Abstract
Purpose
To examine children’s experiences of chemotherapy-induced cognitive impairment––colloquially “chemobrain”––and the impact on children’s social, academic, and daily living skills via a qualitative systematic review. Experiencing chemotherapy as a child, when the brain is still developing, may cause lifelong detriment to survivors’ lives. There is a significant gap in understanding their lived experience, including the self-identified barriers that children face following treatment. Such a gap can only be fully bridged by listening to the child’s own voice and/or parent proxy report through an exploration of the qualitative research literature.
Methods
A search of MEDLINE, Embase, PsycINFO, and CINAHL databases was conducted. Inclusion criteria were qualitative studies with a focus on children (0–18 years) during and/or following chemotherapy treatment and explored children’s experiences of chemobrain.
Results
Two synthesized findings were identified from six studies. (1) Chemobrain has an academic and psychosocial impact, which may not be understood by education providers. (2) Children and their parents have concerns about their reintegration and adaptation to school, social lives, and their future selves as independent members of society. Children’s experiences primarily related to changes in their academic and social functioning.
Conclusion
This review highlights two important considerations: (1) the lived experiences of pediatric childhood cancer survivors guiding where future interventions should be targeted, and (2) a need to perform more qualitative research studies in this area, as well as to improve the quality of reporting among the existing literature, given that this is a current gap in the field.
Similar content being viewed by others
Background
Each year, an estimated 400,000 children and adolescents between the ages of 0 and 19 develop cancer worldwide [1]. Of these, the most common diagnoses include leukemias, brain tumors, and other central nervous system (CNS) cancers [2]. Age is a strong influencing factor, with the highest incidence of cancer and death in children aged 1–4 years old [3]. Standard therapies include the use of chemotherapy, surgery, and/or radiotherapy [1].
Advances in cancer treatment and supportive care have resulted in vast improvements in survival rates over the past 50 years in children with a cancer diagnosis, with a current event-free 5-year relative survival rate of 85–90% [4,5,6]. As a result, issues of survivorship are more prominent, with approximately 60–90% of childhood cancer survivors developing one or more chronic conditions affecting cardiovascular, renal, ocular, gastrointestinal, pulmonary, endocrine, musculoskeletal, neurological, immune, psychological, and reproductive systems—many of which are disabling conditions [7]. It is therefore evident that cancer, and its treatments, are different in children compared to adults, likely due to the disruption it causes to the normal development of a child’s body and brain [8]. Of particular note is that 40–60% of pediatric cancer survivors experience significant neurocognitive deficits with respect to attention, executive functioning, processing speed, visual processing, and visual motor function [6, 9,10,11]. These neurocognitive deficits generally predominate when combined polychemotherapy and radiation has been used in treatment [12]. Although childhood cancer patients being treated for CNS tumors with radiotherapy, particularly whole-brain irradiation, are at the greatest risk of developing long-term neurocognitive impairments, there is evidence that patients treated with chemotherapy-only are also at significant risk [13,14,15]. It is important to note that cognitive impairment can also be present prior to commencing any treatments, with a diagnosis of cancer itself resulting in impaired cognition in 20–50% of patients [16,17,18,19].
The presence of cognitive impairment following chemotherapy treatment specifically is known as chemotherapy-induced cognitive impairment (CICI)––colloquially known as “chemobrain.” This debilitating condition is characterized by impairments in verbal, visual, and working memory and facets of executive functioning, such as motivation, attention, and processing speed [16, 20]. A study conducted by the Swiss Childhood Cancer Register demonstrated that childhood cancer survivors (n = 644) are prone to developing issues with memory, concentration, and processing speed versus their healthy siblings (n = 247) following cancer and its treatment(s) across diagnostic and treatment groupings [21]. The implications of these impairments typically manifest in children at school through difficulty paying attention, incomplete assignments, additional time needed to complete work, struggling to keep up with the workload, and difficulties retaining and recalling information [22]. Developmental trajectories for these children are slower than the age-expected levels, with impacts evident in their IQ and academic performance over time [22]. This is particularly concerning considering potential long-term ramifications, with many survivors of childhood cancer achieving lower levels of educational attainment, experiencing a higher risk of job discrimination, and lower levels of career success over their lifetime [23,24,25,26,27]. To date, clinical studies examining CICI have focused primarily on adult female breast cancer patients [20]. As such, there is an under-representation of other populations of particular concern, including children.
While the prevalence and presentation of chemobrain have been previously explored in the literature, there is currently a significant gap in understanding the lived experience of childhood cancer survivors, including the self-identified burden of treatment and barriers that children face during and following treatment. Such a gap can only be fully bridged by listening to the child’s own voice through an exploration of the qualitative research literature. Listening to the child’s own voice allows for candid insights into experiences that they deem important and the subsequent impact on their lives, prioritizing where treatment and supportive care should be implemented to achieve the greatest positive effect for childhood cancer survivors. Oftentimes, it is not plausible or ethical for children to provide self-report as they may be too young, often seen in childhood cancer populations, where the highest incidence of cancer is in those under 4 years of age, or they may be cognitively or physically impaired [3, 28]. As such, parent proxy reports may have utility for shedding light on their child’s experience when the child’s own voice was not possible to obtain. At present, the lived experience of childhood cancer survivors is underrepresented in the literature. A preliminary search yielded no systematic reviews that specifically examined the experiences of children with chemobrain, either in their own voice or through parent proxy reports. This is important, as systematic reviews are considered the most reliable sources of evidence to guide the development of clinical practice guidelines; however, traditionally, systematic reviews limit their consideration only to the quantitative literature, losing a critical component of survivors’ perceptions of impact [29, 30].
To address this gap, this review explores the experiences of pediatric populations that have received chemotherapy for cancer treatment. Specifically, the impact of chemobrain on children’s social, academic, and daily living skills is considered through the voice of the child and/or their parent. It is hoped that a greater understanding of disease burden, from a patient-centered perspective, will inform survivorship frameworks and decisions on the need for and resourcing of rehabilitation, as well as other support strategies.
Review question
What are the experiences of children who have chemobrain, and what is the impact of chemobrain on children’s social, academic, and daily living skills as described in either their own words or through parent proxy report?
Inclusion criteria
Participants
Studies were eligible for inclusion if they reported on the experiences of children (0–18 years) who were receiving, or had finished, chemotherapy treatment (including those who received adjuvant therapy, such as radiotherapy) and discussed experiences of cognitive impairment, commonly known as chemobrain. Studies with partial inclusion of the age range were screened at full-text to assess whether data could be extrapolated by age. There were no restrictions on time from cessation of treatment. Participants over the age of 18 years who underwent chemotherapy as children/adolescents were not eligible to minimize recall bias [31].
Phenomena of interest
Studies that explored the impact of chemobrain on social, academic, and/or daily living skills heard through the child’s voice, or via parent/guardian proxy reports, were eligible for inclusion. If a study presented child and parent voices, it was included if both voices were distinctly identified. If the voices were combined or not adequately identified, the study was excluded.
Context
This review considered studies that included primary and tertiary health care settings (e.g., hospital and community-based settings), their home, and education settings. Studies were not restricted by geographic location if they were English-language publications.
Types of studies
All peer-reviewed studies using qualitative methodology were eligible for inclusion. This included data from studies that used methods such as interviews, surveys, and focus groups. Theses and dissertations were included. Other gray literature was excluded.
Methods
This review was conducted using JBI guidance for qualitative systematic reviews and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines [32, 33]. This review was registered with PROSPERO (PROSPERO Registration CRD42021240573) and conducted in accordance with an a priori protocol [34].
Search strategy
An initial search was conducted to identify appropriate key terms, index terms, and controlled vocabulary, such as MeSH terms performed in MEDLINE via PubMed. Identified keywords included “childhood cancer survivor(s),” “pediatric,” “quality of life,” and facets of cognitive impairment such as “psychological adaptation,” “interpersonal relations,” “social skills,” and “academic performance” to broadly encompass all potential experiences. The search strategy was developed in conjunction with a medical information specialist to ensure appropriate terms and a robust search methodology. MEDLINE via Ovid, Embase, PsycINFO via Ovid, CINAHL via EBSCOhost, and ProQuest Dissertations and Theses were searched from database inception to identify studies for title and abstract screening (Online Resource 1). No date restrictions were applied to the searches. Only English-language publications were included due to a lack of ready access to translators.
Study selection
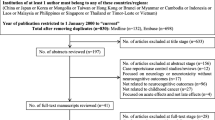
Following searches of included databases, all citations were collated and uploaded to EndNote X9 (Clarivate Analytics, PA, USA) and imported into Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia), where duplicates were removed. Where conflicts arose, a third independent reviewer was consulted (DP). The title and abstract and full-text screening process was piloted by assigning a random subset of studies (10 studies per reviewer) to two independent reviewers (IS and ALW). These reviewers assessed whether to include or exclude these studies with reasoning. To ensure consistency in the study selection, a consensus of 90% between the reviewers was attained prior to undertaking full screening. Each study was screened based on the title and abstract against the inclusion and exclusion criteria by four independent reviewers (IS, OJH, RPG, ALW). The reference lists of all included studies were screened for additional studies. Full-text and supplementary materials were imported into the JBI System for the Unified Management, Assessment, and Review of Information (JBI SUMARI; JBI, Adelaide, Australia) [35]. Full-text studies were assessed against the inclusion and exclusion criteria by four independent reviewers (IS, OJH, RPG, ALW), with a fifth reviewer being consulted where there was any disagreement (DP). Reasons for exclusion were recorded and presented. An updated search was conducted in 2022, a year from the original search. The results of both searches are reported in full, presented in a PRISMA flow diagram [33] (Fig. 1).
PRISMA 2020 flow diagram for new systematic reviews which included searches of databases, registers, and other sources [33]
Assessment of methodological quality
Studies eligible for inclusion were critically appraised for their methodological quality using the standard JBI critical appraisal checklist for qualitative research tool in JBI SUMARI [32] (Online Resource 5). Each study was appraised against 10 predefined questions for which answers “yes,” “unclear,” or “no” were applicable to determine overall quality. Two independent reviewers (IS AND ALW) conducted the critical appraisal blinded to each other’s assessment. Any conflicts that arose were resolved via discussion or consultation with a third independent reviewer (DP). All studies, regardless of the results of their methodological quality, underwent data extraction and synthesis.
Data extraction
JBI’s standardized extraction tool was used for the six included studies (Online Resource 2) [32]. Two independent reviewers (IS and ALW) conducted data extraction. Any conflicts that arose were resolved via discussion or consultation with a third independent reviewer (DP). Extracted data included citation details, study design, country of origin, country where research was conducted, setting/context, time or time frame of data collection (if applicable), population characteristics (based on inclusion/exclusion criteria), methodology, and study outcomes.
Each finding and associated illustrations was graded for credibility (unequivocal, credible, or not supported) using the ConQual process [36]. Supplementary materials and appendices were referred to where necessary.
Data synthesis
A meta-aggregative approach was utilized to synthesize the results in JBI SUMARI [37]. This approach involves collating similar findings to generate general statements that describe that aggregation by categorizing them based on similarity of meaning. These categories were then subjected to a synthesis to produce a single comprehensive set of synthesized findings. Only findings that achieved an unequivocal (U) or credible (C) grading were included in aggregation; unsupported findings are presented separately (Online Resource 3).
Assessing confidence in the findings
Synthesized findings obtained from data synthesis were subject to the ConQual approach to determine confidence in the findings [36]. The Summary of Findings table including the review title, population, phenomena of interest, and context is presented. Each synthesized finding is presented, along with the evidence informing it, scores of dependability and credibility, the overall ConQual score, and relevant comments informing this process.
Results
Study inclusion
The original database search, and an updated search conducted a year later, identified a total of 10,117 studies. A total of 7063 studies were excluded based on title and abstract screening, with 773 remaining for full-text assessment. During the full-text screening, 699 studies were excluded due to duplicates, ineligible phenomena of interest, ineligible participant characteristics, and ineligible study type. In total, six studies were included in this review.
Details of the identification process are described in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) flow chart [33] (Fig. 1).
Study characteristics
For the six studies that met the eligibility criteria, publication dates ranged from 1999 to 2021. Data were provided from the USA (n = 2), Belgium (n = 1), Taiwan (n = 1), Canada (n = 1), and the UK (n = 1). Included studies employed semi-structured interviews (n = 5) and clinical interview (n = 1) methodology. Eighty percent of studies did not report a philosophical perspective, and 50% did not report the qualitative methodology. Both Choquette and Vance reported an interpretive philosophical perspective, while Choquette, Vance, and Chen reported descriptive methodology [38,39,40]. The characteristics of the included studies are reported in Online Resource 4.
Participant characteristics
Participant characteristics from the included studies included age at diagnosis (8–16 years), age at study inclusion (7–18 years), and a range of 5.6 to 11.9 (mean) months since the cessation of treatment. Medical diagnoses included leukemias (acute lymphoblastic leukemia and acute myeloid leukemia), lymphomas (Hodgkin and non-Hodgkin), sarcoma (Ewing and osteosarcoma), testicular, and brain tumors (medulloblastoma), treated with a combination of chemotherapy, radiotherapy, bone marrow transplant, and/or surgical procedures. Seven participants attended school, with one of these participants additionally receiving special education [38,39,40,41,42]. One participant attended school but was previously home-schooled [43]. One participant was home-schooled but previously attended school [39]. Where specific participants were not identified, general characteristics were reported [38, 41]. Detailed characteristics of participants included in each study are reported in Table 1.X`X`XXXXXX`[Edit]
Critical appraisal results
Each study (n = 6) was critically appraised for methodological quality using the standard JBI critical appraisal checklist for qualitative research tool in JBI SUMARI [37] (Online Resource 5). Of the studies, half had issues with congruity with the research methodology, research question/objective, methods used to collect data, representation and analysis of data, and the interpretation of the results. Four studies had issues with congruity between the stated philosophical perspective and research methodology and had no statement locating the researcher culturally or theoretically. One study did not adequately represent the participant’s voice(s). All studies reported ethics approval and presented logical conclusions drawn from the analysis, or interpretation, of their data (Online Resource 5).
Findings of the review
The findings of this review and meta-aggregation are reported in full in Online Resource 6 and 7. The final synthesized findings were graded according to the ConQual Summary of Findings, as shown in Table 2.
Synthesized finding 1: Chemobrain has an academic and psychosocial impact which may not be understood by education providers
Children’s experiences with chemobrain manifest as problems with memory, attention, comprehension, and feeling “mentally slow” with an emphasis on functioning in the school setting [38,39,40, 42, 43]. Children found it difficult to transition back to school and struggled with academic performance [40, 42]. Children were acutely aware of their reduced abilities and compared themselves to peers who were performing well, causing mental distress [39, 41]. Only one child was able to get “statemented” (given a statement of special needs) to be able to access support [43]. As such, resources appear to be lacking, with minimal support or education provided to aid struggling children (Table 3).
Synthesized finding 2: Children and adolescents and their parents have concerns about their reintegration and adaption to school, social life, and their future selves as independent members of society
Parents express concern regarding their child’s future, specifically their level of independence and ability to self-care [39]. While some children recognize and accept the changes to their abilities and adapt by reducing their workload or finding other ways to excel non-academically, other children can develop debilitating issues like social phobia without the necessary support [39, 42]. Many children additionally struggle with fundamental daily living skills such as hygiene, feeding themselves, and handling money, posing a significant barrier to their future employability, livelihood, and quality of life [39] (Table 3).
Discussion
To our knowledge, this is the first systematic review of qualitative evidence exploring how chemobrain affects a child’s social, academic, and daily living skills from the perspective of the child and/or parent proxy report. Our primary finding is that children who have had childhood cancer, and have subsequently suffered cognitive changes (chemobrain), find their lives impacted, on a personal level, interpersonal level, and academic level. Their parents express concern for their future as a result.
Chemobrain affected children’s memory, concentration, attention, and learning, resulting in poor academic performance. Some children demonstrated more specific attentional deficits. Children found it difficult to get back to school and catch up on missed work, could not remember school material, could not understand the teacher, felt mentally slow, took a long time to complete work, and had poor performance in tests. Changes in their functioning made children feel different from their peers, who could keep up with the workload or extracurricular activities. Indeed, the presentation of these symptoms is consistent with what has been previously demonstrated in this population with quantitative research studies highlighting that childhood cancer survivors struggle with memory, concentration, and attention interfering with their schooling, as demonstrated by lower academic achievement, incomplete assignments, struggling to keep up with the workload, and difficulties in retaining and recalling information they learn [21, 22]. Long-term, these issues manifest as lower levels of educational attainment, higher risk of job discrimination, and lower levels of career success over their lifetime [23,24,25,26,27].
Despite evidence of these challenges voiced by the children in the included studies, it is difficult to tease apart whether these difficulties are due to chemobrain specifically or other factors associated with treatment. Time spent away from school due to health may result in significant impacts on a child’s academic performance and abilities upon returning to school following treatment. Children who miss school for prolonged periods of time due to chronic health issues are three times more likely to have developmental and behavioral conditions than their peers [44]. Additionally, studies have demonstrated that children who miss more days of school report lower academic performance and achievement [45]. Conversely, the physical side effects of cancer and its treatment can also impact cognitive performance, particularly fatigue. Cancer-related fatigue (CRF), in particular, is a condition associated with diminished concentration, attention, motivation, and work-related cognitive limitations in adult breast cancer patients and is associated with decreased quality of life long-term [46, 47].
In addition to physical and cognitive ramifications of cancer and its treatment, psychological effects are also more prevalent in this population, with symptoms of anxiety, depression, post-traumatic stress disorder, and low self-esteem potentially exacerbating other negative experiences, such as poor performance at school, difficulty attaining employment, and deficits in socializing [24, 25, 27]. Evident in this review, some children would compare their own performance to how well their peers were doing and would feel upset. Children were confronted with these changes upon returning to school. Alongside academic changes, children’s social landscape also changed, with some children withdrawing. In contrast, some children adapted to their new way of being and confronted these changes. One child took up art as an alternative way to excel at school without excelling in academic performance. Children who recognized that their abilities and lifestyles in survivorship are different and found acceptance of these changes accommodated their lifestyle to follow suit. The potential presentation of psychological effects may put some children at more risk than others of experiencing a lower quality of life post-cancer and its treatment [24, 25, 27]. Importantly, all these factors may be occurring in conjunction, worsening the personal burden and impact on short-term and long-term quality of life.
Parents recognized the impact that these changes had on their child’s academic performance. Many parents sought help for their child, primarily through the form of being statemented (given a statement of special needs). Although parents’ experiences were not the focus of this review, a key theme related to the ability to access support. Many parents found that obtaining support for their children was a difficult process and they had to fight for help as monitoring for their child’s cancer diagnosis had ceased years prior. As a result, the education departments deemed there was no evidence of needed support. Many parents failed to obtain the help needed from the education department, leaving these children in a vulnerable position. Resources available for parents/caregivers appeared to be lacking, with minimal support or education provided to the education department, schools, or parents to navigate the process for obtaining additional support or where to obtain it. As such, a secondary finding demonstrates that there is a lack of education support and resources from educational departments for these children and their caregivers. No mention was made as to whether these children were still attending hospitals/clinics in an outpatient capacity, or if they were attending survivorship organizations for additional support.
Additionally, parents expressed significant concern about their child’s ability to be independent and how this may impact their child’s future. Indeed, it is estimated that 60% of childhood CNS tumor survivors do not reach full independence in relation to factors such as employment, living independently, taking care of themselves, obtaining a driver’s license, and marital status [48]. The risk of lower levels of independence was associated with craniospinal irradiation treatment and younger age at diagnosis, putting childhood cancer survivors at particular risk, with the highest incidence of cancer in children aged 1–4 years old [3, 48].
While the experiences children shared primarily related to their academic functioning and social functioning, given how school and friends are critical factors for them during this period of their lives, parents, instead, showed a significant concern for their child’s future—particularly in their ability to be independent and self-care. Despite the evident impact and concern for future outcomes, adequate support and resources were not made available to improve short-term and long-term outcomes for these children.
Despite the broad inclusion criteria to cover those who were undergoing treatment or had completed treatment, all included studies were of children who had completed treatment, likely due to the inherent ethical risks of children undergoing treatment. Additionally, this review had as an inclusion criterion that cancer treatment had to include chemotherapeutic agents, with or without adjuvant therapies, but did not consider treatment strategies without the use of chemotherapy. While individual diagnoses and treatment(s) will vary greatly between patients, it is well established that children being treated for central nervous system (CNS) tumors with radiation therapy, particularly whole-brain irradiation, are at the greatest risk of developing long-term neurocognitive impairments [49]. From a patient perspective, it is of little consequence whether the cognitive decline results from chemotherapy, or some other treatment, the cancer itself, or as a result of missed schooling; the experience of life impact is just as valid. As such, the external validity of the study remains sound. However, more evidence may have been sourced by the inclusion of all cancer types and treatments, regardless of whether adjuvant chemotherapy was administered or not. Additionally, there are few qualitative study designs that investigate this topic utilizing the terminology of “chemobrain,” “chemotherapy-induced cognitive impairment,” or more broadly “cancer-related cognitive impairment,” leading to the inclusion of only six relevant studies that addressed the criteria for these conditions. Rather than specific focuses on outcomes of chemobrain, such as memory or attention, there is a greater focus on how general changes integrate with the children’s lives, making it difficult to discern what outcomes are the result of physical changes, fatigue, time spent at the hospital, memory issues, and so forth. As such, this review was supported by few studies, i.e., limited evidence, however, does identify an important research gap. Within the included studies, as reflected by the quality appraisal, there was a distinct lack of concise and consistent reporting regarding research paradigms and research methodology. Of the excluded studies, many public health researchers, in particular, did not report imperative methodological information, such as participant characteristics, leading to study exclusion and potentially missing out on informative perspectives.
This is reflected as out of 674 studies screened for full-text, only 6 studies were eligible for inclusion. While we acknowledge that this is a small number of studies, it does not limit the value of the included studies to inform our understanding of the self-perceived impact of chemobrain on childhood cancer survivors. Furthermore, it highlights an important gap that should be communicated more widely to the field about the relatively small amount of literature currently available on the patient perspective and identifies a critical area of unmet need that should inform future research.
Clinical implications
From the perspective of childhood cancer survivors, there is a significant area of unmet need surrounding resources, support, and education available for the child themselves, as well as their parents, and those in support positions, such as allied health and educational departments, who may be able to provide support. The use of organized educational programs directed at teachers and class peers, providing guidance on how to manage problems that are associated with school reentry for survivors, has been shown to be successful [50]. Programs provided typically cover tutoring, communication between the family, hospital, and school, education for parents/children regarding return to school, school staff training, individual education plans (IEP), neuropsychological evaluation, cognitive remediation, buddy programs, social skills programs, and planned learning support meetings [50,51,52,53,54]. However, the implementation of school-based interventions appears to be mainly done when legislation requires it [50]. This is particularly evident when considering the geographical location of survivors, with school reentry programs being widely implemented in North America due to legislation which protects the educational and employment rights of individuals with disabilities; however, the form varies widely across the USA due to differences in state laws [49, 50]. While some countries, such as Australia, have both the existence of legislation to protect these children, namely the Disability Discrimination Act 1992 and Disability Standards for Education 2005, and available documentation on return to school, this population is still not adequately supported [55,56,57,58]. Variations and ambiguity in the existing documentation appear to lead to inconsistent care and often fail to facilitate communication between the hospital, home, and school to guide this process [57]. Australian parents report that little or no structured support is provided, with the most common form being “general classroom support” and “school counsellor,” and that accessing support was dependent on the parent’s will rather than a systemically employed approach [56]. Similarly in Europe, rather than the systemic implementation of universal guidelines, survivorship surveillance and care are being driven by research organizations, such as PanCare (Europe) and the European Society for Paediatric Oncology (SIOP). These organizations, in collaboration with 17 partners across Europe, aim to implement digital “Survivorship Passports” that provide childhood/adolescent cancer survivors with custom survivorship plans based on individual medical history [59, 60]. While a promising initiative, these approaches still rely on the survivor and their caregivers to drive their own survivorship care implementation. Interestingly, there is a lack of concordance between government initiatives and these organizations. The European Union has launched the “EU4Health Programme” from 2021 to 2027 utilizing a similar design, the “Cancer Survivor Smart-Card,” to support childhood cancer survivors, rather than working with existing organizations to harmonize the development and implementation of such interventions [61].
Given this, there is a fundamental need for governing bodies to recognize this population and employ both supportive legislation to ensure they are protected and provided with universal resources by their primary healthcare providers following remission with a significant need to focus on harmonizing guidelines and implementation. The use of an assigned liaison for each survivor to help with the transition from hospital to school reentry may be beneficial to act as an advocate for children to access neuropsychological evaluation and occupational therapy, and be an information provider and communicator for parents and involved educational departments ensuring equitable care [50, 54].
Conclusion
To our knowledge, this is the first systematic review of qualitative evidence to examine how chemobrain affects a child’s social, academic, and daily living skills through the voice of the children themselves and/or parent proxy report. This review highlights two important considerations. Firstly, the lived experiences of pediatric childhood cancer survivors, guiding where future interventions should be targeted. While the prevalence and presentation of chemobrain have been previously explored in the literature, we now have evidence that this is reflected in their lived experience and that these findings have a discernible impact on quality of life. Secondly, there is a need to perform more qualitative research studies in this area, as well as to improve the quality of reporting among the existing literature, given that this is a current gap in the field.
Data availability
All data generated and/or analyzed during this study are included in the published article and its supplementary information files. Any queries may be directed to the corresponding author.
References
World Health O (2021) CureAll framework: WHO global initiative for childhood cancer: increasing access, advancing quality, saving lives. World Health Organization, Geneva
Mogavero MP, Bruni O, DelRosso LM, Ferri R (2020). Neurodevelopmental consequences of pediatric cancer and its treatment: the role of sleep. Brain Sci 10(7). https://doi.org/10.3390/brainsci10070411
Wu Y, Deng Y, Wei B, Xiang D, Hu J, Zhao P, Dai Z (2022) Global, regional, and national childhood cancer burden, 1990–2019: an analysis based on the Global Burden of Disease Study 2019. J Adv Res 40:233–247. https://doi.org/10.1016/j.jare.2022.06.001
Ashford J, Schoffstall C, Reddick WE, Leone C, Laningham FH, Glass JO, Conklin HM (2010) Attention and working memory abilities in children treated for acute lymphoblastic leukemia. Cancer 116(19):4638–4645. https://doi.org/10.1002/cncr.25343
Howlader NNA, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA. (2020). SEER Cancer Statistics Review, 1975–2017. Retrieved from https://seer.cancer.gov/csr/1975_2017/. Accessed 22 Nov 2022
Winick N (2011) Neurocognitive outcome in survivors of pediatric cancer. Curr Opin Pediatr 23(1):27–33. https://doi.org/10.1097/MOP.0b013e32834255e9
PDQ® Pediatric Treatment Editorial Board. (06/14/2023). PDQ late effects of treatment for childhood cancer. Retrieved from https://www.cancer.gov/types/childhood-cancers/late-effects-hp-pdq. Accessed 14 Jul 2023
Marusak HA, Iadipaolo AS, Harper FW, Elrahal F, Taub JW, Goldberg E, Rabinak CA (2018) Neurodevelopmental consequences of pediatric cancer and its treatment: applying an early adversity framework to understanding cognitive, behavioral, and emotional outcomes. Neuropsychol Rev 28(2):123–175. https://doi.org/10.1007/s11065-017-9365-1
van der Plas E, Nieman BJ, Butcher DT, Hitzler JK, Weksberg R, Ito S, Schachar R (2015). Neurocognitive late effects of chemotherapy in survivors of acute lymphoblastic leukemia: focus on methotrexate. J Can Acad Child Adolesc Psychiatry, 24(1), 25–32. https://www.ncbi.nlm.nih.gov/pubmed/26336377
Moleski M (2000). Neuropsychological, neuroanatomical, and neurophysiological consequences of CNS chemotherapy for acute lymphoblastic leukemia. Arch Clin Neuropsychol, 15(7), 603–630. https://www.ncbi.nlm.nih.gov/pubmed/14590198. Accessed 22 Nov 2022
Buizer AI, de Sonneville LM, Veerman AJ (2009) Effects of chemotherapy on neurocognitive function in children with acute lymphoblastic leukemia: a critical review of the literature. Pediatr Blood Cancer 52(4):447–454. https://doi.org/10.1002/pbc.21869
Ikonomidou C (2018) Chemotherapy and the pediatric brain. Mol Cell Pediatr 5(1):8. https://doi.org/10.1186/s40348-018-0087-0
Cheung YT, Krull KR (2015) Neurocognitive outcomes in long-term survivors of childhood acute lymphoblastic leukemia treated on contemporary treatment protocols: a systematic review. Neurosci Biobehav Rev 53:108–120. https://doi.org/10.1016/j.neubiorev.2015.03.016
Krull KR, Hardy KK, Kahalley LS, Schuitema I, Kesler SR (2018) Neurocognitive outcomes and interventions in long-term survivors of childhood cancer. J Clin Oncol 36(21):2181–2189. https://doi.org/10.1200/jco.2017.76.4696
Sleurs C, Lemiere J, Vercruysse T, Nolf N, Van Calster B, Deprez S, Uyttebroeck A (2017) Intellectual development of childhood ALL patients: a multicenter longitudinal study. Psychooncology 26(4):508–514. https://doi.org/10.1002/pon.4186
Ahles TA, Saykin AJ, McDonald BC, Furstenberg CT, Cole BF, Hanscom BS, Kaufman PA (2008) Cognitive function in breast cancer patients prior to adjuvant treatment. Breast Cancer Res Treat 110(1):143–152. https://doi.org/10.1007/s10549-007-9686-5
Iuvone L, Peruzzi L, Colosimo C, Tamburrini G, Caldarelli M, Di Rocco C, Riccardi R (2011) Pretreatment neuropsychological deficits in children with brain tumors. Neuro-oncology 13(5):517–524. https://doi.org/10.1093/neuonc/nor013
Margelisch K, Studer M, Ritter BC, Steinlin M, Leibundgut K, Heinks T (2015) Cognitive dysfunction in children with brain tumors at diagnosis. Pediatr Blood Cancer 62(10):1805–1812. https://doi.org/10.1002/pbc.25596
Wefel JS, Lenzi R, Theriault R, Buzdar AU, Cruickshank S, Meyers CA (2004) ‘Chemobrain’ in breast carcinoma?: a prologue. Cancer 101(3):466–475. https://doi.org/10.1002/cncr.20393
Ahles TA, Root JC, Ryan EL (2012) Cancer- and cancer treatment-associated cognitive change: an update on the state of the science. J Clin Oncol 30(30):3675–3686. https://doi.org/10.1200/JCO.2012.43.0116
Wengenroth L, Rueegg CS, Michel G, Gianinazzi ME, Essig S, von der Weid NX, Kuehni CE (2015) Concentration, working speed and memory: cognitive problems in young childhood cancer survivors and their siblings. Pediatr Blood Cancer 62(5):875–882. https://doi.org/10.1002/pbc.25396
Nathan PC, Patel SK, Dilley K, Goldsby R, Harvey J, Jacobsen C, Armstrong FD (2007) Guidelines for identification of, advocacy for, and intervention in neurocognitive problems in survivors of childhood cancer: a report from the Children’s Oncology Group. Arch Pediatr Adolesc Med 161(8):798–806. https://doi.org/10.1001/archpedi.161.8.798
Haupt R, Fears TR, Robison LL, Mills JL, Nicholson HS, Zeltzer LK, Byrne J (1994). Educational attainment in long-term survivors of childhood acute lymphoblastic leukemia. JAMA, 272(18), 1427–1432. https://www.ncbi.nlm.nih.gov/pubmed/7933424. Accessed 22 Nov 2022
Kirchhoff AC, Krull KR, Ness KK, Armstrong GT, Park ER, Stovall M, Leisenring W (2011) Physical, mental, and neurocognitive status and employment outcomes in the childhood cancer survivor study cohort. Cancer Epidemiol Biomarkers Prev 20(9):1838–1849. https://doi.org/10.1158/1055-9965.EPI-11-0239
Mavrea K, Efthymiou V, Katsibardi K, Tsarouhas K, Kanaka-Gantenbein C, Spandidos DA, Bacopoulou F (2021) Cognitive function of children and adolescent survivors of acute lymphoblastic leukemia: a meta-analysis. Oncol Lett 21(4):262. https://doi.org/10.3892/ol.2021.12523
Mohrmann C, Henry J, Hauff M, Hayashi RJ (2015) Neurocognitive outcomes and school performance in solid tumor cancer survivors lacking therapy to the central nervous system. J Pers Med 5(2):83–90. https://doi.org/10.3390/jpm5020083
Zeltzer LK, Recklitis C, Buchbinder D, Zebrack B, Casillas J, Tsao JC, Krull K (2009) Psychological status in childhood cancer survivors: a report from the Childhood Cancer Survivor Study. J Clin Oncol 27(14):2396–2404. https://doi.org/10.1200/JCO.2008.21.1433
Varni JW, Limbers CA, Burwinkle TM (2007) Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL™ 4.0 Generic Core Scales. Health and Quality of Life Outcomes 5(1):2. https://doi.org/10.1186/1477-7525-5-2
Jane C (2011) What is a systematic review? Evid Based Nurs 14(3):64. https://doi.org/10.1136/ebn.2011.0049
Hoffmann T, Bennett S, Del Mar C (2013). Evidence-based practice across the health professions 2nd edition. Sydney: Elsevier, p 349
Althubaiti A (2016) Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc 9:211–217. https://doi.org/10.2147/JMDH.S104807
Lockwood CPK, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M, Loveday H, Carrier J, Stannard D. (2020). Chapter 2: Systematic reviews of qualitative evidence. In: M. Z. Aromataris E (ed), JBI manual for evidence synthesis. JBI Available from https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-03
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Moher D (2021) Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol 134:103–112. https://doi.org/10.1016/j.jclinepi.2021.02.003
Semendric I, Pollock D, Haller OJ, George RP, Collins-Praino L E, Whittaker AL (2022). Impact of “chemobrain” in childhood cancer survivors on social, academic, and daily living skills: a qualitative systematic review protocol. JBI Evid Synth, 20(1), 222–228. https://doi.org/10.11124/JBIES-21-00115
Munn Z, Aromataris E, Tufanaru C, Stern C, Porritt K, Farrow J, Jordan Z (2019) The development of software to support multiple systematic review types: the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI). Int J Evid Based Healthc 17(1):36–43. https://doi.org/10.1097/XEB.0000000000000152
Munn Z, Porritt K, Lockwood C, Aromataris E, Pearson A (2014) Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Med Res Methodol 14:108. https://doi.org/10.1186/1471-2288-14-108
Lockwood C, Munn Z, Porritt K (2015) Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc 13(3):179–187. https://doi.org/10.1097/XEB.0000000000000062
Choquette A, Rennick JE, Lee V (2016) Back to school after cancer treatment: making sense of the adolescent experience. Cancer Nurs 39(5):393–401. https://doi.org/10.1097/ncc.0000000000000301
Vance YH, Eiser C, Horne B (2004) Parents’ views of the impact of childhood brain tumours and treatment on young people’s social and family functioning. Clin Child Psychol Psychiatry 9(2):271–288. https://doi.org/10.1177/1359104504041923
Chen CM, Hsu BH, Chen YC, Cheng SN, Liaw JJ (2015) Meshing gears: mothers and their adolescents returning to their social life after cancer treatment in Taiwan. J Pediatr Oncol Nurs 32(4):219–229. https://doi.org/10.1177/1043454214563402
Vanclooster S, Van Hoeck K, Peremans L, Bilsen J, Der Werff Van, Ten Bosch J, Laureys G, Jansen A (2021) Reintegration into school of childhood brain tumor survivors: a qualitative study using the International Classification of Functioning, Disability and Health – Children and Youth framework. Disability and Rehabilitation 43(18):2610–2620. https://doi.org/10.1080/09638288.2019.1708484
Walker AJ, Lewis FM, Lin Y, Zahlis E, Rosenberg AR (2019) Trying to feel normal again: early survivorship for adolescent cancer survivors. Cancer Nurs 42(4):E11-e21. https://doi.org/10.1097/ncc.0000000000000629
Suntup M (1999). An initial reintegration treatment of children with acute lymphoblastic leukemia. (Publication No. 9923133). (Doctoral Dissertation, California School of Professional Psychology - San Diego, Ann Arbor). ProQuest Dissertations & Theses Global database
Emerson ND, Distelberg B, Morrell HE, Williams-Reade J, Tapanes D, Montgomery S (2016) Quality of life and school absenteeism in children with chronic illness. J Sch Nurs 32(4):258–266. https://doi.org/10.1177/1059840515615401
Park M, Park HJ, Lee JM, Ju HY, Park BK, Yu ES, Shin HY (2018) School performance of childhood cancer survivors in Korea: a multi-institutional study on behalf of the Korean Society of Pediatric Hematology and Oncology. Psychooncology 27(9):2257–2264. https://doi.org/10.1002/pon.4819
Ruiz-Casado A, Álvarez-Bustos A, de Pedro CG, Méndez-Otero M, Romero-Elías M (2021) Cancer-related fatigue in breast cancer survivors: a review. Clin Breast Cancer 21(1):10–25. https://doi.org/10.1016/j.clbc.2020.07.011
Ekenga CC, Pérez M, Margenthaler JA, Jeffe DB (2018) Early-stage breast cancer and employment participation after 2 years of follow-up: a comparison with age-matched controls. Cancer 124(9):2026–2035. https://doi.org/10.1002/cncr.31270
Brinkman TM, Ness KK, Li Z, Huang IC, Krull KR, Gajjar A, Armstrong GT (2018) Attainment of functional and social independence in adult survivors of pediatric CNS tumors: a report from the St Jude Lifetime Cohort Study. J Clin Oncol 36(27):2762–2769. https://doi.org/10.1200/jco.2018.77.9454
Castellino SM, Ullrich NJ, Whelen MJ, Lange BJ (2014). Developing interventions for cancer-related cognitive dysfunction in childhood cancer survivors. J Natl Cancer Inst, 106(8). https://doi.org/10.1093/jnci/dju186
Institute of Medicine (US) and National Research Council (US) (2003) National cancer policy board. In: Hewitt M, Weiner SL, Simone JV (eds) Childhood cancer survivorship: Improving care and quality of life. National Academies Press (US). https://doi.org/10.17226/10767
Armstrong D (2008). Advocating for your child’s learning needs: through treatment and beyond. Telephone Education Program. http://www.leukemia-lymphoma.org. Accessed 9 Aug 2023
Butler RW, Mulhern RK (2005) Neurocognitive interventions for children and adolescents surviving cancer. J Pediatr Psychol 30(1):65–78. https://doi.org/10.1093/jpepsy/jsi017
Butler RW, Sahler OJ, Askins MA, Alderfer MA, Katz ER, Phipps S, Noll RB (2008) Interventions to improve neuropsychological functioning in childhood cancer survivors. Dev Disabil Res Rev 14(3):251–258. https://doi.org/10.1002/ddrr.33
Donnan BM, Webster T, Wakefield CE, Dalla-Pozza L, Alvaro F, Lavoipierre J, Marshall GM (2015) What about school? Educational challenges for children and adolescents with cancer. Aust Ed Dev Psych 32(1):23–40. https://doi.org/10.1017/edp.2015.9
Psychosocial management of AYA cancer patients Working Group. (06/06/2023). COSA: Psychosocial management of AYA cancer patients/summary of good practice points. Psychosocial management of AYAs diagnosed with cancer: Guidance for health professionals. https://wiki.cancer.org.au/australiawiki/index.php?oldid=78878. Accessed 9 Aug 2023
Martinez-Santos AE, Fernandez-De-La-Iglesia JDC, Sheaf G, Coyne I (2021) A systematic review of the educational experiences and needs of children with cancer returning to school. J Adv Nurs 77(7):2971–2994. https://doi.org/10.1111/jan.14784
Lum A, Donnan B, Wakefield CE, Fardell JE, Marshall GM (2017) Establishing Australian school re-entry service guidelines for children diagnosed with cancer. J Paediatr Child Health 53(6):529–533. https://doi.org/10.1111/jpc.13563
Cancer Council Australia. (2018, June 2018). Cancer in the school community: A guide for staff members. https://www.cancer.org.au/assets/pdf/cancer-in-the-school-community
Haupt R, Essiaf S, Dellacasa C, Ronckers CM, Caruso S, Sugden E, ExPo-r-Net Working G (2018) The ‘Survivorship Passport’ for childhood cancer survivors. Eur J Cancer 102:69–81. https://doi.org/10.1016/j.ejca.2018.07.006
van Kalsbeek RJ, van der Pal HJH, Hjorth L, Winther JF, Michel G, Haupt R, PanCareFollowUp C (2021) The European multistakeholder PanCareFollowUp project: novel, person-centred survivorship care to improve care quality, effectiveness, cost-effectiveness and accessibility for cancer survivors and caregivers. Eur J Cancer 153:74–85. https://doi.org/10.1016/j.ejca.2021.05.030
European Commission. (2021). Europe’s beating cancer plan communication from the comission to the European Parliament and the Council. https://health.ec.europa.eu/system/files/2022-02/eu_cancer-plan_en_0.pdf. Accessed 9 Aug 2023
Acknowledgements
We thank Ms. Vikki Langton, library liaison, for her assistance in the development and execution of the search strategy utilized to inform this review.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. I. S. and O. H. are supported by the Australian Government Research Training Program Scholarship. A. L. W. was supported by a NHMRC Peter Doherty Biomedical Research Fellowship (APP1140072). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Ines Semendric: conceptualization; methodology; investigation; data curation; formal analysis; writing—original draft; writing—review and editing; visualization. Danielle Pollock: methodology; resources; data curation; formal analysis; writing—review and editing; visualization. Olivia J. Haller: investigation, data curation, formal analysis, visualization. Rebecca P. George: investigation, data curation, visualization. Lyndsey. E Collins-Praino: supervision; writing—review and editing, visualization. Alexandra L. Whittaker: supervision, conceptualization, methodology, data curation, formal analysis, writing—review and editing, visualization.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Semendric, I., Pollock, D., Haller, O.J. et al. “Chemobrain” in childhood cancer survivors—the impact on social, academic, and daily living skills: a qualitative systematic review. Support Care Cancer 31, 532 (2023). https://doi.org/10.1007/s00520-023-07985-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07985-z