Abstract
Aim
Non-surgical treatment for head and neck cancer (HNC) often results in severe toxicities, which are detrimental to a patient’s health and quality of life. There is limited published UK data on unplanned hospital admissions and reasons associated with admission. We aim to identify frequencies and reasons for unplanned hospital admissions, highlighting those patient groups who are most vulnerable.
Methods
A retrospective study of unplanned hospital admissions of HNC patients receiving non-surgical treatment was completed. An inpatient admission was defined as ≥ 1 night spent in the hospital. To test potential demographic and treatment predictors of inpatient admission, a multiple regression model was constructed using the endpoint measure (unplanned admission), as the dependent variable.
Results
A cohort of 216 patients was identified over a 7-month period, and 38 of these patients (17%) required an unplanned admission. Treatment type was the only statistically significant predictor of in-patient admission. The majority of admissions were patients receiving chemoradiotherapy (CRT) (58%) with predominant reasons for admission being nausea and vomiting (25.5%) and decreased oral intake/dehydration (30%). Of the patients admitted, 12 had a prophylactic PEG placed pre-treatment, and 18 of 26 admitted without prophylactic PEG required nasogastric tube feeding during their admission.
Discussion
Almost one-fifth of HNC patients over this time period required hospital admission; the majority of which can be attributed to treatment toxicities when receiving CRT. This is concurrent with other studies which review the impact of radiotherapy versus CRT. Increased support and monitoring, particularly focused on nutrition, are required for patients with HNC who receive CRT.
Key message
This article describes a retrospective review of a patient undergoing non-surgical treatment for head and neck cancer. These patients frequently require unplanned hospital admission. The results indicate that patients undergoing (chemo)radiotherapy are most vulnerable to deterioration and additional support focused on nutrition for these patients is indicated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemoradiotherapy is an important and effective treatment for head and neck cancer (HNC) but can often induce acute and chronic toxicities such as significant swallowing difficulties [1] that can be detrimental to patients’ health and quality of life. Although treatment schedules and regimes have sought to reduce toxicity and improve overall disease control [2], side effects such as mucositis, dysphagia and nausea and vomiting remain common [3]. As well as the incurred distress to patients and their families, these symptoms can lead to treatment breaks with high healthcare resource utilisation, such as unplanned hospital admission during treatment [4].
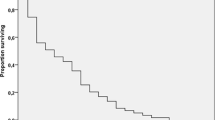
Current evidence affirms that treatment breaks are associated with poorer overall survival rates, patients with short (4–8 days) or long breaks (> 8 days) had lower absolute 4-year overall survival by 4 and 12% [5], with preliminary data suggesting that hospitalisation during radiotherapy for HNC may be an early marker for worse survival in this patient cohort [6]. A small number of studies in the USA suggest that hospitalisation during treatment is a relatively common occurrence, affecting up to a third of patients [7-9].
Identified risk factors associated with unplanned hospitalisation include treatment type, premorbid status and social circumstances. Systemic chemotherapy is an independent risk factor for treatment toxicity leading to unplanned admission as well as comorbidities (notably poorly controlled diabetes and chronic pulmonary disease) [7-9]. An individual’s social circumstances have also been shown to influence the likelihood of unplanned admission [6] with unmarried status purporting a greater admission risk. There is currently limited corroborative evidence from UK-based treatment cohorts in the literature, and both nutritional and oral intake status are risk factors of particular interest that warrant further impact assessment for admission.
Research in this area is vital to establish pre-emptive management pathways to minimise admission risk, reduce treatment interruptions and ultimately, improve patient outcomes. The aim of this study was to investigate the frequency, reasons and predictors of unplanned hospital admissions in HNC patients during non-surgical treatment modalities, with a specific focus on enteral feeding status and associated issues.
Methods
The study was registered and approved following institutional review (Clatterbridge Cancer Centre NHS Foundation Trust’s Audit Committee).
This was a single-centre cohort study of unplanned hospital admissions of HNC patients receiving non-surgical treatment modalities as part of their treatment package at a large tertiary oncology unit in North West England over a 7-month period. These admissions all occurred at varying time points during their treatment schedule.
All HNC referrals from 1.4.20 to 31.10.20 were screened, and those patients who underwent chemoradiotherapy in either primary, adjuvant or palliative settings were included in the analysis and entered into an anonymised electronic medical record system. This time period coincided with the first wave of the COVID-19 pandemic.
Data on patient demographics—age, gender and disease characteristics including tumour site and staging, TNM7 stage [10] treatment intent (curative or palliative) and the treatment modality (chemotherapy, radiotherapy, chemoradiotherapy)—was captured. Feeding tube status was recorded, including the timepoint of placement, pre or during treatment, and route of insertion—nasogastric or long-term enteral feeding tube (ie. percutaneous endoscopic gastrostomy (PEG), radiologically inserted percutaneous gastrostomy (RIG) or jejunostomy (JEJ)).
Unplanned admissions were categorised according to attendance at the “Clinical Decisions Unit” in the Clatterbridge Cancer Centre—where urgent medical care is provided during normal working hours. Reasons for unplanned admission are recorded by the medical professional who completes the initial assessment, and these reasons were categorised and coded using the terms: nausea and vomiting, nasogastric tube insertion, reduced oral intake/dehydration, infection, dysphagia/aspiration, deranged types of blood, etc. Data on admissions to other acute centres was not available.
Data was anonymised and screened for accuracy and consistency by a second internal reviewer.
Analysis
Analyses were carried out using SPSS for Windows version 24 (Chicago, Illinois, USA) [11]. Univariable analysis was initially performed to test each potential explanatory variable association with hospital admission, using Pearson’s Chi-square test for categorical explanatory variables. A conservative p value (0.1) for univariate analysis was used to take variables forward to binary logistic regression. A backwards selection procedure was used to determine the final model (criteria for entry p < 0.05 and for removal p > 0.1). The overall fit of the model was ascertained using the Hosmer and Lemeshow goodness of fit test.
Results
Patient characteristics
There were 216 patients identified as fitting the inclusion criteria during the six-month data collection period. Patient characteristics are summarised in Table 1.
Of this cohort, 38 patients (17%) required an unplanned admission during their treatment, and 9 of these patients had more than one admission with a total admission number of 47. The majority of admissions were patients receiving primary curative-intent chemoradiotherapy (CRT) (58%). For the majority of patients, the treatment intent was curative.
In total, 45 (21%) patients had a prophylactic gastrostomy tube (PEG/RIG/ JEJ) placed pre-treatment. Eighteen patients had a reactive nasogastric tube placed during an admission. Oropharynx was the most common tumour site for both PEG (n = 26) and NG placement (n = 7) followed by oral cavity (PEG (n = 7) and NGT (n = 5)).
Of the patients admitted (n = 38), 12 had a prophylactic gastrostomy placed pre-treatment, and 18 of 26 admitted without prophylactic enteral feeding required reactive nasogastric tube feeding during their admission.
Predictors of unplanned hospital admission
A binary logistic regression model was tested to see if independent variables (p > 0.1) from the univariate analysis (see Table 1) predicted an unplanned admission. The model was statistically significant χ2 = 18.47, p < 0.0001 (see Table 2). Patients treated with chemoradiation were more likely to be admitted than those receiving radiotherapy. Patients with T3-4 tumours were more likely to be admitted than those with T1-2 (25% vs. 15%). Age was also a significant variable. Just under one-third of patients aged < 50 years were admitted to hospital, compared with five per cent of those aged > 70 years.
The predominant reasons for admission being nausea and vomiting (34%) and decreased oral intake/dehydration (34%) are shown in Table 3.
Discussion
This study is the first UK-based cohort to our knowledge to report on unplanned hospital admissions for HNC patients receiving non-surgical treatment in a tertiary oncology centre. The frequency of admissions was lower than reported in other studies; 21% compared with 36% [7, 8] despite similar demographics. During the data collection period, the COVID-19 pandemic placed unprecedented pressure upon surgical services [12] with a subsequent increase in non-surgical management of HNC. Services aimed to reduce unplanned hospital admissions and the risk of COVID-19 exposure in this vulnerable group meaning that criteria for admission were likely temporarily elevated. There was advice published suggesting increased caution with the use of chemoradiotherapy with the majority of those patients over 60 years of age receiving radiotherapy alone or palliative RT (with reduced volumes) [13]. This may explain the reduction in unplanned admissions in our study compared to published cohorts. Despite this, almost one-fifth of HNC patients required hospital admission, and one-fifth of these had multiple admissions, similar to findings elsewhere. [7]
In keeping with previous work, patients receiving primary chemoradiotherapy were at greater risk of admission, many of whom had substantial deterioration in their diet and fluid intake [8, 9]. Reasons for chemoradiotherapy-related admissions include nausea and vomiting, dehydration/malnutrition, mucositis-related eating and drinking problems and pneumonia [14]. Although not coded for within our data, it is likely that reduced intake (one of the predominant reasons for admission in our study) was due to mucositis. Prevention and treatment strategies for mucositis should be a core part of clinical care and patient education [15]. A quarter of patients admitted also had nausea and vomiting with decreased oral intake/dehydration. Although implicated as a reason for admission in other cancer groups [16], nausea and vomiting appear more common in HNC patients (25% vs. 13%).
Importantly, placing a prophylactic gastrostomy did not seem to prevent hospital admission, as 27% of those with a prophylactic gastrostomy required admission compared with 15% of patients without a tube. Conversely, other centres have reported prophylactic gastrostomy does reduce unplanned admissions [17]. In our cohort, the decision to place a prophylactic gastrostomy was on a personalized case-by-case basis rather than a protocol-driven approach. The placement of prophylactic versus reactive feeding tubes has long been debated within the literature, and there are no nationally agreed selection criteria, with demonstrable variation in clinical practice [18]. Recent work to identify a clinical algorithm suggests performance status, tumour subsite, stage and nodal involvement, and platinum-based chemotherapy are predictors of the need for prophylactic gastrostomy [19, 20].
The tumour stage was also a predictor of an admission. Patients with higher staged tumours are more likely to have multi-modality treatment but may also present at diagnosis with significant weight loss, dysphagia and multiple co-morbidities rendering them more vulnerable to hospital admission [21, 22]. The analysis showed that age was an important variable, with those < 50 years having a higher percentage of admissions, although patient numbers in this category were low. Whether other previously identified predictors such as social circumstances influenced these findings is unknown [7].
There are a number of limitations in this study. We did not include co-morbidities, frailty score or social circumstances in our data collection as these were details not uniformly entered into medical records. These may be significant influencing factors [9, 23] and may help to identify vulnerable groups at an earlier stage. For future research, it would also be beneficial to review whether t-stage data and time point of treatment influenced admission in this group.
A better understanding of unplanned hospital admissions is important as such events can lead to a change in treatment plan e.g. reduced chemotherapy cycles, to manage severe side effects, thus negatively impacting overall survival [24]. In summary, whilst our admission rates appear favourable, findings suggest that concurrent chemoradiotherapy results in more severe toxicities and increased unplanned admission rates. Pre-emptive management of treatment side effects, such as mucositis, nausea and dysphagia, should be prioritised, particularly in vulnerable groups. Nutritional prehabilitation delivered before and during treatment may help to prevent deterioration, although evidence to support its effectiveness in HNC is lacking [25]. Regional data is also important in order to appropriately consent patients when discussing treatment plans. Patient’s nutrition and hydration status should be closely monitored throughout treatment. An increased focus on nutritional support may help to reduce the frequency of hospital utilisation in this patient group in the future.
References
Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, Leemans CR, Aaronson NK, Slotman BJ (2008) Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol 26(22):3770–3776. https://doi.org/10.1200/JCO.2007.14.6647
National Collaborating Centre for Cancer (UK) (2016) Cancer of the upper aerodigestive tract: assessment and management in people aged 16 and over. London: National Institute for Health and Care Excellence (UK)
Trotti A, Bellm LA, Epstein JB, Frame D, Fuchs HJ, Gwede CK, Komaroff E, Nalysnyk L, Zilberberg MD (2003) Mucositis incidence, severity and associated outcomes in patients with head and neck cancer receiving radiotherapy with or without chemotherapy: a systematic literature review. Radiother Oncol 66(3):253–262. https://doi.org/10.1016/s0167-8140(02)00404-8
Rosenthal DI (2007) Consequences of mucositis-induced treatment breaks and dose reductions on head and neck cancer treatment outcomes. J Support Oncol 5(9 Suppl 4):23–31
Xiang M, Gensheimer MF, Pollom EL, Holsinger FC, Colevas AD, Le QT, Beadle BM (2021) Prolongation of definitive head and neck cancer radiotherapy: survival impact and predisposing factors. Radiother Oncol 156:201–208. https://doi.org/10.1016/j.radonc.2020.12.025
Han HR, Hermann GM, Ma SJ, Iovoli AJ, Wooten KE, Arshad H, Gupta V, McSpadden RP, Kuriakose MA, Markiewicz MR, Chan JM, Platek ME, Ray AD, Gu F, Hicks WL Jr, Repasky EA, Singh AK (2020) Matched pair analysis to evaluate the impact of hospitalization during radiation therapy as an early marker of survival in head and neck cancer patients. Oral Oncol 109:104854. https://doi.org/10.1016/j.oraloncology.2020.104854
Moore ZR, Pham NL, Shah JL, Nedzi L, Sumer BD, Day AT, Khan SA, Sher DJ (2019) Risk of unplanned hospital encounters in patients treated with radiotherapy for head and neck squamous cell carcinoma. J Pain Symptom Manage 57(4):738-745.e3. https://doi.org/10.1016/j.jpainsymman.2018.12.337
Hazelden LA, Newman MJ, Shuey S, Waldfogel JM, Brown VT (2019) Evaluation of the head and neck cancer patient population and the incidence of hospitalization at an academic medical center. J Oncol Pharm Pract 25(2):333–338. https://doi.org/10.1177/1078155217735688
Ling DC, Kabolizadeh P, Heron DE, Ohr JP, Wang H, Johnson J, Kubicek GJ (2015) Incidence of hospitalization in patients with head and neck cancer treated with intensity-modulated radiation therapy. Head Neck 37(12):1750–1755. https://doi.org/10.1002/hed.23821
Sobin LH, Gospodarowicz MK, Wittekind C (eds) (2009) 7th edn. New York, Wiley
IBM Corp Released (2016) IBM SPSS statistics for Windows, Version 24.0. Armonk, NY: IBM Corp
NHS England and NHS Improvement. Important and urgent – next steps on NHS response to COVID-19. In: https://www.england.nhs.uk/coronavirus/wpcontent/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-tocovid-19-letter-simon-stevens.pdf (last accessed on 28th September 2022)
Roques T, Prestwich R (n.d.) Head and neck cancer and COVID-19. Available from https://www.rcr.ac.uk/default/files/head-and-neck-cancer-treatment-covid-19.pdf (last accessed on 28th September 2022)
Givens DJ, Karnell LH, Gupta AK, Clamon GH, Pagedar NA, Chang KE, Van Daele DJ, Funk GF (2009) Adverse events associated with concurrent chemoradiation therapy in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 135(12):1209–1217. https://doi.org/10.1001/archoto.2009.174
Liu S, Zhao Q, Zheng Z, Liu Z, Meng L, Dong L, Jiang X (2021) Status of treatment and prophylaxis for radiation-induced oral mucositis in patients with head and neck cancer. Front Oncol 11:642575. https://doi.org/10.3389/fonc.2021.642575
Gibson S, McConigley R (2016) Unplanned oncology admissions within 14 days of non-surgical discharge: a retrospective study. Support Care Cancer 24(1):311–317. https://doi.org/10.1007/s00520-015-2786-6
Brown TE, Banks MD, Hughes BGM, Lin CY, Kenny LM, Bauer JD (2018) Comparison of nutritional and clinical outcomes in patients with head and neck cancer undergoing chemoradiotherapy utilizing prophylactic versus reactive nutrition support approaches. J Acad Nutr Diet 118(4):627–636. https://doi.org/10.1016/j.jand.2016.10.013
Moor JW, Patterson J, Kelly C, Paleri V (2010) Prophylactic gastrostomy before chemoradiation in advanced head and neck cancer: a multiprofessional web-based survey to identify current practice and to analyse decision making. Clin Oncol (R Coll Radiol) 22(3):192–198. https://doi.org/10.1016/j.clon.2010.01.008
Kano S, Tsushima N, Suzuki T, Hamada S, Yokokawa T, Idogawa H, Yasuda K, Minatogawa H, Dekura Y, Aoyama H, Homma A (2021) Predictors of the need for prophylactic percutaneous endoscopic gastrostomy in head and neck cancer patients treated with concurrent chemoradiotherapy. Int J Clin Oncol 26(7):1179–1187. https://doi.org/10.1007/s10147-021-01889-w
Willemsen ACH, Kok A, van Kuijk SMJ, Baijens LWJ, de Bree R, Devriese LA, Hoebers FJP, Lalisang RI, Schols AMWJ, Terhaard CHJ, Hoeben A (2020) Prediction model for tube feeding dependency during chemoradiotherapy for at least four weeks in head and neck cancer patients: a tool for prophylactic gastrostomy decision making. Clin Nutr 39(8):2600–2608. https://doi.org/10.1016/j.clnu.2019.11.033
Patterson JM, McColl E, Carding PN, Hildreth AJ, Kelly C, Wilson JA (2014) Swallowing in the first year after chemoradiotherapy for head and neck cancer: clinician- and patient-reported outcomes. Head Neck 36(3):352–358. https://doi.org/10.1002/hed.23306
Eskander A, Krzyzanowska MK, Fischer HD, Liu N, Austin PC, Irish JC, Enepekides DJ, Lee J, Gutierrez E, Lockhart E, Raphael M, Singh S (2018) Emergency department visits and unplanned hospitalizations in the treatment period for head and neck cancer patients treated with curative intent: a population-based analysis. Oral Oncol 83:107–114. https://doi.org/10.1016/j.oraloncology.2018.06.011
Waddle MR, Chen RC, Arastu NH, Green RL, Jackson M, Qaqish BF, Camporeale J, Collichio FA, Marks LB (2015) Unanticipated hospital admissions during or soon after radiation therapy: incidence and predictive factors. Pract Radiat Oncol 5(3):e245–e253. https://doi.org/10.1016/j.prro.2014.08.004
Datema FR, Ferrier MB, de Baatenburg Jong RJ (2011) Impact of severe malnutrition on short-term mortality and overall survival in head and neck cancer. Oral Oncol 47(9):910–914. https://doi.org/10.1016/j.oraloncology.2011.06.510
Cantwell LA, Fahy E, Walters ER, Patterson JM (2022) Nutritional prehabilitation in head and neck cancer: a systematic review. Support Care Cancer 30(11):8831–8843. https://doi.org/10.1007/s00520-022-07239-4
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by Emer Fahy. The first draft of the manuscript was written by Emer Fahy, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fahy, E., Brooker, R.C., Fleming, J.C. et al. A review of unplanned admissions in head and neck cancer patients undergoing oncological treatment. Support Care Cancer 31, 328 (2023). https://doi.org/10.1007/s00520-023-07770-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07770-y