Abstract
Background
The final conversion ratios among opioids used for successful switching are unknown. The aim of this study was to determine the initial and final conversion ratios used for a successful opioid switching in cancer patients, and eventual associated factors.
Methods
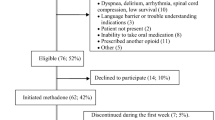
Ninety-five patients who were successfully switched were evaluated. The following data were collected: age, gender, Karnofsky performance score, primary cancer, cognitive function, the presence of neuropathic, and incident pain. Opioids, route of administration, and their doses expressed in oral morphine equivalents used before OS were recorded as well as opioids use for starting opioid switching, and at time of stabilization. Physical and psychological symptoms were routinely evaluated by Edmonton Symptom Assessment Scale.
Results
No statistical changes were observed between the initial conversion ratios and those achieved at time of stabilization for all the sequences of opioid switching. When considering patients switched to methadone, there was no association between factors taken into considerations.
Conclusion
Opioid switching is a highly effective and safe technique, improving analgesia and reducing the opioid-related symptom burden. The final conversion ratios were not different from those used for starting opioid switching. Patients receiving higher doses of opioids should be carefully monitored for individual and unexpected responses in an experienced palliative care unit, particularly those switched to methadone. Future studies should provide data regarding the profile of patients with difficult pain to be hospitalized.
Similar content being viewed by others
Data availability
Data are available on request.
References
van den Beuken-van Everdingen MH et al (2016) Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage 51:1070–1090
Portenoy RK, Ahmed E (2014) Principles of opioid use in cancer pain. J Clin Oncol 32:1662–1670
Mercadante S (2019) The patient with difficult cancer pain. Cancers (Basel) 11:565
Mercadante S (1999) Opioid rotation for cancer pain: rationale and clinical aspects. Cancer 86:1856–1866
Mercadante S, Bruera E (2016) Opioid switching in cancer pain: from the beginning to nowadays. E Crit Rev Oncol Hematol 99:241–8
Mercadante S, Caraceni A (2011) Conversion ratios for opioid switching in the treatment of cancer pain: a systematic review. Palliat Med 25:504–559
Knotkova H, Fine PG, Portenoy RK (2009) Opioid rotation: the science and the limitations of the equianalgesic dose table. J Pain Symptom Manage 38:426–439
McPherson ML (2020) Why equianalgesic tables are only part of the answer to equianalgesia. Ann Palliat Med 9:537–541
Benítez-Rosario MA, Salinas-Martín A, Aguirre-Jaime A, Pérez-Méndez L, Feria M (2009) Morphine-methadone opioid rotation in cancer patients: analysis of dose ratio predicting factors. J Pain Symptom Manage 37:1061–1068
Reddy A, Sinclair C, Crawford GB et al (2022) Opioid rotation and conversion ratios used by palliative care professionals: an international survey. J Palliat Med 2022 5. https://doi.org/10.1089/jpm.2022.0266 Online ahead of print
Mercadante S, Lo Cascio A, Adile C, Ferrera P, Casuccio A (2022) Maddalena Opioid Switching Score (MOSS) in patients with cancer pain. Pain 2022 2. https://doi.org/10.1097/j.pain.0000000000002669. Online ahead of print
Mercadante S, Ferrera P, Villari P et al (2009) Frequency, indications, outcomes, and predictive factors of opioid switching in an acute palliative care unit. J Pain Symptom Manage 37:632–641
Mercadante S (2012) Stop and go strategy for opioid switching requires flexibility. Eur J Cancer 48:944–945
Bouassirha D, Attal N, Alchaar H et al (2005) Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 114:29–36
Mulvey MR, Boland EG, Bouhassira D et al (2017) Neuropathic pain in cancer: systematic review, performance of screening tools and analysis of symptom profiles. Br J Anaesth 119:765–774
Mercadante S, Portenoy RK (2016) Breakthrough cancer pain: twenty-five years of study. Pain 157:2657–2663
Mercadante S, Coluzzi F (2021) Factors influencing pain expression in patients with cancer: an expert opinion. Pain Ther 10:765–775
Hui D, Bruera E (2017) The Edmonton Symptom Assessment System 25 years later: past, present, and future developments. J Pain Symptom Manage 53:630–643
Breibart W, Rosenfeld B, Roth A et al (1997) The Memorial Delrium Assessment Scale. J Pain Symptom Manage 13:128–137
Pereira J, Lawlor P, Vigano A, Dorgan M, Bruera E (2001) Equianalgesic dose ratios for opioids: a critical review and proposals for long-term dosing. J Pain Symptom Manage 22:672–678
Reddy A, Yennurajalingam S, Pulivarthi K et al (2013) Frequency, outcome, and predictors of success within 6 weeks of an opioid rotation among outpatients with cancer receiving strong opioids. Oncologist 18:212–20
Rennick A, Atkinson T, Cimino NM et al (2016) Variability in opioid equivalence calculations. Pain Med 17:892–898
McPherson ML, Walker K, Davis M et al (2019) Safe and appropriate use of methadone in hospice and palliative care: expert consensus white paper. J Pain Symptom Manage 57:635–645
Quigley C (2004) Opioid switching to improve pain relief and drug tolerability. Cochrane Database Syst Rev (3): CD004847
Mercadante S, Casuccio A, Calderone L (1999) Rapid switching from morphine to methadone in cancer patients with poor response to morphine. J Clin Oncol 17:3307–3312
Mercadante S (2012) Switching methadone: a 10-year experience of 345 patients in an acute palliative care unit. Pain Med 13:399–404
Mercadante S, Ferrera P, Villari P, Casuccio A (2005) Rapid switching between transdermal fentanyl and methadone in cancer patients. J Clin Oncol 23:5229–5234
Watanabe S, Tarumi Y, Oneschuk D, Lawlor P (2002) Opioid rotation to methadone: proceed with caution. J Clin Oncol 20:2409–2410
Mancini I, Lossignol DA, Body JJ (2000) Opioid switch to oral methadone in cancer pain. Curr Opin Oncol 12:308–313
Hagen NA, Wasylenko E (1999) Methadone: outpatient titration and monitoring strategies in cancer patients. J Pain Symptom Manage 18:369–375
Parsons HA, de la Cruz M, El Osta B et al (2010) Methadone initiation and rotation in the outpatient setting for patients with cancer pain. Cancer 116:520–528
Porta-Sales J, Garzón-Rodríguez C, Villavicencio-Chávez C, Llorens-Torromé S, González-Barboteo J (2016) Efficacy and safety of methadone as a second-line opioid for cancer pain in an outpatient clinic: a prospective open-label study. Oncologist 21:981–7
Walker PW, Palla S, Pei BL et al (2008) Switching from methadone to a different opioid: what is the equianalgesic dose ratio? J Palliat Med 11:1103–1108
Reddy A, Yennurajalingam S, Pulivarthi K et al (2013) Frequency, outcome, and predictors of success within 6 weeks of an opioid rotation among outpatients with cancer receiving strong opioids. Oncologist 18:212–220
Mercadante S, Bruera E (2012) The effect of age on opioid switching to methadone: a systematic review. J Palliat Med 15:347–351
Gagnon B, Bruera E (1999) Differences in the ratios of morphine to methadone in patients with neuropathic pain versus non-neuropathic pain. J Pain Symptom Manage 18:120–125
Oian Y, Haider A, Lu Z et al (2020) Factors associated with improvement in uncontrolled cancer pain without increasing the opioid daily dose among patients seen by an inpatient palliative care team. J Palliat Med 23:483–488
Mercadante S (2012) Switching methadone: a 10-year experience of 345 patients in an acute palliative care unit. Pain Med 13:399–404
Author information
Authors and Affiliations
Contributions
SM: protocol, writing.
PF, YG, CA: recruiting patients.
AL: database.
AC: statistics.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mercadante, S., Adile, C., Ferrera, P. et al. Conversion ratios for opioid switching: a pragmatic study. Support Care Cancer 31, 91 (2023). https://doi.org/10.1007/s00520-022-07514-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07514-4