Abstract
Purpose
The latest systematic review on the prevalence of pain in cancer survivors was published 5 years ago. The current review aims to provide an extended overview on the prevalence of pain, pain mechanisms, pain characteristics, and assessment methods in cancer survivors.
Methods
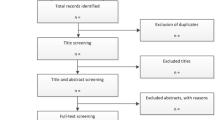
A systematic research was conducted on 17th of April 2020 using MEDLINE, Embase, Scopus, Web of Science, and Cochrane looking at studies from 2014 to 2020. Studies had to report pain prevalence rates in cancer survivors with a solid tumor who finished curative treatment at least 3 months ago. Methodological quality was assessed by two independent reviewers using the Joanna Briggs Institute quality appraisal tool. Characteristics of the included studies, participants and reported pain prevalence rates were extracted. The reported prevalence rates of the individual studies were pooled within a meta-analysis. Meta-regressions were performed to identify possible determinants of the pooled pain prevalence.
Results
After deduplication, 7300 articles were screened, after which 38 were included in the meta-analysis. Risk of bias was rated low in 26 articles and moderate in 12 articles. The pooled pain prevalence was 47% (95%CI 39–55), with a heterogeneity of 98.99%.
Conclusion
This meta-analysis suggests that nearly half of cancer survivors report pain after completing curative treatment at least 3 months ago. However, substantial unexplained heterogeneity warrants cautious interpretation of these results. Meta-regression using cancer type, treatment location, pain measurement, and follow-up time as a covariate could not explain influencing factors explaining the high heterogeneity.



Similar content being viewed by others
Abbreviations
- EORTC:
-
European Organization of Research and Treatment of Cancer
- QoL:
-
Quality of life
- NRS:
-
Numeric rating scale
- IASP:
-
International Association for the Study of Pain
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT:
-
Randomized controlled trial
- CIPN:
-
Chemotherapy-Induced Peripheral Neuropathy
- VH:
-
Vincent Haenen
- TdB:
-
Tom De Baerdemaecker
- ME:
-
Margaux Evenepoel
- ADG:
-
An De Groef
- JBI:
-
Joanna Briggs Institute
- VAS:
-
Visual analogue scale
- BPI:
-
Brief Pain Inventory
- NPSI:
-
Neuropathic Pain Symptom Inventory
- EORTC-QLQ-C30:
-
European Organization for Research and Treatment for Cancer Quality of Life Questionnaire
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Marzorati C, Riva S, Pravettoni G (2017) Who is a cancer survivor? A systematic review of published definitions. J Cancer Educ Off J Am Assoc Cancer Educ 32:228–237. https://doi.org/10.1007/s13187-016-0997-2
Richards M, Corner J, Maher J (2011) The National Cancer Survivorship Initiative: new and emerging evidence on the ongoing needs of cancer survivors. Br J Cancer 105:S1–S4. https://doi.org/10.1038/bjc.2011.416
Moser EC, Meunier F (2014) Cancer survivorship: a positive side-effect of more successful cancer treatment. EJC Suppl 12(1):1–4. https://doi.org/10.1016/j.ejcsup.2014.03.001
Gegechkori N, Haines L, Lin JJ (2017) Long-term and latent side effects of specific cancer types. Med Clin North Am 101:1053–1073. https://doi.org/10.1016/j.mcna.2017.06.003
Jacobs LA, Shulman LN (2017) Follow-up care of cancer survivors: challenges and solutions. Lancet Oncol 18(1):e19–e29. https://doi.org/10.1016/S1470-2045(16)30386-2
van den Beuken-van Everdingen MHJ, Hochstenbach LMJ, Joosten EAJ et al (2016) Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manag 51:1070-1090.e9. https://doi.org/10.1016/j.jpainsymman.2015.12.340
Serlin RC, Mendoza TR, Nakamura Y et al (1995) When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 61:277–284. https://doi.org/10.1016/0304-3959(94)00178-H
Chimenti RL, Frey-Law LA, Sluka KA (2018) A mechanism-based approach to physical therapist management of pain. Phys Ther 98:302–314. https://doi.org/10.1093/ptj/pzy030
Nijs J, Apeldoorn A, Hallegraeff H et al (2015) Low back pain: guidelines for the clinical classification of predominant neuropathic, nociceptive, or central sensitization pain. Pain Physician 18:E333-346
Malfait A-M, Schnitzer TJ (2013) Towards a mechanism-based approach to pain management in osteoarthritis. Nat Rev Rheumatol 9:654–664. https://doi.org/10.1038/nrrheum.2013.138
Merskey H, Bogduk N (1994) Classification of Chronic Pain, 2nd edn. IASP Press, Seattle, IASP Task Force on Taxonomy
Baron R (2006) Mechanisms of disease: neuropathic pain–a clinical perspective. Nat Clin Pract Neurol 2:95–106. https://doi.org/10.1038/ncpneuro0113
Backonja M-M (2003) Defining neuropathic pain. Anesth Analg 97(3):785–790. https://doi.org/10.1213/01.ANE.0000062826.70846.8D
Kosek E, Cohen M, Baron R et al (2016) Do we need a third mechanistic descriptor for chronic pain states? Pain 157:1382–1386. https://doi.org/10.1097/j.pain.0000000000000507
Nijs J, Leysen L, Adriaenssens N et al (2016) Pain following cancer treatment: guidelines for the clinical classification of predominant neuropathic, nociceptive and central sensitization pain. Acta Oncol Stockh Swed 55:659–663. https://doi.org/10.3109/0284186X.2016.1167958
Leysen L, Adriaenssens N, Nijs J et al (2019) Chronic pain in breast cancer survivors: nociceptive, neuropathic, or central sensitization pain? Pain Pract Off J World Inst Pain 19:183–195. https://doi.org/10.1111/papr.12732
Mustonen L, Aho T, Harno H, Kalso E (2020) Static mechanical allodynia in post-surgical neuropathic pain after breast cancer treatments. Scand J Pain 20:683–691. https://doi.org/10.1515/sjpain-2020-0013
Page MJ, McKenzie JE, Bossuyt PM, et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ n71. https://doi.org/10.1136/bmj.n71
Grisold W, Cavaletti G, Windebank AJ (2012) Peripheral neuropathies from chemotherapeutics and targeted agents: diagnosis, treatment, and prevention. Neuro-Oncol 14:iv45–iv54. https://doi.org/10.1093/neuonc/nos203
Munn Z, Moola S, Lisy K et al (2015) Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc 13:147–153. https://doi.org/10.1097/XEB.0000000000000054
Hoy D, Brooks P, Woolf A et al (2012) Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 65:934–939. https://doi.org/10.1016/j.jclinepi.2011.11.014
Higgins JPT, Thomas J, Chandler J et al (2022) Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). Cochrane. Available from www.training.cochrane.org/handbook
Lin L, Xu C (2020) Arcsine‐based transformations for meta‐analysis of proportions: Pros, cons, and alternatives. Health Sci Rep 3:. https://doi.org/10.1002/hsr2.178
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Wang L, Cohen JC, Devasenapathy N et al (2020) Prevalence and intensity of persistent post-surgical pain following breast cancer surgery: a systematic review and meta-analysis of observational studies. Br J Anaesth 125:346–357. https://doi.org/10.1016/j.bja.2020.04.088
Viechtbauer W (2010) Conducting Meta-Analyses in R with the metafor Package. J Stat Softw 36:. https://doi.org/10.18637/jss.v036.i03
R Core Team (2020) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.r-project.org/
Alkan A, Guc ZG, Senler FC et al (2016) Breast cancer survivors suffer from persistent postmastectomy pain syndrome and posttraumatic stress disorder (ORTHUS study): a study of the palliative care working committee of the Turkish Oncology Group (TOG). Support Care Cancer 24:3747–3755. https://doi.org/10.1007/s00520-016-3202-6
Bovbjerg DH, Keefe FJ, Soo MS et al (2019) Persistent breast pain in post-surgery breast cancer survivors and women with no history of breast surgery or cancer: associations with pain catastrophizing, perceived breast cancer risk, breast cancer worry, and emotional distress. Acta Oncol 58:763–768. https://doi.org/10.1080/0284186X.2019.1574023
Cobo-Cuenca AI, Martín-Espinosa NM, Sampietro-Crespo A et al (2018) Sexual dysfunction in Spanish women with breast cancer. PLoS One 13:e0203151. https://doi.org/10.1371/journal.pone.0203151
Edmond SN, Shelby RA, Keefe FJ et al (2017) Persistent breast pain among women with histories of breast-conserving surgery for breast cancer compared with women without histories of breast surgery or cancer. Clin J Pain 33:51–56. https://doi.org/10.1097/AJP.0000000000000377
Feiten S, Dünnebacke J, Heymanns J et al (2014) Breast cancer morbidity. Dtsch Aerzteblatt Online. https://doi.org/10.3238/arztebl.2014.0537
Frey A, Pedersen C, Lindberg H et al (2017) Prevalence and predicting factors for commonly neglected sexual side effects to external-beam radiation therapy for prostate cancer. J Sex Med 14:558–565. https://doi.org/10.1016/j.jsxm.2017.01.015
Hamood R, Hamood H, Merhasin I, Keinan-Boker L (2018) Chronic pain and other symptoms among breast cancer survivors: prevalence, predictors, and effects on quality of life. Breast Cancer Res Treat 167:157–169. https://doi.org/10.1007/s10549-017-4485-0
Kibar S, Dalyan Aras M, Ünsal Delialioğlu S (2017) The risk factors and prevalence of upper extremity impairments and an analysis of effects of lymphoedema and other impairments on the quality of life of breast cancer patients. Eur J Cancer Care (Engl) 26:e12433. https://doi.org/10.1111/ecc.12433
Stinesen Kollberg K, Waldenström A-C, Bergmark K et al (2015) Reduced vaginal elasticity, reduced lubrication, and deep and superficial dyspareunia in irradiated gynecological cancer survivors. Acta Oncol 54:772–779. https://doi.org/10.3109/0284186X.2014.1001036
Kramer N, Ramjith J, Shamley D (2019) Prevalence of shoulder morbidity after treatment for breast Cancer in South Africa. Support Care Cancer 27:2591–2598. https://doi.org/10.1007/s00520-018-4540-3
Lopez C, Charles C, Rouby P et al (2015) Relations between arthralgia and fear of recurrence: results of a cross-sectional study of breast cancer patients treated with adjuvant aromatase inhibitors therapy. Support Care Cancer 23:3581–3588. https://doi.org/10.1007/s00520-015-2722-9
Lowery AE, Krebs P, Coups EJ et al (2014) Impact of symptom burden in post-surgical non-small cell lung cancer survivors. Support Care Cancer 22:173–180. https://doi.org/10.1007/s00520-013-1968-3
Manfuku M, Nishigami T, Mibu A et al (2019) Comparison of central sensitization-related symptoms and health-related quality of life between breast cancer survivors with and without chronic pain and healthy controls. Breast Cancer 26:758–765. https://doi.org/10.1007/s12282-019-00979-y
Mertz BG, Duriaud HM, Kroman N, Andersen KG (2017) Pain, sensory disturbances and psychological distress are common sequelae after treatment of ductal carcinoma in situ : a cross-sectional study. Acta Oncol 56:724–729. https://doi.org/10.1080/0284186X.2017.1295167
Santos LJF, dos Garcia JBS, Pacheco JS et al (2014) Quality of life, pain, anxiety and depression in patients surgically treated with cancer of rectum. ABCD Arq Bras Cir Dig São Paulo 27:96–100. https://doi.org/10.1590/S0102-67202014000200003
Smoot B, Boyd BS, Byl N, Dodd M (2014) Mechanosensitivity in the upper extremity following breast cancer treatment. J Hand Ther 27:4–11. https://doi.org/10.1016/j.jht.2013.08.021
Steyaert A, Forget P, Dubois V et al (2016) Does the perioperative analgesic/anesthetic regimen influence the prevalence of long-term chronic pain after mastectomy? J Clin Anesth 33:20–25. https://doi.org/10.1016/j.jclinane.2015.07.010
Yi M, Hwang E (2018) Pain and menopause symptoms of breast cancer patients with adjuvant hormonal therapy in Korea: secondary analysis. Asia-Pac J Oncol Nurs 5:262. https://doi.org/10.4103/apjon.apjon_45_17
Aerts L, Enzlin P, Verhaeghe J et al (2014) Long-term sexual functioning in women after surgical treatment of cervical cancer stages IA to IB: a prospective controlled study. Int J Gynecol Cancer 24:1527–1534. https://doi.org/10.1097/IGC.0000000000000236
Andersen KG, Duriaud HM, Kehlet H, Aasvang EK (2017) The relationship between sensory loss and persistent pain 1 year after breast cancer surgery. J Pain 18:1129–1138. https://doi.org/10.1016/j.jpain.2017.05.002
De Groef A, Van Kampen M, Tieto E et al (2016) Arm lymphoedema and upper limb impairments in sentinel node-negative breast cancer patients: a one year follow-up study. Breast 29:102–108. https://doi.org/10.1016/j.breast.2016.07.021
Farrell R, Gebski V, Hacker NF (2014) Quality of life after complete lymphadenectomy for vulvar cancer: do women prefer sentinel lymph node biopsy? Int J Gynecol Cancer 24:813–819. https://doi.org/10.1097/IGC.0000000000000101
Gjeilo KH, Oksholm T, Follestad T et al (2020) Trajectories of pain in patients undergoing lung cancer surgery: a longitudinal prospective study. J Pain Symptom Manag 59:818-828.e1. https://doi.org/10.1016/j.jpainsymman.2019.11.004
Hadji P, Jackisch C, Bolten W et al (2014) COMPliance and Arthralgia in Clinical Therapy: the COMPACT trial, assessing the incidence of arthralgia, and compliance within the first year of adjuvant anastrozole therapy. Ann Oncol 25:372–377. https://doi.org/10.1093/annonc/mdt513
Hurtz H-J, Tesch H, Göhler T et al (2017) Persistent impairments 3 years after (neo)adjuvant chemotherapy for breast cancer: results from the MaTox project. Breast Cancer Res Treat 165:721–731. https://doi.org/10.1007/s10549-017-4365-7
Janssen S, Glanzmann C, Lang S et al (2014) Hypofractionated radiotherapy for breast cancer acceleration of the START A treatment regime: intermediate tolerance and efficacy. Radiat Oncol 9:165. https://doi.org/10.1186/1748-717X-9-165
Johansen S, Fosså K, Nesvold IL et al (2014) Arm and shoulder morbidity following surgery and radiotherapy for breast cancer. Acta Oncol 53:521–529. https://doi.org/10.3109/0284186X.2014.880512
Johannsen M, Christensen S, Zachariae R, Jensen A (2015) Socio-demographic, treatment-related, and health behavioral predictors of persistent pain 15 months and 7–9 years after surgery: a nationwide prospective study of women treated for primary breast cancer. Breast Cancer Res Treat 152:645–658. https://doi.org/10.1007/s10549-015-3497-x
Kidwell KM, Harte SE, Hayes DF et al (2014) Patient-reported symptoms and discontinuation of adjuvant aromatase inhibitor therapy: baseline symptoms & AI discontinuation. Cancer 120:2403–2411. https://doi.org/10.1002/cncr.28756
Koehler LA, Hunter DW, Blaes AH, Haddad TC (2018) Function, shoulder motion, pain, and lymphedema in breast cancer with and without axillary web syndrome: an 18-month follow-up. Phys Ther 98:518–527. https://doi.org/10.1093/ptj/pzy010
Laroche F, Perrot S, Medkour T et al (2017) Quality of life and impact of pain in women treated with aromatase inhibitors for breast cancer A multicenter cohort study. PLoS One 12:e0187165. https://doi.org/10.1371/journal.pone.0187165
Lee M-J, Beith J, Ward L, Kilbreath S (2014) Lymphedema following taxane-based chemotherapy in women with early breast cancer. Lymphat Res Biol 12:282–288. https://doi.org/10.1089/lrb.2014.0030
Mandelblatt JS, Zhai W, Ahn J et al (2020) Symptom burden among older breast cancer survivors: The Thinking and Living With Cancer (TLC) study. Cancer 126:1183–1192. https://doi.org/10.1002/cncr.32663
Mózsa E, Mészáros N, Major T et al (2014) Accelerated partial breast irradiation with external beam three-dimensional conformal radiotherapy: five-year results of a prospective phase II clinical study. Strahlenther Onkol 190:444–450. https://doi.org/10.1007/s00066-014-0633-1
Mustonen L, Aho T, Harno H et al (2019) What makes surgical nerve injury painful? A 4-year to 9-year follow-up of patients with intercostobrachial nerve resection in women treated for breast cancer. Pain 160:246–256. https://doi.org/10.1097/j.pain.0000000000001398
Rizk NP, Ghanie A, Hsu M et al (2014) A prospective trial comparing pain and quality of life measures after anatomic lung resection using thoracoscopy or thoracotomy. Ann Thorac Surg 98:1160–1166. https://doi.org/10.1016/j.athoracsur.2014.05.028
Schmidt ME, Wiskemann J, Steindorf K (2018) Quality of life, problems, and needs of disease-free breast cancer survivors 5 years after diagnosis. Qual Life Res 27:2077–2086. https://doi.org/10.1007/s11136-018-1866-8
United Nations (2021) World economic situation and prospects. UN, New York. https://digitallibrary.un.org/record/3898345/files/WESP2021_FullReport.pdf. Accessed 16 Aug 2021
Kaur N, Kumar A, Saxena AK et al (2018) Postmastectomy chronic pain in breast cancer survivors: an exploratory study on prevalence, characteristics, risk factors, and impact on quality of life. Indian J Surg 80:592–598. https://doi.org/10.1007/s12262-017-1663-6
Finnerup NB, Haroutounian S, Kamerman P et al (2016) Neuropathic pain: an updated grading system for research and clinical practice. Pain 157:1599–1606. https://doi.org/10.1097/j.pain.0000000000000492
Minello C, George B, Allano G et al (2019) Assessing cancer pain—the first step toward improving patients’ quality of life. Support Care Cancer 27:3095–3104. https://doi.org/10.1007/s00520-019-04825-x
Munn Z, Moola S, Lisy K et al (2020) Chapter 5: systematic reviews of prevalence and incidence. In: Aromataris E, Munn Z(Editors). JBI Manual for Evidence Synthesis. JBI, 2020. Available from https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-06
Borges Migliavaca C, Stein C, Colpani V et al (2020) How are systematic reviews of prevalence conducted? A methodological study. BMC Med Res Methodol 20:96. https://doi.org/10.1186/s12874-020-00975-3
Mills SEE, Nicolson KP, Smith BH (2019) Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth 123:e273–e283. https://doi.org/10.1016/j.bja.2019.03.023
Breivik H, Collett B, Ventafridda V et al (2006) Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur J Pain 10:287–287. https://doi.org/10.1016/j.ejpain.2005.06.009
Belfer I, Schreiber KL, Shaffer JR et al (2013) Persistent postmastectomy pain in breast cancer survivors: analysis of clinical, demographic, and psychosocial factors. J Pain 14:1185–1195. https://doi.org/10.1016/j.jpain.2013.05.002
Funding
This research was supported by the Flanders Research Foundation [grant number 12R1719N].
Author information
Authors and Affiliations
Contributions
Vincent Haenen and Margaux Evenepoel were responsible for the study conception and design. Study preparation, data collection and analysis were performed by Vincent Haenen and Margaux Evenepoel. The first version of the manuscript was written by Vincent Haenen and all authors reviewed previous versions. The final manuscript was read and approved by all authors.
Corresponding author
Ethics declarations
Ethics approval
N/A.
Consent to participate
N/A.
Consent for publication
N/A.
Competing interests
All authors have completed the ICMJE uniform disclosure form (available on request from the corresponding author) and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work. B. Morlion has served as a consultant for Reckitt-Benekiser, Grunenthal, Pfizer, GSK, and as a speaker for Grunenthal, Krka, GSK Belgium.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haenen, V., Evenepoel, M., De Baerdemaecker, T. et al. Pain prevalence and characteristics in survivors of solid cancers: a systematic review and meta-analysis. Support Care Cancer 31, 85 (2023). https://doi.org/10.1007/s00520-022-07491-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07491-8