritised PA over other obligations [10]. Grimmett et al. (2020) also found that health benefits of PA were highly valued amongst gastrointestinal cancer survivors who had maintained PA following intervention [8]. In the present study, participants that deemed PA as essential for health were more successful in PABC, whereas those that were sceptical of the guidelines or doubted the importance of PA valued PA less and were less committed to PA. Similar findings concerning scepticism of health guidelines amongst cancer survivors have been recognised previously [20]. Consistent with previous research, low motivation and low priority typified those that did not increase MVPA during the intervention [8, 9, 20]. However, contrary to previous findings [8], a lack of enjoyment did not typify those that did not increase MVPA, nor did enjoyment play an obvious role in exercise maintenance. Previous research has similarly found that instrumental attitude, but not affective attitude, predicted PA intention in cancer survivors [21, 22] whilst other research supports relations between affective attitudes, and PA participation [23, 24].
Participants that developed a PA routine appeared more likely to increase MVPA consistent with previous research [8]. This is unsurprising, since those who are more committed to exercise are more likely to schedule PA. Scheduling exercise has been identified as a facilitator of PA engagement amongst cancer survivors [25]. Conversely, participants who engaged in more incidental PA were less likely to increase MVPA. This is a novel finding and indicates that a focus on accumulating steps is unlikely to be sufficient to achieve the PA guidelines.
A further novel finding was the resistance to structure and planning, related to retirement and a desire for less structure where formal scheduling was rejected as a reminder of employment. Although successful participants developed a PA routine, most did not engage in formal action-planning, despite it being a core intervention component. Instead, participants used a combination of goal-setting, self-monitoring, Fitbit-derived feedback and review, to evaluate progress and change behaviour accordingly. Self-monitoring was the primary technique used to sustain motivation and PA.
Reviews also support the role of self-monitoring for PABC [26,27,28] in addition to goal-setting [27, 28] and action-planning [26, 29, 30] in cancer survivors. In the present study, commitment led to goal-setting, which was kept in check through daily self-monitoring and review of behaviour. The Fitbit did not work for all participants; some experienced technical problems and others were demotivated due to its inability to accurately reflect users’ PA. Similar findings of cancer survivors rejecting wearables due to discrepancies between perceived PA and data provided by the device have been reported [9].
Finally, participants reliant on external accountability tended to be less successful in PABC. The desire for external accountability and monitoring to produce accountability in survivors has been reported elsewhere [9, 31]. Check-ins were valued, although most who were successful were not focused on external accountability for motivation.
Study limitations
Our study recruited participants in Western Australia; therefore, findings may not be generalizable. The potential for selection bias and recall bias are further limitations. Strengths of the study include the high response rate, the focus on MVPA, lengthy interviews and capture of participants with varying PABC success.
Conclusion
To our knowledge, this is the first study to comprehensively explore endometrial and CRC survivors’ experiences of a low-intensity intervention and to identify the salient dimensions that influenced PABC. Commitment was the foundational dimension that influenced PABC. Those who assigned a higher priority to PA were more likely to schedule PA and be successful. Those less successful lacked motivation and tended to engage in more incidental PA. Interventions that enhance commitment through increasing the value of PA would be worthwhile. Wearables hold promise in PA promotion and harnessing the technique of discrepancy between behaviour and goals is likely a valuable technique. Given the disappointment associated with devices failing to register short bouts of MVPA, future wearable would do well to ensure that all MVPA is captured.
Notes
Overall, 12 (52%) increased MVPA and maintained PA at T3 and one increased MVPA during the intervention but did not maintain PA. Seven participants (30%) did not change their MVPA during the intervention and three (13%) reduced MVPA over the course of the intervention but remained physically active.
The identifiers following each quote include pseudonym, age, symbols (> or <) to denote increased or decreased MVPA (derived from the Actigraph GTX9 accelerometer) from T1 to T2, and M or DNM to denote maintained or did not maintain MVPA at T3 (24 weeks).
References
Sung HJ, Ferlay RL, Siegal R (2021) Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71(3):209–249
Friedenreich CM, Stone CR, Cheung WY, Hayes SC (2019) Physical activity and mortality in cancer survivors: a systematic review and meta-analysis. JNCI Cancer Spectr. https://doi.org/10.1093/jncics/pkz080
Schmid D, Leitzmann MF (2014) Association between physical activity and mortality among breast cancer and colorectal cancer survivors: a systematic review and meta-analysis. Ann Oncol 25(7):1293–1311
Friedenreich CM, Cook LS, Wang Q, Kokts-Porietis RL, McNeil J, Ryder-Burbidge C, Courneya KS (2020) Prospective cohort study of pre- and postdiagnosis physical activity and endometrial cancer survival. J Clin Oncol 38(34):4107–4117. https://doi.org/10.1200/JCO.20.01336
Arem H, Mama SK, Duan X, Rowland JH, Bellizzi KM, Ehlers DK (2020) Prevalence of healthy behaviors among cancer survivors in the United States: how far have we come? Cancer Epidemiol Biomark Prev 29:1179–1187. https://doi.org/10.1158/1055-9965.EPI-19-1318
Campbell KL, Winters-Stone KM, Wiskemann JM, May AM, Schwartz A, Courneya KS, Zucker DS et al (2019) Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc 51(11):2375–2390
Hardcastle SJ, Hagger MS (2015) Psychographic profiling for effective health behavior change interventions. Front Psychol 6:1988. https://doi.org/10.3389/fpsyg.2015.01988
Grimmett C, Foster C, Bradbury K, Lally P, May CR, Myall M, Pinto B, Corbett T (2020) Exploring maintenance of physical activity behaviour change among people living with and beyond gastrointestinal cancer: a cross-sectional qualitative study and typology. BMJ Open 10:e037136. https://doi.org/10.1136/bmjopen-2020-037136
Kokts-Porietis RL, Stone CR, Friedenreich CM, Froese A, McDonough M, McNeil J (2019) Breast cancer survivors’ perspectives on a home-based physical activity intervention utilizing wearable technology. Support Care Cancer 27(8):2885–2892. https://doi.org/10.1007/s00520-018-4581-7
Midtgaard JK, Rossell JF, Christensen J, Uth L, Rørth M (2012) Demonstration and manifestation of self-determination and illness resistance—a qualitative study of long-term maintenance of physical activity in posttreatment cancer survivors. Support Care Cancer 20(9):1999–2008. https://doi.org/10.1007/s00520-011-1304-8
Maxwell-Smith C, Hince D, Cohen PA, Bulsara M, Boyle T, Platell C, Tan P et al (2019) A randomized controlled trial of WATAAP to promote physical activity in colorectal and endometrial cancer survivors. Psycho-Oncology 28(7):1420–1429. https://doi.org/10.1002/pon.5090
Hardcastle SJ, Maxwell-Smith C, Hince D, Bulsara M, Boyle T, Tan P, Levitt M et al (2021) The wearable activity technology and action-planning trial in cancer survivors: Physical activity maintenance post-intervention. J Sci Med Sport 24(9):902–907. https://doi.org/10.1016/j.jsams.2021.04.004
Maxwell-Smith C, Cohen PA, Platell C, Tan P, Levitt M, Salama P, Makin G et al (2018) Wearable activity technology and action-planning (WATAAP) to promote physical activity in cancer survivors: randomised controlled trial protocol. Int J Clin Health Psychol 18(2):124–132. https://doi.org/10.1016/j.ijchp.2018.03.003
O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA (2014) Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 89(9):1245–1251. https://doi.org/10.1097/ACM.0000000000000388
Braun V, Clarke V (2019) Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health 11(4):589–597. https://doi.org/10.1080/2159676X.2019.1628806
Braun V, Clarke V (2013) Successful qualitative research: a practical guide for beginners. Sage Publications, Thousand Oaks
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3(2):77–101. https://doi.org/10.1191/1478088706qp063oa
Hardcastle SJ, Caraher M (2021) The role of foodbanks in the context of food insecurity: experiences and eating behaviours amongst users. Appetite 1(163):105208. https://doi.org/10.1016/j.appet.2021.105208
Hardcastle SJ, Hagger MS (2011) You can't do it on your own: experiences of a motivational interviewing intervention on physical activity and dietary behaviour. Psychol Sport Exerc 12(3):314–323. https://doi.org/10.1016/j.psychsport.2011.01.001
Maxwell-Smith C, Zeps N, Hagger MS, Platell C, Hardcastle SJ (2017) Barriers to physical activity participation in colorectal cancer survivors at high risk of cardiovascular disease. Psycho-Oncology 26(6):808–814. https://doi.org/10.1002/pon.4234
Trinh L, Plotnikoff RC, Ryan E, North S, Courneya KS (2012) Correlates of physical activity in a population-based sample of kidney cancer survivors: an application of the theory of planned behavior. Int J Behav Nutr Phys Act 6(9):96. https://doi.org/10.1186/1479-5868-9-96
Maxwell-Smith C, Hagger MS, Kane R, Cohen PA, Tan P, Platell C et al (2021) Psychological correlates of physical activity and exercise preferences in metropolitan and nonmetropolitan cancer survivors. Psycho-Oncology 30(2):221–230. https://doi.org/10.1002/pon.555
Courneya KS, Reid RD, Friedenreich CM, Gelmon K, Proulx C, Vallance JK, McKenzie DC, Segal RJ (2008) Understanding breast cancer patients’ preference for two types of exercise training during chemotherapy in an unblinded randomized controlled trial. Int J Behav Nutr Phys Act 27(5):52. https://doi.org/10.1186/1479-5868-5-52
Rhodes RE, Kates A (2019) Can the affective response to exercise predict future motives and physical activity behavior? A systematic review of published evidence. Ann Behav Med 49(5):715–731. https://doi.org/10.1007/s12160-015-9704-5
Elshahat SC, Treanor, and Donnelly M (2021) Factors influencing physical activity participation among people living with or beyond cancer: a systematic scoping review. Int J Behav Nutr Phys Act 18(50). https://doi.org/10.1186/s12966-021-01116-9.
Meyer-Schwickerath CC, Morawietz FT, Baumann G, Wiskemann J (2021) Efficacy of face-to-face behavior change counselinyg interventions on physical activity behavior in cancer survivors - a systematic review and meta-analysis. Disabil Rehabil 14:1–16. https://doi.org/10.1080/09638288.2021.1938247
Mbous YP, Patel J, Kelly KM (2020) A systematic review and meta-analysis of physical activity interventions among colorectal cancer survivors. Transl Behav Med 10(5):1134–1143. https://doi.org/10.1093/tbm/ibz176
Hailey V, Rojas-Garcia A, Kassianos AP (2022) A systematic review of behaviour change techniques used in interventions to increase physical activity among breast cancer survivors. Breast Cancer 29:193–208. https://doi.org/10.1007/s12282-021-01323-z
Grimmett C, Corbett T, Brunet J, Shepherd J, Pinto BM, May CR, Foster C (2019) Systematic review and meta-analysis of maintenance of physical activity behaviour change in cancer survivors. Int J Behav Nutr Phys Act 16(1):37. https://doi.org/10.1186/s12966-019-0787-4
Ester M, Eisele M, Wurz A, McDonough MH, McNeely M, Culos-Reed N (2021) Current evidence and directions for future research in eHealth physical activity interventions for adults affected by cancer: systematic review. JMIR Cancer 7(3):e28852. https://doi.org/10.2196/28852
Dennett AM, Peiris CL, Taylor NF, Reed MS, Shields N (2019) A good stepping stone to normality’: a qualitative study of cancer survivors’ experiences of an exercise-based rehabilitation program. Support Care Cancer 27(5):1729–1736. https://doi.org/10.1007/s00520-018-4429-1
Acknowledgements
We thank the study participants for their time and contribution.
Author information
Authors and Affiliations
Contributions
Sarah Hardcastle conceived the original idea and Chloe Maxwell-Smith helped supervise the project. Emma Douglass and Bree Wilson collected and transcribed the data. Sarah Hardcastle analysed the data and wrote the manuscript with support from all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the St John of God Hospital Subiaco Ethics Committee (Reference #1102).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the interview data using pseudonyms.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 18 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hardcastle, S.J., Douglass, E., Wilson, B. et al. Experiences and facilitators of physical activity engagement amongst colorectal and endometrial cancer survivors: the Wearable Activity Technology and Action-Planning (WATAAP) trial. Support Care Cancer 31, 662 (2023). https://doi.org/10.1007/s00520-023-08137-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-08137-z