Abstract
Purpose
Insomnia is frequent in patients with advanced cancer, and a variety of pharmacological agents is used to treat this condition. Still, few clinical trials have investigated the effectiveness of pharmacological sleep therapies in this patient group. We aimed to study the short-term effectiveness of zopiclone on sleep quality in patients with advanced cancer who report insomnia.
Methods
A randomized, double-blind, placebo-controlled, parallel-group, multicenter, phase IV clinical trial in adult patients with metastatic malignant disease and insomnia. Patients were treated with zopiclone or placebo for six subsequent nights. Primary end point was patient-reported sleep quality during the final study night (NRS 0–10). Secondary end points were patient-reported sleep onset latency (SOL) and total sleep time (TST).
Results
Forty-one patients were randomized, with 18 being analyzed in the zopiclone group and 21 in the placebo group. Median age was 66, median Karnofsky performance score was 80, and 56% were male. Mean sleep quality at end of study was 2.9 (CI 2.3 to 3.8) in the zopiclone group and 4.5 (CI 3.6 to 5.4) in the placebo group (p = 0.021). At end of study, SOL was significantly different between the treatment groups: zopiclone 29 min (CI 13 to 51) and placebo 62 min (CI 40 to 87) (p = 0.045). TST was not significantly different across groups: zopiclone 449 min (403 to 496) and placebo 411 min (CI 380 to 440) (p = 0.167).
Conclusion
Zopiclone improved short-term patient-reported sleep quality in this cohort of patients with advanced cancer.
Trial registration
ClinicalTrials.gov Identifier: NCT02807922.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep disturbances are frequent in patients with advanced cancer, with insomnia being the most prevalent sleep disorder [1]. The cancer disease and cancer treatments place patients at increased risk for disruption of normal behaviors and physiological states that are associated with restful sleep [2, 3]. Insomnia may occur at various points in the patient’s disease and treatment trajectory [4, 5].
Treatment for sleep disturbances in advanced cancer should address the multifactorial and manageable causes of sleep disturbances [6]. However, relief of symptoms such as pain, fatigue, anxiety, and depression does not necessarily lead to improvement of insomnia [2, 7]. Thus, in cancer patients as in other populations, sleep specific interventions must be considered. The recommended therapy for sleep disturbances is a stepwise approach starting with non-pharmacological intervention with cognitive behavior therapy for insomnia (CBT-I). If these are ineffective, pharmacological sleep interventions are a next step [6, 8]. A limitation for the implementation of CBT-I in cancer clinics is the lack of health professionals formally trained in these techniques. In addition, the number of CBT-I sessions, usually four to eight, might be too demanding for patients during cancer treatment. Thus, for patients with advanced cancer, pharmacological therapy is often used because of its rapid and relatively immediate effects [9, 10].
Several classes of sleep medications are used to treat sleep disturbances in cancer patients [11]. In a multicenter European study, the non-benzodiazepine hypnotic agent, zopiclone, was used by 348 of 2282 patients and was the most frequently used hypnotic agent in these patients with advanced cancer [11]. Zopiclone is one of the currently available therapies of insomnia. However, there is limited data from randomized controlled trials about the efficiency of hypnotic drugs in patients with advanced cancer, indicating a lack of evidence-based knowledge in the pharmacological treatment of insomnia in this group [2, 6, 8]. Patients with advanced cancer are in a different clinical situation than other patients with sleep disturbances, due to the limited life expectancy and the complexity of symptoms. Thus, findings from other patient populations cannot be extrapolated. In this group of patients, a well-designed randomized controlled trial is needed to determine the effectiveness of zopiclone on sleep quality to advise the clinical management of insomnia in palliative care populations.
On the basis of the lack of knowledge in pharmacological treatment of insomnia in patients with advanced cancer, we designed a double-blind, placebo-controlled, parallel-group RCT with the primary objective to evaluate the short-term effectiveness of zopiclone on self-reported sleep quality in patients with advanced metastatic cancer who report insomnia [12]. The secondary objectives were to study the effectiveness of zopiclone on mean self-reported sleep onset latency (SOL) and total sleep time (TST).
Methods
The trial was a randomized, double-blind, placebo-controlled, parallel-group, phase IV clinical trial. Three palliative care and outpatient oncology services in Norway participated in the study: St. Olavs hospital, Trondheim University Hospital, Vestfold Hospital Trust, Tønsberg, and Telemark Hospital Trust, Skien.
Participants
Eligible adult patients had verified malignant metastatic or disseminated disease (stage IV) and insomnia. Insomnia syndrome in the context of cancer was defined as self-reported difficulty initiating sleep (greater than 30 min to sleep onset) and/or difficulty maintaining sleep (greater than a 30-min nocturnal waking time) and/or waking up earlier than desired, for at least 3 nights per week. Furthermore, sleep problems should significantly impair daytime functioning, e.g., altered level of functioning, feeling tired, and lack of energy, as reported by the patients [13]. Main exclusion criteria were ongoing or previous treatment (within last 4 weeks) for more than 3 consecutive days with medications given for insomnia, adverse reactions to zopiclone, history of substance abuse, and concomitant use of rifampicin or erythromycin. Informed consent was signed before any study related procedures were done. Patients were randomized to either the zopiclone arm or the placebo arm using the web-based randomization system administered by the Clinical Research Unit, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology (NTNU)/St. Olavs hospital, Trondheim University Hospital.
Intervention
Patients were randomized to zopiclone “Actavis” or placebo for 6 subsequent nights. The initial dose of zopiclone/placebo was 3.75 mg (dose level I), self-administered 30 min before bedtime, started after 1 night (baseline) with sleep quality assessment and symptom assessment. Patient-reported sleep quality was assessed by study personnel by phone after 2 and 4 nights on study medication, using a numerical rating scale (NRS) “Please circle the number that best describes how you feel now,” where 0 = best sleep, and 10 = worst possible sleep. If the NRS was ≥ 4 after 2 nights, the dose was increased to 5 mg (dose level II) zopiclone/placebo, and similarly if the NRS was still ≥ 4 after 4 nights, the dose was further increased 7.5 mg (dose level III) zopiclone/placebo. If patient-reported sleep quality was NRS < 4 after 2 or 4 nights, the patient would continue with the same dose. Dose titration was recorded in the WebCRF. Kragerø Tablettproduksjon AS, Norway produced, blinded, packed, and labeled identical looking and identical tasting zopiclone and placebo tablets. The study drug was blinded for patients, sites, and study personnel. The Unit for Applied Clinical Research, NTNU was external monitor for the trial.
End points and assessments
The primary end point was patient-reported sleep quality during the final study night with treatment (night 6), assessed at daytime after night 6 using NRS 0–10, 0 = best sleep, 10 = worst possible sleep. Secondary end points were patient-reported sleep onset latency (SOL, i.e., how many minutes it takes to fall asleep starting from the moment of intention to fall asleep) and total sleep time (TST, i.e., the actual time slept in minutes) the final study night with treatment (night 6). All end points were reported in a sleep diary. Patients completed the sleep diary every morning when getting up. Patient-reported overall sleep quality, a predefined explorative end point, was assessed at baseline and at daytime after night 6 using the Pittsburgh Sleep Quality Index (PSQI) which in this study was modified to assess sleep quality during the past week [14]. Cancer-related symptoms (pain, drowsiness, tiredness, nausea, lack of appetite, shortness of breath, depression, anxiety, well-being, constipation, and vomiting) were measured using a NRS 0–10 from the European Association for Palliative Care (EAPC) basic dataset [15]. At the end of treatment, the patients were asked “How satisfied were you with the effect of the sleep medication”? with response categories: “not satisfied” (i.e., not at all satisfied, dissatisfied, and neither satisfied nor dissatisfied) or “satisfied” (i.e., satisfied and very satisfied) to assess their global perceived treatment benefits [16]. Performance status was rated by the Karnofsky performance status (KPS) [17], and sociodemographic and medical characteristics were obtained from the medical records by study personnel.
Statistical analysis
The estimated sample size was 33 patients needed in each group, using a significance level of 5% and 80% power. The predefined minimal clinical important difference between the zopiclone and placebo group was 2 for the primary outcome sleep quality, scored on the NRS 0–10. Sample size calculations are presented in the protocol paper [12]. Demographic variables are reported as means with standard deviations (SD) or frequencies. In the comparison of sleep quality between the two groups after night 6 of using the study drug, independent Student’s t-test was used for continues variables. Additionally, a general linear model (ANCOVA) including baseline values of sleep quality as a covariate was used to assess differences in sleep quality at night 6 between the intervention group and the control group. The Pearsons Chi square test was used to compare the number of patients in each treatment group reporting satisfaction with study treatment. Intention-to-treat analyzes were used including all randomized patients regardless of protocol adherence. A two-sided P value ≤ 0.05 was considered statistically significant. Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 27 Armonk, NY: IBM Corp.
Results
Baseline characteristics and cancer-related symptoms
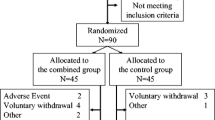
From January 2017 to April 2020, a total of 278 patients were screened for eligibility. Main reasons for non-participation were ongoing treatment with medication given for insomnia (n = 102) and no presence of metastatic disease (n = 65), (Fig. 1). Forty-one patients were randomized to zopiclone or placebo; 20 were allocated to the zopiclone group and 21 to the placebo group, of which 18 could be evaluated in the zopiclone group and 21 in the placebo group (Fig. 1). Overall, median age was 66 years (range 26–79), median Karnofsky performance score was 80, and 56% of patients were male. Table 1 presents baseline demographic and clinical characteristics for each treatment group. The presence of cancer-related symptoms (mean scores, SD) at baseline and end of study is presented in Table 2.
Patient-reported sleep quality
There were no baseline differences in mean patient-reported sleep quality (NRS 0–10) between the zopiclone group and the placebo group (4.9; 95%CI 4.2 to 5.6 vs. 5.4; 95%CI 4.5 to 6.0, p = 0.528). At night 6 with treatment, there was a statistically significant difference in sleep quality between the study groups (mean difference, 1.5; 95% CI, 0.3 to 2.8), with a mean NRS 2.9 (95% CI 2.3 to 3.8) in the zopiclone group and a mean NRS 4.5 (95% CI 3.6 to 5.4) in the placebo group (p = 0.021, Table 3). At night 6 with treatment, patient-reported SOL was 29 min (CI 13 to 51) in the zopiclone group and 62 min (CI 40 to 87) in the placebo group (p = 0.045), with a mean difference 33 min; 95% CI − 0.6 to 67.4). Total sleep time at night 6 with treatment was 449 min (CI 403 to 496) in the zopiclone group and 411 min in the placebo group (95% CI 380 to 440), (p = 0.167), with a mean difference − 38 min (95% CI − 93 to 17). Controlling for baseline scores on sleep (NRS 0–10) also showed significant differences in the sleep quality with zopiclone compared with placebo (ANCOVA, F = 5.64, p = 0.023) at night 6 with treatment. Figure 2 shows sleep quality (NRS 0–10) for baseline and study drug nights 1–6 by treatment group.
At baseline, the mean PSQI global score was 10.1 (CI 9 to11) in the zopiclone group and 9.4 (CI 8 to 11) in the placebo group. At end of the study, there were no significant difference in the global PSQI score between the groups with 8.13 (CI 6 to 10) in the zopiclone group vs. 9.7 (CI 6 to 10) in the placebo group (p = 0.179).
Dose titration
All patients started with 3.75 mg (dose level I). In the zopiclone group, three patients (16.7%) continued this dose level, seven (38.9%) increased to dose level II (5 mg), and eight (44.4%) increased to 7.5 mg (dose level III) during the intervention. In the placebo group, one patient (4.8%) continued dose level I, eight (38.1%) increased to dose level II, and 12 (57.1%) increased to dose level III.
Safety and satisfaction
In the zopiclone group, one patient reported temporary dizziness (reported at night 5 with treatment). In the placebo group, one patient reported transient headache (reported at night 4 with treatment). No serious adverse events was reported in either group. Patients’ global perceived treatment benefits assessed at the end of treatment showed that 62.5% in the zopiclone group were satisfied with the effect of the sleep medication (i.e., satisfied and very satisfied) vs. 15.4% in the placebo group (p = 0.027). In total, 15 (38.5%) reported “neither satisfied” nor “dis-satisfied” with the effect of the study drug.
Discussion
This randomized, double-blinded, placebo-controlled, parallel-group, multicenter, clinical trial was designed to study the short-term effectiveness of zopiclone on patient-reported sleep quality in patients with advanced cancer who report insomnia. After six nights of intervention, patients receiving zopiclone reported significantly better sleep quality as compared with patients receiving placebo, adjusted for baseline sleep quality.
Two systematic reviews, one from 2013 and another from 2020, on the management of sleep disturbance in cancer identified no RCTs investigating pharmacological interventions for sleep disturbance in palliative cancer care [2, 8]. Nevertheless, a variety of pharmacological agents are in use to treat insomnia in patients with cancer [8]. Benzodiazepines, with zolpidem and trazodone as the most frequently used drugs in palliative care, are reported by patients to be helpful at the time of prescription [2, 18]. However, due to the absence of clinical trials with randomization and a placebo comparison group, the effectiveness of these drugs was previously unproven for use against insomnia in cancer patients [2, 18,19,20,21]. The present study is, to the best of our knowledge, the first RCT that presents the effectiveness of zopiclone in patients with advanced cancer.
Our results agree with trials which have demonstrated the effectiveness and safety of zopiclone in other populations [22,23,24,25]. A recent review including older adults with and without comorbidities demonstrated that zopiclone had positive effects on sleep quality leading to significant reduction in sleep latency, which corresponds with our results [23]. The eligibility criteria for this review were limited to older adults (≥ 60), which is comparable to the median age of 66 years in our trial. Another review including older adults with sleep disorders, with a mean age of 70 in all 24 trials, also demonstrated positive effects of zopiclone [26].
In addition to SOL and sleep quality, total sleep time is a commonly used outcome in studies of hypnotic drugs [23]. In the present trial, patients receiving zopiclone reported 38 min longer sleep duration as compared to patients receiving placebo. The difference between groups was not statistically significant, but might be clinically significant, as increased sleep duration between 23 and 29 min by the use of zopiclone is previously reported being effective to treat insomnia in older adults [23, 24]. On the other hand, an RCT comparing zopiclone, cognitive behavioral therapy, and placebo did not identify any difference in TST between the treatment arms [27]. Moreover, a meta-analysis demonstrated that several other hypnotic drugs such as doxepin, temazepam, eszopiclone, zolpidem, suvorexant, zaleplon, and triazolam yield significantly longer sleep duration than zopiclone, when compared to placebo [24].
Patients with advanced cancer represent a heterogeneous group of patients, differing in age, diagnoses, symptom burden, and expected survival time [15]. Regardless of these diversities, however, improving insomnia is an essential factor for optimizing of well-being and relief of symptoms in this group of patients. Cancer-related symptoms assessed on a 0–10 NRS at baseline and after six nights of intervention demonstrated a relative low intensity of pain, anxiety, and depression as compared to other studies in palliative care [18, 28,29,30]. As such, the findings from the present trial are applicable to patients with advanced cancer reporting mild cancer-related symptoms. The effectiveness of zopiclone on sleep quality in patients with higher symptom intensity might differ from the results from our trial.
To manage insomnia successfully, cognitive behavior therapy for insomnia (CBT-I) is considered the first-line treatment in adults of any age [31, 32]. This treatment incorporates cognitive and behavior-change techniques and targets dysfunctional attitudes, beliefs, and habits involving sleep [33]. It usually consists of psychoeducation/sleep hygiene, relaxation training, stimulus control therapy, sleep restriction therapy, and cognitive therapy [34]. In patients with cancer, CBT-I has been found to be associated with clinically and statistically significant improvements in patient-reported sleep outcomes [33]. However, given the lack of trained mental health professionals in palliative cancer care, the implementation of CBT-I is challenging. Besides, pharmacological interventions are often needed to provide immediate effective relief of symptoms, and when life expectancy is limited and patients experience complex symptoms such as pain and other problems, the goal of symptomatic relief overrides the concerns of long-term side effects [35]. Thus, for patients with advanced cancer, pharmacological therapy is often used as the first step after interventions directed at symptom control to remove the potential causative conditions for insomnia [18].
This trial has some major strengths. First, the trial is designed with methodological rigor, using a randomized, double-blind, placebo-controlled design, with patient recruitment at three centers. Second, the study included a titration protocol which recognized that patients need different doses. Third, the short intervention period of six nights with zopiclone or placebo, made it ethically feasible for patients to participate despite the blinding. Moreover, it kept the drop-out rate to a minimum, which is an important consideration in palliative care research [36].
The main limitation is the number of patients enrolled. Because of slow recruitment the trial was stopped before the predefined target of patients was reached. However, the risk for a potential type two error was mitigated by the statistically significant difference for the predefined primary end point. In fact, we believe that an interim analysis would have led to the trial being discontinued given the favorable outcomes. For this study, as in many other RCTs in palliative care studies, inclusion is difficult [37]. To improve palliative care, evidence-based knowledge on the effect of therapeutic interventions is needed, and measures should be taken to increase the feasibility of controlled trials also in this population [38,39,40]. Another limitation is that this study cannot report the effectiveness of long-term therapy with zopiclone. Nevertheless, study results showed positive effects of short-term use of zopiclone, indicating improved patient-reported sleep quality and reduced patient-reported sleep onset latency in patients with advanced cancer.
Conclusion
In conclusion, this trial demonstrated in a randomized double-blind, placebo-controlled clinical trial that patient-reported sleep quality was significantly improved in cancer patients receiving short-term treatment with zopiclone compared to placebo. Future research should investigate the effectiveness of long-term treatment of zopiclone on sleep quality in patients with advanced cancer.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sateia MJ, Lang BJ (2008) Sleep and cancer: recent developments. Curr Oncol Rep 10:309–318
Nzwalo I, Aboim MA, Joaquim N, Marreiros A, Nzwalo H (2020) Systematic review of the prevalence, predictors, and treatment of insomnia in palliative care. Am J Hosp Palliat Care 37:957–969
Graci G (2005) Pathogenesis and management of cancer-related insomnia. J Support Oncol 3:349–359
Jakobsen G, Engstrom M, Fayers P, Hjermstad MJ, Kaasa S, Kloke M, Sabatowski R, Klepstad P (2018) Sleep quality with WHO Step III opioid use for cancer pain. BMJ Support Palliat Care 9(3):307–315
Verkissen MN, Hjermstad MJ, Van Belle S, Kaasa S, Deliens L, Pardon K (2019) Quality of life and symptom intensity over time in people with cancer receiving palliative care: results from the international European Palliative Care Cancer Symptom study. PLoS One 14:e0222988
Induru RR, Walsh D (2014) Cancer-related insomnia. Am J Hosp Palliat Care 31:777–785
Nieder C, Dalhaug A, Haukland E, Engljähringer K (2018) Patient-reported symptom burden, rate of completion of palliative radiotherapy and 30-day mortality in two groups of cancer patients managed with or without additional care by a multidisciplinary palliative care team. Anticancer Res 38:2271–2275
Howell D, Oliver TK, Keller-Olaman S, Davidson JR, Garland S, Samuels C, Savard J, Harris C, Aubin M, Olson K, Sussman J, MacFarlane J, Taylor C (2014) Sleep disturbance in adults with cancer: a systematic review of evidence for best practices in assessment and management for clinical practice. Ann Oncol 25:791–800
Kvale EA, Shuster JL (2006) Sleep disturbance in supportive care of cancer: a review. J Palliat Med 9:437–450
Guzman-Marin R, Avidan AY (2015) Sleep disorders in patients with cancer. The Journal of community and supportive oncology 13:148–155
Kotlinska-Lemieszek A, Paulsen O, Kaasa S, Klepstad P (2014) Polypharmacy in patients with advanced cancer and pain: a European cross-sectional study of 2282 patients. J Pain Symptom Manage 48:1145–1159
Jakobsen G, Engstrøm M, Paulsen Ø, Sjue K, Raj SX, Thronæs M, Hjermstad MJ, Kaasa S, Fayers P, Klepstad P (2018) Zopiclone versus placebo for short-term treatment of insomnia in patients with advanced cancer: study protocol for a double-blind, randomized, placebo-controlled, clinical multicenter trial. Trials 19:707
Savard J, Morin CM (2001) Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol 19:895–908
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Sigurdardottir KR, Kaasa S, Rosland JH, Bausewein C, Radbruch L, Haugen DF, on behalf of P, (2014) The European Association for Palliative Care basic dataset to describe a palliative care cancer population: results from an international Delphi process. Palliat Med 28:463–473
Omvik S, Pallesen S, Bjorvatn B, Sivertsen B, Havik OE, Nordhus IH (2010) Patient characteristics and predictors of sleep medication use. Int Clin Psychopharmacol 25:91–100
Karnofsky DA, Abelmann WH, Craver LF, Burchenal JH (1948) The use of nitrogen mustards in the palliative treatment of carcinoma. Cancer 1:23
Hugel H, Ellershaw JE, Cook L, Skinner J, Irvine C (2004) The prevalence, key causes and management of insomnia in palliative care patients. J Pain Symptom Manage 27:316–321
Sela RA, Watanabe S, Nekolaichuk CL (2005) Sleep disturbances in palliative cancer patients attending a pain and symptom control clinic. Palliat Support Care 3:23–31
Claxton RN, Blackhall L, Weisbord SD, Holley JL (2010) Undertreatment of symptoms in patients on maintenance hemodialysis. J Pain Symptom Manage 39:211–218
Gómez-Batiste X, Porta-Sales J, Espinosa-Rojas J, Pascual-López A, Tuca A, Rodriguez J (2010) Effectiveness of palliative care services in symptom control of patients with advanced terminal cancer: a spanish, multicenter, prospective, quasi-experimental, pre-post study. J Pain Symptom Manage 40:652–660
Nutt DJ, Stahl SM (2010) Searching for perfect sleep: the continuing evolution of GABAA receptor modulators as hypnotics. J Psychopharmacology (Oxford, England) 24:1601–1612
Louzada LL, Machado FV, Nóbrega OT, Camargos EF (2021) Zopiclone to treat insomnia in older adults: a systematic review. Eur Neuropsychopharmacol 50:75–92
Chiu HY, Lee HC, Liu JW, Hua SJ, Chen PY, Tsai PS, Tu YK (2021) Comparative efficacy and safety of hypnotics for insomnia in older adults: a systematic review and network meta-analysis. Sleep 44
Rios P, Cardoso R, Morra D, Nincic V, Goodarzi Z, Farah B, Harricharan S, Morin CM, Leech J, Straus SE, Tricco AC (2019) Comparative effectiveness and safety of pharmacological and non-pharmacological interventions for insomnia: an overview of reviews Syst Rev 8:281
Dolder C, Nelson M, McKinsey J (2007) Use of non-benzodiazepine hypnotics in the elderly: are all agents the same? CNS Drugs 21:389–405
Sivertsen B, Omvik S, Pallesen S, Bjorvatn B, Havik OE, Kvale G, Nielsen GH, Nordhus IH (2006) Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial. JAMA 295:2851–2858
George GC, Iwuanyanwu EC, Anderson KO, Yusuf A, Zinner RG, Piha-Paul SA, Tsimberidou AM, Naing A, Fu S, Janku F, Subbiah V, Cleeland CS, Mendoza TR, Hong DS (2016) Sleep quality and its association with fatigue, symptom burden, and mood in patients with advanced cancer in a clinic for early-phase oncology clinical trials. Cancer 122:3401–3409
Nishiura M, Tamura A, Nagai H, Matsushima E (2015) Assessment of sleep disturbance in lung cancer patients: relationship between sleep disturbance and pain, fatigue, quality of life, and psychological distress. Palliat Support Care 13:575–581
Mercadante S, Aielli F, Adile C, Ferrera P, Valle A, Cartoni C, Pizzuto M, Caruselli A, Parsi R, Cortegiani A, Masedu F, Valenti M, Ficorella C, Porzio G (2015) Sleep disturbances in patients with advanced cancer in different palliative care settings. J Pain Symptom Manage 50:786–792
Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, Espie CA, Garcia-Borreguero D, Gjerstad M, Goncalves M, Hertenstein E, Jansson-Frojmark M, Jennum PJ, Leger D, Nissen C, Parrino L, Paunio T, Pevernagie D, Verbraecken J, Weess HG, Wichniak A, Zavalko I, Arnardottir ES, Deleanu OC, Strazisar B, Zoetmulder M, Spiegelhalder K (2017) European guideline for the diagnosis and treatment of insomnia. J Sleep Res 26:675–700
Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M (2008) Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med 4:487–504
Garland SN, Johnson JA, Savard J, Gehrman P, Perlis M, Carlson L, Campbell T (2014) Sleeping well with cancer: a systematic review of cognitive behavioral therapy for insomnia in cancer patients. Neuropsychiatr Dis Treat 10:1113–1124
Riemann D, Perlis ML (2009) The treatments of chronic insomnia: a review of benzodiazepine receptor agonists and psychological and behavioral therapies. Sleep Med Rev 13:205–214
Kaneishi K, Kawabata M, Morita T (2015) Single-dose subcutaneous benzodiazepines for insomnia in patients with advanced cancer. J Pain Symptom Manage 49:e1-2
Hui D, Glitza I, Chisholm G, Yennu S, Bruera E (2013) Attrition rates, reasons, and predictive factors in supportive care and palliative oncology clinical trials. Cancer 119:1098–1105
Boland J, Currow DC, Wilcock A, Tieman J, Hussain JA, Pitsillides C, Abernethy AP, Johnson MJ (2015) A systematic review of strategies used to increase recruitment of people with cancer or organ failure into clinical trials: implications for palliative care research. J Pain Symptom Manage 49:762-772.e765
Kars MC, van Thiel GJ, van der Graaf R, Moors M, de Graeff A, van Delden JJ (2016) A systematic review of reasons for gatekeeping in palliative care research. Palliat Med 30:533–548
Kaasa S, Hjermstad MJ, Loge JH (2006) Methodological and structural challenges in palliative care research: how have we fared in the last decades? Palliat Med 20:727–734
Bouca-Machado R, Rosario M, Alarcao J, Correia-Guedes L, Abreu D, Ferreira JJ (2017) Clinical trials in palliative care: a systematic review of their methodological characteristics and of the quality of their reporting. BMC Palliat Care 16:10
Acknowledgements
The authors would like to thank patients for participating in the study and the personnel at the participating centers for their contribution in recruiting patients and collecting data. We would like to thank Berit Bjelkåsen and Ann Jorunn Sandstå at the Clinical Research Unit, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology (NTNU)/St. Olavs hospital, Trondheim University Hospital for the support on randomization, WebCRF, and monitoring.
Funding
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital) This research was funded by The Liaison Committee for education, research, and innovation in Central Norway between the Regional Health Authority and the Norwegian University of Science and Technology [46083200] and the Cancer Foundation, St. Olavs Hospital, Trondheim University Hospital, Trondheim, Norway [15/9116–115/NISLIN], and Norwegian Competence Center for Sleep Disorders, Haukeland University Hospital, Bergen, Norway. The funders have no role in the trial design, collection, analysis, and interpretation of data, or writing the manuscript. No commercial interests are involved in the trial.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. GJ, KS, and ØP collected the data, which were analyzed, by GJ, ØP, and PK. Data were interpreted by GJ, KS, MJH, ØP, and PK, and confirmed by all authors. All authors were involved in the manuscript writing and critically appraised the manuscript before providing final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This trial is conducted in accordance with ethical principles that have their origin in the Declaration of Helsinki and are consistent with ICH/Good Clinical Practice and applicable regulatory requirements. The Regional Committee for Medical and Health Research Ethics, Section C, South East Norway, approved the final version of the protocol (Sleep RCT_270215) prior to the start of the trial (approval number 2016/353).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jakobsen, G., Sjue, K., Paulsen, Ø. et al. Zopiclone versus placebo for short-term treatment of insomnia in patients with advanced cancer—a double-blind, randomized placebo-controlled clinical multicenter phase IV trial. Support Care Cancer 31, 60 (2023). https://doi.org/10.1007/s00520-022-07537-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07537-x