Abstract
Purpose
Many patients prefer an active role in making decisions about their care and treatment, but participating in such decision-making is challenging. The aim of this study was to explore whether patient-reported outcomes (quality of life and patient satisfaction), patients’ coping strategies, and sociodemographic and clinical characteristics were associated with self-efficacy for participation in decision-making among patients with advanced cancer.
Methods
We used baseline data from the ACTION trial of patients with advanced colorectal or lung cancer from six European countries, including scores on the decision-making participation self-efficacy (DEPS) scale, EORTC QLQ-C15-PAL questionnaire, and the EORTC IN-PATSAT32 questionnaire. Multivariable linear regression analyses were used to examine associations with self-efficacy scores.
Results
The sample included 660 patients with a mean age of 66 years (SD 10). Patients had a mean score of 73 (SD 24) for self-efficacy. Problem-focused coping (B 1.41 (95% CI 0.77 to 2.06)), better quality of life (B 2.34 (95% CI 0.89 to 3.80)), and more patient satisfaction (B 7.59 (95% CI 5.61 to 9.56)) were associated with a higher level of self-efficacy. Patients in the Netherlands had a higher level of self-efficacy than patients in Belgium ((B 7.85 (95% CI 2.28 to 13.42)), whereas Italian patients had a lower level ((B −7.50 (95% CI −13.04 to −1.96)) than those in Belgium.
Conclusion
Coping style, quality of life, and patient satisfaction with care were associated with self-efficacy for participation in decision-making among patients with advanced cancer. These factors are important to consider for healthcare professionals when supporting patients in decision-making processes.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Patients with advanced cancer often face complex treatment decisions that can have important consequences in terms of quality and length of life. Shared decision-making has been acknowledged as the preferred model to engage and support patients in the decision-making process about diagnosis, treatment, and care [1, 2]. Initiatives targeting shared decision-making are growing and are advocated internationally by key figures such as patient representatives, policymakers, and hospitals [1]. Shared decision-making requires active participation from both health care provider and patient as they have to collaborate in considering relevant treatment options, taking into account the goals and values of the patient. An important aspect for physicians in the decision-making process is to communicate and behave in a way that facilitates the patient to express him or herself, speak openly, and ask questions about their care and treatment options [3, 4].
It has been suggested that patients who participate more actively in decision-making processes have better physical and mental health and tend to be more satisfied with their care than patients with a less active role [5, 6]. In addition, patient participation in decision-making improves the patient-physician relationship and communication [7, 8]. However, although many patients prefer an active role [9, 10], it is challenging for patients to adequately participate in decision-making about treatment and care [11]. Several studies have shown a difference between patients’ preferred and actual roles during decision-making [11, 12]. For patients, an important aspect for participation in decision-making according to their preferred role is self-efficacy in communicating with physicians [4]. Self-efficacy refers to individual’s confidence or belief to carry out a specific task in order to reach a desired outcome [13]. In the interaction with physicians, self-efficacy is the self-perceived ability of patients to gather medical information from physicians and to ensure that their health-related concerns are identified and addressed [14]. Self-efficacy regarding decision-making is associated with greater participation in treatment-related decision-making [15], such as asking questions, and better disease-specific health-related quality of life [16].
Self-efficacy in decision-making can affect and be affected by elements of the patient-physician interaction, including information exchange, trust, satisfaction, and understanding instructions and treatment options [17, 18]. The more the patient has experienced being listened to and having questions answered, the more likely the patient is to have higher levels of self-efficacy [19]. Furthermore, in a study among patients with prostate cancer, those who were less satisfied with their care, or had more symptom distress were more likely to have a low level of self-efficacy in interacting with physicians [20]. In non-oncology settings, it was suggested that patients provided with good verbal support by their physician (e.g., information about symptoms and strategies to manage these) may have higher levels of self-efficacy in decision-making [21, 22]. Patient-related factors such as health literacy, socioeconomic status, age, religious beliefs, and coping with cancer have also been linked to self-efficacy [14, 23,24,25,26,27,28]. In addition, clinical characteristics such as poor clinical performance status have been associated with less confidence in making decisions among patients with lung cancer [29]. All these studies have, however, been conducted among specific patient populations, such as older people, or within particular types of cancer, including breast cancer or prostate cancer, and are, thus, limited to either male or female subjects. Less is known about self-efficacy regarding decision-making among patients diagnosed with highly prevalent cancers that affect both males and females, such as lung and colorectal cancer.
A better understanding of factors associated with self-efficacy is important for supporting patients’ participation in the decision-making process. The aim of this study was to explore whether sociodemographic and clinical characteristics, patient-reported outcomes (i.e., quality of life (QoL) and patient satisfaction), and coping strategies were associated with self-efficacy regarding treatment-related decision-making among patients with advanced lung or colorectal cancer in six European countries.
Methods
Study design and setting
Baseline data were used from the ACTION study, a multicenter cluster-randomized trial to investigate the effects of an advance care planning (ACP) intervention compared to care as usual [30]. ACP is a formal process of communication between patients, relatives, and healthcare professionals about future care and promotes discussion of preferences [31]. Patients were recruited in pulmonology and oncology departments in academic and nonacademic hospitals in Belgium, Denmark, Italy, the Netherlands, Slovenia, and the UK. Written informed consent was obtained. The trial was approved by research ethics committees in all participating countries.
Recruitment took place between May 2015 and February 2018. Hospitals were randomized to the intervention arm, providing usual care and ACP, or the control arm, providing usual care. All patients with advanced lung (stage III or IV) or colorectal cancer (stage IV), WHO performance status 0–3, an estimated life expectancy of at least 3 months, and competence to give consent were eligible. When a care team considered patients eligible, they were asked to consider participation in ACTION. Patients who wanted to consider participation were contacted by the researcher team and provided with more information about the study. Patients in control hospitals were informed that the study focused on preparing patients for decision-making about care, and that they would receive usual care.
Due to the cluster-randomized study design in which patients knew beforehand whether they were recruited for the intervention group or the control group, and as the response rate was substantially lower in the intervention than in the control arm [32], patients in the intervention and control groups may not be entirely comparable. Since the response rate was substantially higher in the control group and, thus, data from this group was more reliable, we chose to only include baseline patient data from the control arm (care as usual) in the present study. Care as usual mainly consisted of receiving systemic treatment and related support as provided by the hospitals.
Measures
Patients were asked to complete a written questionnaire at baseline, at 2.5 months, and 4.5 months after inclusion. The primary outcomes of the ACTION study were quality of life, assessed with 10 items of the European Organisation for Research and Treatment of Cancer (EORTC) emotional functioning item bank [33, 34] and symptoms (EORTC QLQ-C15-PAL [35]). Several secondary outcomes were coping (COPE, Brief COPE [36, 37]), satisfaction with care (items of the EORTC IN-PATSAT [38]), satisfaction with the intervention (9 study-constructed items), and shared decision-making (decision-making self-efficacy scale [39]). Details of the measures used for the present study are presented below.
Sociodemographic and clinical characteristics
At baseline, patients provided information about their age, educational level (number of years of education), gender (male/female), living situation (with/without a spouse), having children (yes/no), and religiosity (yes/no/prefer not to specify). Ethnicity was measured by asking whether participants considered themselves a member of a minority ethnic group (yes/no). Healthcare providers gave information on patients’ type of cancer (lung/colorectal cancer), the time since diagnosis of the primary tumor, current stage of the disease, current treatment (yes/no receiving systemic treatment), and performance status according to the World Health Organization (WHO) (0-fully active to 3-capable of only limited self-care).
Self-efficacy for participation in decision-making
To assess patient’s self-efficacy for participation in different activities associated with treatment-related decision-making, the decision-making participation self-efficacy scale (DEPS) was used [39]. Activities addressed in this scale include: (1) participating in discussions with the physician about available treatment options; (2) raising questions or concerns about the physician’s recommendations; (3) telling the physician which option one prefers; (4) resolving differences of opinion; (5) taking responsibility for making the final decision. Patients could score how confident they were about these items using a five-point Likert response scale, ranging from “not at all confident” to “completely confident”. The mean score of the responses to the five items was computed and then linearly transformed into a 0–100 metric scale score [39]. A higher score indicates a higher perceived self-efficacy for participation in treatment-related decision-making.
Coping
Coping was measured using the subscales denial and acceptance of the COPE inventory and the subscales planning and active coping of the brief COPE [36]. Patients were asked to rate the items according to the best description of how they had been coping with their disease during the past 2 months. Items were rated on a four-point Likert scale from 1 (“I don’t do this at all”), 2 (“I do this a little bit”), 3 (“I do this a medium amount”), to 4 (“I do this a lot”). As recommended [40], principal components analysis was conducted to confirm subscales of the underlying coping strategies. The analysis confirmed the denial, acceptance, and problem-focused coping subscales. Responses per subscale were summed to create subscale sum scores. This resulted in a range of 4 to 16 for each subscale, with higher scores indicating more use of that particular coping strategy.
Quality of life (QoL)
As overall quality of life was one of the variables of interest, we used a question from the EORTC QLQ-C30 questionnaire asking patients how they would rate their overall quality of life during the past week on a seven-point Likert scale ranging from 1 (poor) to 7 (excellent) [33].
Patient satisfaction about care
As general patient satisfaction was one of the variables of interest, we used a question from the EORTC IN-PATSAT32 questionnaire, asking how patients, in general, would rate the hospital care they received during the past 2 months on a five-point Likert scale ranging from 1 (poor) to 5 (excellent) [38].
Analyses
Descriptive statistics were used to summarize the characteristics of the study population. The Pearson (r) and Spearman (rs) correlation methods were used to, respectively, assess correlations of continuous and ordinal scale variables with self-efficacy scores. Multivariable linear regression analyses were performed to investigate the association of clinical characteristics, patient-reported outcomes (QoL and patient satisfaction with care), and coping strategies (independent variables) with patients’ self-efficacy (dependent variable). We used five linear regression models, with model 0 adjusted for sociodemographic characteristics including age, sex, living with a spouse, having children, years of education, religiosity, country of residence, and considering oneself a member of a minority group. We added the following variables to model 0: model (1a) clinical characteristics, model (1b) coping strategies, and model (1c) QoL and patient satisfaction with care. In the final model (model 2), all sociodemographic and clinical characteristics, patient-reported outcomes, and coping strategies were included. Regression coefficients and 95% confidence intervals were used to evaluate associations between the independent variables and self-efficacy. P values lower than 0.05 were considered statistically significant. The explained variance (adjusted R) of each model was shown.
Multiple imputation was used to deal with missing data of independent variables. Missing values on independent variables were imputed by the use of the multivariate imputation by chained equations (MICE) [41]. The percentages of missing values per variable varied from 0.2 to 14% and were assumed to be missing at random. Five imputed datasets were generated, and the results of the pooled analyses are presented. In sensitivity analysis, multivariable linear regression analyses were performed on cases with complete data, in order to assess departures from the missing at random assumption. All analyses were performed using SPSS Statistical version 28 (IBM).
Results
The study population included 660 patients. The number of patients per country ranged from n = 25 in Slovenia to n = 164 in the Netherlands. Patients had a mean age of 66 years (SD 9.6), and the majority were men (n = 394, 60%). Most patients lived with a spouse (n = 490, 74%), and slightly more than half of the patients were religious (n = 334, 51%). Half of the patients were diagnosed with lung cancer (n = 331, 50%). Most patients received systemic anti-tumor treatment at the time of inclusion in the study (n = 581, 88%), (Table 1).
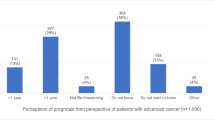
Patients had an average score of 72.8 (SD 23.9) on self-efficacy for participation in decision-making (Table 1, Supplemental Table 1). Patients in the Netherlands (B 10.77 (95% CI 5.47 to 16.07)), Denmark (B 10.34 (95% CI 3.53 to 17.15)), and UK (B 7.10 (95% CI 1.49 to 12.71)) had a higher level of self-efficacy for participation in decision-making compared to patients in Belgium (reference group), whereas Italian patients had a lower level ((B −7.38 (95% CI −12.94 to −1.83)) than patients in Belgium (model 0, not shown). Patients who indicated to be religious (B −4.33 (95% CI −8.41 to −0.25)) or preferred not to specify their religion (B −6.70 (95% CI −12.33 to −1.08)) had lower levels of self-efficacy for participation in decision-making compared to those who were not religious (model 0, not shown). In model 1a, a lower WHO performance status was associated with a lower level of self-efficacy for participation in decision-making (B −5.27 (95% CI −8.54 to −2.01)) (Table 2). Higher scores of problem-focused coping were associated with higher levels of self-efficacy for participation in decision-making ((B 1.63 (95% CI 0.96 to 2.31)) (model 1b). Higher scores for acceptance coping were also associated with higher levels of self-efficacy for participation in decision-making ((B 1.13 (95% CI 0.43 to 1.83)), (Table 2).
A better QoL was associated ((B 2.78 (95% CI 1.41 to 4.15)) with a higher level of self-efficacy for participation in decision-making. Greater patient satisfaction with hospital care was also associated ((B 8.25 (95% CI 6.29 to 10.22)) with a higher level of self-efficacy for participation in decision-making (model 1c). In the final model (model 2), the effect estimates for problem-focused coping style, QoL, patient satisfaction with care, and country of residence remained significant. The explained variance of this model was 28% (adjusted R2 = 0.28). The sensitivity analyses performed on a sample with complete data (n = 450) showed comparable results (Supplemental Table 2).
Discussion
In this study in six European countries, we explored whether sociodemographic and clinical characteristics, coping strategies, and patient-reported outcomes were associated with self-efficacy for participation in treatment-related decision-making among patients with advanced cancer. We found problem-focused coping, better QoL, and more patient satisfaction with hospital care to be associated with higher levels of self-efficacy for participation in decision-making. Differences were observed in self-efficacy scores for participation in decision-making between countries.
The present study shows that patients reporting problem-focused coping strategies had a higher level of self-efficacy for participation in decision-making. In general, it is well known that patients reporting active or problem-focused coping fare better on a variety of physical and mental health outcomes than those less reporting active or problem-focused coping [42, 43]. Although literature on the association of coping and self-efficacy for participation in decision-making is scarce, our findings are in line with one study among slightly older patients showing that those who reported to have an active coping style rather than an avoidant coping style were more confident in interacting with physicians [14]. Patients who have an active or problem solving coping style may feel more confident to participate in decision-making with physicians, as they tend to show proactive behavior in order to solve issues as part of their coping strategy. A higher level of self-efficacy for participation in decision-making can lead to more participation in the decision-making process and, thus, positively influence health and functioning [15]. Therefore, supporting patients’ active coping mechanisms may lead to higher levels of self-efficacy for participation in decision-making about treatment.
In a study among patients with different types of cancer, those who reported to use active coping styles were more likely to have an active rather than passive role in decision-making [44]. In addition, it was suggested that patients’ decision-making role is one component of a coping style, indicating that decision-making role and coping style may be related as part of one process. This is in contrast to previous studies which considered decision-making and coping styles as separate phenomena [44]. It might be useful to study the role of self-efficacy for participation in decision-making in the context of different coping styles in order to gain a better understanding of self-efficacy for participation in decision-making.
It is worth noting that patients who prefer the doctor to make decisions do not necessarily have a lower level of self-efficacy for participation in decision-making. One study among 623 bladder, leukemia, and colorectal cancer survivors showed that those who prefer the physician to control decisions had similar self-efficacy levels for engaging in the decision-making process and greater trust in their physicians compared to those who prefer a more active role in decision-making [45]. This may illustrate the importance of supporting patients’ self-efficacy to participate in decision-making regardless of who controls the decisions. When physicians recognize and support patients’ capabilities and beliefs and establish a trusting relationship, physicians can help to foster self-efficacy beliefs regardless of patients’ preferences for an active or inactive role [46, 47]. Therefore, interventions to support or increase patients’ self-efficacy for participation during the decision-making process with the physician could facilitate the discussion about the extent to which patients wish to be engaged in the decision-making process [15]. This may particularly benefit patient populations characterized by low education or income, ethnic minorities, or low health literacy and, therefore, not optimally involved in treatment-related decision-making [4, 48].
Patient satisfaction with care was also associated with self-efficacy for participation in decision-making. Although comparable studies are lacking, one study among low-income men with early-stage prostate cancer also showed that less satisfaction with care was associated with lower self-efficacy to interact with physicians [20], and the same was found in a study of older patients [14]. Together with our results, these findings may imply that satisfaction with care can influence self-efficacy for participation in decision-making, or vice versa. Satisfaction with care often includes patients’ evaluation of the quality of communication with physicians [17]. A good patient-physician communication may lead to shared understanding, trust in decision-making, and, thus, more patient satisfaction [49, 50]. As a result, patients may feel valued, comfortable, and supported to ask questions and share concerns or expectations and, thus, develop a higher level of self-efficacy for participation in decision-making.
Better QoL was the third factor associated with a higher level of self-efficacy for participation in decision-making. It is unknown whether the association is due to patients’ physical or mental well-being. In a study among older persons, better health status was associated with a higher level of self-efficacy in patient-physician interactions [14]. In another study, patient self-efficacy in communicating with physicians predicted better QoL [20]. These studies imply that next to elements of the patient-physician interaction, self-efficacy for participation in decision-making can also affect and be affected by aspects of well-being. Given the impact of cancer on patients’ daily functioning and well-being, it is relevant that physicians and patients collaborate to discuss patients’ QoL and support patients to feel confident to engage in decision-making about their care and treatment.
Differences between countries were found in self-efficacy levels for participation in decision-making. Patients in the Netherlands had a higher level of self-efficacy for participation in decision-making than patients in Belgium, whereas Italian patients had a lower level than those in Belgium. In a previous European study, large variations were found between countries in the extent to which decisions were discussed with patients [51]. End-of-life decisions were discussed with the patient and relatives most frequently in the Netherlands and least frequently in Italy. For example, more than 50% of all end-of-life decisions were discussed neither with the patient nor with relatives in Italy. Patients were generally involved in decision-making in countries in which the frequency of making these decisions is high, which was the case in The Netherlands. Therefore, the practice of end-of-life discussions and patient involvement in countries may be associated with or reflect self-efficacy levels for participation in decision-making among patients and potentially explain differences between countries.
This study has several strengths. The DEPS scale used in this study covers several important aspects of self-efficacy for participation in decision-making such as the ability to ask questions. Other studies have used the validated perceived efficacy in patient-physicians interaction (PEPPI) scale [14] and the decision self-efficacy scale (DSE). However, these assess patients’ confidence in participating in interactions with physicians in general and not within the context of medical decision-making and do not provide emphasis on the decision-making process. Another strength is that we were able to include a substantial number of patients with advanced cancer across multiple countries, whereas data about patients at this stage are not easy to obtain due to their vulnerability.
One limitation of this study is that due to its cross-sectional design, it cannot provide robust insight into causal relationships. It is, however, likely that the associations studied are complex and bidirectional. In addition, it might be useful to understand which aspects of self-efficacy are particularly important in order to actually participate in decision-making [29]. Another limitation of this study relates to the low number of individuals considering themselves part of a minority group within the six countries. This might have led to sampling bias, i.e., people who participated to the study may reflect higher levels of self-efficacy for participation in decision-making compared to people from ethnic minority groups who may have lower levels of self-efficacy, for example, due to language barriers. Lastly, since we were interested in overall QoL and patient satisfaction in general, it remains unknown which elements of these concepts are related to self-efficacy for participation in decision-making. We only used one item measuring QoL and patient satisfaction. It would potentially have strengthened the reliability of results if we had used a multi-item scale measuring these constructs. Future research could investigate which specific components of quality of life and patient satisfaction correlate with self-efficacy for participation in decision-making. This would help to identify areas where interventions can be implemented more effectively.
Since our findings show associations of coping strategies, patient satisfaction, and quality of life with self-efficacy for participation in decision-making, we recommend to take into account these aspects when developing tailored interventions to facilitate self-efficacy or patient empowerment, especially in the face of a growing population of individuals living with advanced cancer. This requires physicians to become a skilled companion asking the right questions about what matters to the patient, while supporting them to actively participate in decision-making about treatment [52]. Given the potential benefits of a problem-focused coping style, it is important that healthcare professionals find patient-centered ways to support patients who have difficulties to cope with their disease [53]. Physicians should be aware that patients who have difficulties to cope with their disease or use avoidant coping strategies may not feel confident to interact with physicians. Also, adopting a participatory physician decision-making style in which patients are involved in the decision-making process may facilitate self-efficacy for participation in decision-making among patients [54].
In conclusion, this study shows that a problem-focused coping strategy, better patient satisfaction, and better QoL were associated with higher levels of self-efficacy for participation in decision-making among patients with advanced cancer. Differences between countries were observed in patients’ self-efficacy for participation in decision-making. We recommend physicians who aim to support patients in a process of decision-making to take into account patients’ coping strategy. Furthermore, they should be aware that patients’ self-efficacy for participation in decision-making is positively related to their satisfaction with care and their QoL.
Data Availability
The dataset analyzed during the current study is not publicly available, but is available from the corresponding author on reasonable request.
References
Stiggelbout AM, Pieterse AH, De Haes JC (2015) Shared decision making: concepts, evidence, and practice. Patient Educ Couns 98(10):1172–1179
Elwyn G et al (2010) Implementing shared decision making in the NHS. BMJ 341:c5146
Stewart MA (1984) What is a successful doctor-patient interview? A study of interactions and outcomes. Soc Sci Med 19(2):167–175
Bylund CL et al (2010) Improving clinical communication and promoting health through concordance-based patient education. Commun Educ 59(3):294–311
Brown R et al (2012) Meeting the decision-making preferences of patients with breast cancer in oncology consultations: impact on decision-related outcomes. J Clin Oncol 30(8):857–862
Kane HL et al (2014) Implementing and evaluating shared decision making in oncology practice. CA Cancer J Clin 64(6):377–388
Cegala DJ, Street RL Jr, Clinch CR (2007) The impact of patient participation on physicians’ information provision during a primary care medical interview. Health Commun 21(2):177–185
Shay LA et al (2012) Factors associated with patient reports of positive physician relational communication. Patient Educ Couns 89(1):96–101
Skyring TA, Mansfield KJ, Mullan JR (2021) Factors affecting satisfaction with the decision-making process and decision regret for men with a new diagnosis of prostate cancer. Am J Mens Health 15(4):15579883211026812
Chewning B et al (2012) Patient preferences for shared decisions: a systematic review. Patient Educ Couns 86(1):9–18
Tariman JD et al (2010) Preferred and actual participation roles during health care decision making in persons with cancer: a systematic review. Ann Oncol 21(6):1145–1151
Keating NL et al (2002) Treatment decision making in early-stage breast cancer: should surgeons match patients’ desired level of involvement? J Clin Oncol 20(6):1473–1479
Bandura A, Freeman WH, Lightsey R (1999) Self-efficacy: the exercise of control. Springer
Maly RC et al (1998) Perceived efficacy in patient-physician interactions (PEPPI): validation of an instrument in older persons. J Am Geriatr Soc 46(7):889–894
Maly RC et al (2004) Determinants of participation in treatment decision-making by older breast cancer patients. Breast Cancer Res Treat 85(3):201–209
Heckman JE et al (2011) The role of self-efficacy in quality of life for disadvantaged men with prostate cancer. J Urol 186(5):1855–1861
Stewart M et al (2000) The influence of older patient-physician communication on health and health-related outcomes. Clin Geriatr Med 16(1):25–36
Heisler M et al (2002) The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med 17(4):243–252
Zachariae R et al (2003) Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. Br J Cancer 88(5):658–665
Maliski SL et al (2004) Confidence in the ability to communicate with physicians among low-income patients with prostate cancer. Urology 64(2):329–334
Ng YK et al (2018) Attitudes toward concordance and self-efficacy in decision making: a cross-sectional study on pharmacist-patient consultations. Patient Prefer Adherence 12:615–624
Hoffman AJ (2013) Enhancing self-efficacy for optimized patient outcomes through the theory of symptom self-management. Cancer Nurs 36(1):E16
Woodward NJ, Wallston BS (1987) Age and health care beliefs: self-efficacy as a mediator of low desire for control. Psychol Aging 2(1):3
Magon A et al (2021) Trajectories of health-related quality of life, health literacy, and self-efficacy in curatively-treated patients with esophageal cancer: a longitudinal single-center study in Italy. J Patient Exp 8:23743735211060769
Yuan C et al (2014) Self-efficacy difference among patients with cancer with different socioeconomic status: application of latent class analysis and standardization and decomposition analysis. Cancer Epidemiol 38(3):298–306
Farahbakhshbeh S, Nejad SAM, Moazedian A (2019) Predicting self-efficacy of women with breast cancer based on quality of life, religious orientation, resilience, death anxiety, psychological hardiness and perceived social support. Iranian. J Health Psychol 2(1):65–78
Ong LML et al (1999) Cancer patients’ coping styles and doctor–patient communication. Psycho-Oncology 8(2):155–166
Luce MF (2005) Decision making as coping. Health Psychol 24(4S):S23
Pompili C et al (2020) Patients’ confidence in treatment decisions for early stage non-small cell lung cancer (NSCLC). Health Qual Life Outcomes 18(1):1–8
Rietjens JAC et al (2016) Advance care planning – a multi-centre cluster randomised clinical trial: the research protocol of the ACTION study. BMC Cancer 16(1):264
National End of Life Care, P (2007) Advance care planning: a guide for health and social care staff. National End of Life Care Programme
Korfage IJ et al (2020) Advance care planning in patients with advanced cancer: a 6-country, cluster-randomised clinical trial. PLoS Med 17(11):e1003422
Aaronson NK et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Petersen MA et al (2016) An emotional functioning item bank of 24 items for computerized adaptive testing (CAT) was established. J Clin Epidemiol 70:90–100
Groenvold M et al (2006) The development of the EORTC QLQ-C15-PAL: a shortened questionnaire for cancer patients in palliative care. Eur J Cancer 42(1):55–64
Carver CS (1997) You want to measure coping but your protocol’too long: consider the brief cope. Int J Behav Med 4(1):92–100
Carver CS, Scheier MF, Weintraub JK (1989) Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol 56(2):267
Bredart A et al (2005) An international prospective study of the EORTC cancer in-patient satisfaction with care measure (EORTC IN-PATSAT32). Eur J Cancer 41(14):2120–2131
Arora NK et al (2009) Physicians’ decision-making style and psychosocial outcomes among cancer survivors. Patient Educ Couns 77(3):404–412
Jabbarian LJ et al (2020) Coping strategies of patients with advanced lung or colorectal cancer in six European countries: insights from the ACTION Study. Psycho-Oncology 29(2):347–355
Azur MJ et al (2011) Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res 20(1):40–49
Henoch I et al (2007) The impact of symptoms, coping capacity, and social support on quality of life experience over time in patients with lung cancer. J Pain Symptom Manag 34(4):370–379
Kershaw T et al (2004) Coping strategies and quality of life in women with advanced breast cancer and their family caregivers. Psychol Health 19(2):139–155
Colley A et al (2017) Factors associated with oncology patients’ involvement in shared decision making during chemotherapy. Psycho-oncology 26(11):1972–1979
Chawla N, Arora NK (2013) Why do some patients prefer to leave decisions up to the doctor: lack of self-efficacy or a matter of trust? J Cancer Surviv 7(4):592–601
Joseph-Williams N, Elwyn G, Edwards A (2014) Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns 94(3):291–309
Fraenkel L, McGraw S (2007) What are the essential elements to enable patient participation in medical decision making? J Gen Intern Med 22(5):614–619
Perez Jolles M, Richmond J, Thomas KC (2019) Minority patient preferences, barriers, and facilitators for shared decision-making with health care providers in the USA: A systematic review. Patient Educ Couns 102(7):1251–1262
Street RL Jr et al (2009) How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns 74(3):295–301
Andersen MR et al (2009) Involvement in decision-making and breast cancer survivor quality of life. Health Psychol 28(1):29
van der Heide A et al (2003) End-of-life decision-making in six European countries: descriptive study. Lancet 362(9381):345–350
van Delden JJM et al (2022) Asking the right questions: towards a person-centered conception of shared decision-making regarding treatment of advanced chronic kidney disease in older patients. BMC Med Ethics 23(1):1–8
Walshe C et al (2017) Coping well with advanced cancer: a serial qualitative interview study with patients and family carers. PLoS One 12(1):e0169071
Maly RC et al (2008) Racial/ethnic differences in breast cancer outcomes among older patients: effects of physician communication and patient empowerment. Health Psychol 27(6):728–736
Acknowledgements
We thank all participating patients, hospital staff, and the Advisory Board for their valuable contribution to this project.
Funding
The ACTION trial was supported by the European Union’s 7th Framework Programme for Research and Technological Development (FP7) (Proposal No: 602541-2).
Author information
Authors and Affiliations
Contributions
B.Y. performed the statistical analyses and drafted and revised the article. All authors critically reviewed previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The trial was approved by research ethics committees in all participating countries.
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 22 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yildiz, B., Korfage, I.J., Deliens, L. et al. Self-efficacy of advanced cancer patients for participation in treatment-related decision-making in six European countries: the ACTION study. Support Care Cancer 31, 512 (2023). https://doi.org/10.1007/s00520-023-07974-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07974-2