Abstract
Purpose
The “Ballet after breast cancer” study sought to investigate the feasibility and acceptability of a 16-week classical ballet intervention for breast cancer survivors, delivered face-to-face and/or online.
Methods
Breast cancer survivors were recruited to take part in 2 × 1-h ballet classes per week for 16 weeks. Primary outcomes of feasibility and acceptability were assessed according to rates of enrolment and attendance and participant feedback via questionnaire. Secondary outcomes included quality of life (QOL), upper-body disability, shoulder range of motion (ROM), muscular strength, aerobic capacity, and physical activity levels. Associations between rate of attendance and changes in secondary measures were explored.
Results
Thirty-one participants (62% of eligible individuals) enrolled in the program. Twenty-nine women commenced the intervention [53.3 ± 10.8 years (Mean ± SD)], attending 77.6% [67.6, 87.5] (Mean [95% CI]) of sessions. Based on these rates of enrolment and attendance, and participant feedback, the program was deemed feasible and acceptable to participants. Significant improvements in shoulder ROM and reductions in sedentary behaviour were achieved. Participants also reported improvements in physical capacity and psychological, social, and cognitive wellbeing.
Conclusions
The “Ballet after breast cancer” program, delivered face-to-face and/or online, was feasible and acceptable to breast cancer survivors. Improvements in shoulder ROM achieved doing ballet were pertinent given the adverse effects of upper-body morbidity on breast cancer survivor QOL. Improvements in physical activity behaviour and perceived benefits to wellbeing also support the use of ballet to mitigate QOL impairment after treatment.
Implications for cancer survivors
The physical demands and the fun, creative, and social characteristics of ballet promote improvement across multiple domains of health and wellbeing. Ballet shows promise as an activity to improve QOL and increase long-term engagement in health-promoting physical activity after breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most diagnosed malignancy worldwide. In 2020, female breast cancers represented 11.7% of global cancer diagnoses and accounted for 29% of cancer diagnoses in Australian women [1]. Whilst the likelihood of survival from early breast cancer now exceeds 90% [2], quality of life (QOL) for breast cancer survivors may be undermined by persisting treatment effects, impaired psychosocial wellbeing, and elevated risk of comorbid health conditions and cancer recurrences. It is well established that physical activity can impart numerous benefits to individuals on the cancer continuum, improving physical function, body composition, cardiorespiratory function, metabolic health, and psychosocial wellbeing [3,4,5]. With side effects including upper-body morbidity (UBM)—such as upper-limb lymphoedema, reduced shoulder range of motion (ROM), and upper-body pain—impaired cardiac function, poor metabolic health, and reduced bone mineral density known to effect breast cancer survivors, the physiological benefits exercise confers are pertinent to this population. Despite the known benefits, reports indicate that 20 to 54% of breast cancer survivors meet current physical activity guidelines [6], with motivation, persisting treatment-related side effects, self-confidence, and access to suitable exercise resources cited as barriers to engagement [7]. Further barriers to exercise faced during the COVID-19 pandemic, such as restricted access to exercise facilities, exercise professionals, and peers to exercise with, may have contributed to the reduction in physical activity and increase in sedentary behaviour observed in general and breast cancer survivor populations at this time [8,9,10]. Strategies to promote exercise uptake and adherence to help survivors reap the benefits of physical activity during and beyond the COVID-19 era are warranted.
One such strategy is the promotion of dance for health. Dance is a fun, creative, and social activity, which demonstrates potential to improve multiple aspects of health and wellbeing. The positive effects of dance have been observed across healthy and clinical population groups, including cancer patients and survivors [11,12,13,14,15,16,17,18]. Dance has been shown to elicit improvements in cardiometabolic health, cardiorespiratory fitness, muscle strength and power, flexibility, balance, and proprioception [16, 19, 20] as well as mental health and QOL [16], all of which are particularly pertinent after breast cancer treatment.
Classical ballet, like other styles of dance, is an attractive and enjoyable form of physical activity. Ballet has additional characteristics, such as a unique use of the upper-body, which sets it apart as an ideal style of dance for breast cancer survivors. Individuals with treatment-related UBM such as lymphedema, pain, or restricted shoulder ROM are poised to benefit from exercises promoting positive strength/endurance, proprioception, and mobility adaptations to the upper body. The characteristic ballet “port de bras” or “carriage of the arms” (Online Resource 1) through five main upper-body positions calls for postural control, coordination, musculoskeletal endurance, and a large shoulder range of motion (ROM) [21]. Given the potential reductions in QOL associated with UBM, ballet may also contribute to improved QOL by addressing upper-body impairments [22]. Furthermore, ballet is based on a codified movement vocabulary, the basics of which are learned before complex choreographed series are performed [21]. The progressive and repetitive way in which ballet is taught makes it ideal for individuals seeking a graded return to physical activity after breast cancer. Finally, recognising French ballet terminology and being able to recall, anticipate, and execute technical ballet choreography in time with music rely on complex cognitive processing and concentration [23, 24]. This may be of benefit to individuals experiencing cognitive impairment following cancer treatment [25].
Based on findings from other dance genres [12, 14, 15, 18, 26,27,28,29] and online exercise interventions delivered to breast cancer survivors [30], ballet shows promise in promoting physical activity adherence and improvements in health and wellbeing in this population. However, no studies have investigated the use of traditional classical ballet, delivered face-to-face or remotely to individuals following completion of primary breast cancer treatment. Therefore, the objective of this study was to investigate the feasibility and acceptability of a novel 16-week classical ballet intervention for breast cancer survivors, delivered face-to-face and/or remotely online. Additionally, the study aimed to identify changes in QOL, physical activity levels, upper-body function, muscular strength, and aerobic capacity of participants after the intervention and identify associations between ballet class attendance and such changes.
Methods
Ethics approval
Ethical approval for this study was granted by the UNSW Human Research Ethics Committee (HC200758).
Study registration
The study was prospectively registered on the Open Science Framework (osf.io/j87vf).
Sample size and recruitment
As the primary study outcomes were feasibility and acceptability, a priori power calculations based on the secondary outcome QOL were used as a guide for recruitment targets. To detect a moderate effect (d = 0.5) of physical activity on QOL, with 85% confidence, a total sample of 31 participants would be necessary. Accounting for 15–20% attrition, a target sample of 40 participants was deemed suitable for the study [12, 18, 28].
Recruitment
Participants were recruited from the community, via material distributed to breast cancer support groups, organisations, and university social media platforms. Individuals eligible to take part were > 18 years of age, previously diagnosed with stage 0–III breast cancer, and completed primary treatment (surgery, chemotherapy, and/or radiotherapy) > 3 months prior to the intervention. Exclusion criteria were < 18 years of age, currently undergoing active breast cancer treatment (excluding ongoing hormonotherapy or targeted therapy), or had medical conditions and/or physical limitations contraindicating safe participation in dance. Written informed consent was provided by all participants upon enrolment.
Intervention
The intervention consisted of 1-h classical ballet classes twice per week for 16 weeks and was intended for face-to-face delivery to two intervention groups, successively. Baseline assessments and ballet classes commenced face-to-face for intervention group one (G1) and were converted to online delivery via “Zoom” (Zoom Video Communications, Inc.), from week 6 due to COVID-19 restrictions. Intervention group two (G2) completed all study components online. Secondary outcome assessment methods were modified or substituted for remote delivery, based on evidence demonstrating validity and reliability of online assessments delivered by one assessor [31].
Ballet classes were delivered by an experienced instructor qualified by the Royal Academy of Dance. Each class followed a traditional ballet format, including a general 5-min warm up, 50-min of ballet-based exercise, and 5-min cool down. Classes consisted of stationary exercises at the barre (approx. 30 min) involving progressively increasing joint range of motion as in Online Resource 1, followed by a series of dance combinations in the centre of the room (approx. 20 min) usually involving balance training (adage), progressing to a series of travelling and turning combinations, and ending with a set of jump exercises (allegro). The exercises increased in complexity, intensity, and volume, proportionate to the group’s improvement in physical endurance, skill, coordination, and balance. The program was adjusted for online delivery, accounting for space limitations, by designing exercises that could be performed in smaller spaces, e.g. reduced repetition of travelling steps and vertical rather than horizontal jumping movements. Where necessary, the ballet teacher offered exercise modifications or progressions so all participants could complete a variation of each exercise within the limits of their capability.
Primary outcome measures
Feasibility was assessed based on rates of enrolment and ballet class attendance. The intervention was deemed feasible if more than 50% of eligible individuals enrolled in the ballet program and if mean rate of class attendance exceeded 75%. Acceptability was assessed using participant responses to a purpose-designed intervention evaluation questionnaire (Online Resource 2). Items referred to the suitability of class frequency and challenge, perceptions of ballet program benefit, ratings of enjoyment, and likelihood of ballet continuation and recommendation to others.
Secondary outcome measures
Quality of life
QOL was assessed using the Functional Assessment of Cancer Therapy, Breast (Lymphedema) (FACT-B + 4) questionnaire (v4) [32]. The questionnaire is validated for use in breast cancer patients/survivors [32] and assesses wellbeing using seven subscales: physical (PWB), social/family (SWB), emotional (EWB), functional (FWB) wellbeing, breast cancer subscale (BCS), and arm symptoms subscale (ARM). Higher scores indicate superior QOL. Permission to use this tool was granted by the Functional Assessment of Chronic Illness Therapy (FACIT) system.
Upper-body disability
Self-reported upper-body disability was assessed using the Disability of the Arm Shoulder and Hand (DASH) questionnaire [33]. Questionnaire items relate to limitations in daily activities due to arm, shoulder, and hand morbidity. Low scores (< 15) indicate clinically significant upper-body disability [34].
Physical activity levels
Physical activity levels were assessed using the Long International Physical Activity Questionnaire (IPAQ) [35]. Questions relate to the frequency, duration, and intensity of leisure, occupational, transportation, household, and sedentary activities. Questionnaire output included weekly minutes of moderate to vigorous physical activity (MVPA) and average daily sitting time (min/day).
Shoulder range of motion
Shoulder ROM data were collected using goniometry during face-to-face assessments (G1 baseline only) or video recordings during online assessments (G1 post-intervention; G2 baseline and post-intervention). ROM data were extracted from videos using “Tracker” software (v5.1.5, Open Source Physics). Participants performed shoulder flexion/extension, abduction, and internal/external rotation in standing. Digital markers were placed on anatomical landmarks, and the protractor function was used to track movement of upper limb markers (humerus, ulnar) relative to the glenohumeral joint centre. For each movement, the average range achieved across three attempts was calculated. To ensure the same fidelity for online as in-person measures, camera placement was replicated at each time point, instructions were provided by the same researcher, and measures were completed in triplicate.
Upper-body strength
The maximal push up test using the American College of Sports Medicine (ACSM) protocol was used to assess upper-body strength (G2 only, online) with higher scores indicating superior upper-body strength [5]. Tests were terminated when participants were unable to perform the exercise with correct technique.
Lower-body strength
Lower-body strength was assessed using the 30-s chair stand (G2 only, online) [3, 6]. The number of repetitions performed in 30 s was recorded, with higher scores indicating superior lower-body strength.
Aerobic capacity
Aerobic capacity was assessed using the 6-min walk test (6MWT) according to the American Thoracic Society (ATS) protocol [36]. G1 completed the 6MWT face-to-face at baseline. Thereafter, (G1 post-intervention; G2 baseline and post-intervention), participants were equipped to conduct the 6MWT from home independently, with the assistance of a friend/family member. Packs containing two field markers, a 20-m rope, and data collection instructions were mailed to each participant prior to their online assessment. Detailed instructions for the conduct of the test were provided by the study coordinator. Greater total walking distance (metres) indicated superior aerobic capacity.
Statistical analysis
Analysis of the primary outcomes of feasibility and acceptability consisted of mean proportions with a 95% confidence interval using a binomial assumption. Changes in secondary outcome measures including FACT-B + 4, DASH subscale scores, IPAQ questionnaire scores, 6MWT distance, maximal push up score, and 30-s chair stand score were evaluated using paired t-tests. Results are reported as mean change with 95% confidence interval. Linear mixed models were used to evaluate overall changes in shoulder ROM and to determine whether ROM on the affected and unaffected sides changed differentially. ROM change data contained two measures per participant (affected side, unaffected side). “Participant” was included as a random effect to account for dependence. For all secondary analyses, the significance level was set to α = 0.05, with p-values adjusted for multiple testing. Exploratory regression analyses were performed to evaluate the effect of attendance rate on changes in selected secondary outcome measures. Significance levels were also set to α = 0.05, p-values unadjusted.
Results
Participant characteristics
Thirty-one participants enrolled in the study, of which 29 commenced the ballet program and 24 saw it through to completion (Fig. 1). Participants (n = 29) were female, aged 53.3 ± 10.8 years (Mean ± SD). Demographic and treatment-related information are provided in Table 1.
Feasibility and acceptability
Sixty-two percent of eligible individuals enrolled in the study, exceeding the 50% feasibility threshold. The study cohort attended an average of 77.6% [67.6, 87.5] (Mean [95% CI]) of scheduled ballet classes, thus exceeding the feasibility threshold of 75% attendance. G1 and G2 attended 88.3% [78.0, 98.5] and 73.0% [59.5, 86.6] of sessions, respectively.
According to evaluation responses (Participant quotations italicised), 80.9% of participants reported the class frequency as “the right amount” and necessary to “maintain momentum” and achieve meaningful improvements in skill and physical fitness (Online Resource 2). Some considered one class per week a more realistic commitment long term, due to family and work demands. The level of challenge of the classes was rated “The right level of challenge” by 90.5% of participants. The exercises were “not so difficult that [they] didn’t want to go back for the next class” and progressive so that one could be challenged “a little bit more each time and gradually and logically build strength”. The classes met expectations for 87.5% of participants, and only somewhat met expectations for 12.5% participants, all of whom were in G2. These participants indicated that online classes did not facilitate expected levels of social engagement, and exercises were less free flowing and physically demanding than anticipated: “[I] have done many dance classes over the years (ballroom, salsa, swing and flamenco) and was expecting these ballet classes to be a similar level of challenge. However, the classes didn’t challenge me and I didn’t feel I was exercising”.
The majority (87.5%) of participants rated enjoyment and perceived benefit of ballet classes as ≥ 4/5. The classes were enjoyed as an opportunity to “learn a completely new skill and new movements” that were creative and expressive, “without any pressure to be perfect”. Dancing was a way of “exercising without realising it”, and participants valued “option[s] for variation in ability levels”. Participants described improvements in body awareness, fitness, strength, flexibility, balance, and posture. Positive changes in self-esteem, mood, stress levels, and mental focus were reported. In participants with existing musculoskeletal pain, ballet contributed positively to pain management and improved confidence in performing movements they “didn’t think currently possible”. Eighty percent of participants were extremely likely to recommend ballet as a “fun and challenging way to push your physical and mental limits” and the “best and most enjoyable method to rehabilitate after cancer”. Seventy-five percent of participants were “likely” or “extremely likely” to continue with ballet. However, some reported that future participation would be contingent upon the availability of similar ballet programs, targeted towards “being a late learner with physical challenges” after cancer. Accessibility, cost, and scheduling of classes were also cited as considerations for ballet continuation.
Adverse events
One participant experienced light headedness during a face-to-face class, whilst wearing a surgical mask as a COVID-19 precaution. No other adverse events were reported. Minor exercise modifications were provided for participants with joint discomfort or restricted shoulder ROM, where necessary. For example, holding arms in first (below shoulder height), instead of fifth (overhead) position, or replacing jumps with a Plié (Knee bend) and Relevé (Rise).
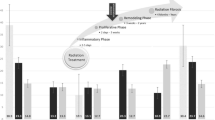
Secondary analyses
Changes in secondary outcome measures are presented in Table 2. QOL was maintained over the course of the intervention, indicated by the absence of significant changes in FACT-B + 4 questionnaire scores. Baseline DASH scores were not indicative of clinically significant upper-body disability. No significant changes were observed in self-reported upper-body disability, including for work and sports/performing arts tasks. Significant reductions in sedentary behaviour were observed with participants reporting a reduction in average daily sitting time of − 54.6 min [− 93.1, − 16.2] (p = 0.04). Participants increased their weekly duration of MVPA by 279.2 min [− 125.7, 683.9], but this change was not significant (p = 0.39). Unadjusted p-values indicated significant reductions in upper-body strength (p = 0.01) and borderline significant improvements in aerobic capacity (p = 0.05). However, following adjustment for multiple testing, no significant changes were observed in aerobic capacity, upper-body strength, or lower-body strength indicated by comparable pre- and post-intervention performance in the 6MWT (p = 0.18), maximal push-up test (p = 0.06), and 30 s chair stand (p = 0.22), respectively. Improvements in shoulder flexion, extension, and abduction were achieved for affected and unaffected sides combined. ROM improved by an average of 6.1° flexion [t = 3.74, df = 23, 95% CI = 2.86, 9.42, p = 0.001], 5.8° extension [t = 4.15, df = 23.06, 95% CI = 3.01, 8.58, p < 0.001], and 6.8° abduction [t = 2.96, df = 23, 95% CI = 2.19, 11.31, p = 0.007] (Table 3). The mean change in shoulder ROM did not differ significantly between affected and unaffected sides for flexion, extension, or abduction.
Exploratory analyses
Exploratory analyses using univariate linear regression provided no evidence to suggest that rate of attendance to the ballet intervention was associated with reductions in sitting time [t = 0.535, df = 22, 95% CI = − 1.79, 3.04, p = 0.598], improvements in upper-body strength [t = 0.96, df = 12, 95% CI = − 0.07, 0.20, p = 0.356], or shoulder flexion [t = − 0.12, df = 22, 95% CI = − 0.22, 0.19, p = 0.906], extension [t = 1.30, df = 21.62, 95% CI = − 0.06, 0.27, p = 0.209], or abduction [t = 0.33, df = 22, 95% CI = − 0.23, 0.33, p = 0.747].
Discussion
The “Ballet after breast cancer” study aimed to investigate the feasibility and acceptability of ballet for breast cancer survivors and identify changes in objective physical capacity and self-reported outcomes. Based on rates of enrolment and attendance, and participant evaluation, the program was deemed feasible and acceptable. Class attendance rates and participant feedback related to the benefits and suitability of dance were comparable to those reported in other studies of dance post-cancer [12, 14, 17, 37]. As in previous interventions assessing the feasibility of Hawaiian Hula dance [12] and Ballroom dance [17] after cancer treatment, participants of the present study were inclined to recommend ballet to others or express interest in ongoing participation.
Previously, dance interventions for individuals after cancer have produced positive changes in self-reported outcomes, such as QOL [12, 14, 15, 18, 37,38,39], fatigue [14, 15, 37], physical activity [12, 18], and psychological wellbeing [14, 15, 27, 37, 39], as well as objective outcomes including cardiorespiratory fitness [18, 28, 38], body composition/anthropometry [12, 28, 38], and muscular strength [28, 38]. The perceived improvements in physical capacity, mood, confidence, and cognition reported by participants in this study endorse ballet as another activity with benefits spanning multiple aspects of wellbeing for cancer survivors. Similar health benefits of participation in dance have also been reported for other clinical populations, including Parkinson’s disease, cerebral palsy, stroke, multiple sclerosis, and Alzheimer’s disease [16]. The health effects of classical ballet have been less frequently studied than other dance genres, but positive effects of ballet have been demonstrated in Parkinson’s disease, cerebral palsy, and multiple sclerosis [40]. The present study is the first to report significant, quantifiable improvements in shoulder ROM following a dance intervention (excluding dance movement therapy) for breast cancer survivors. Studies of other dance styles have reported insignificant changes in ROM [38, 41] or have not provided data to quantify described improvements in ROM [27]. Given the prevalence of treatment-related UBM—including impaired shoulder ROM—and the risk of impaired QOL associated with upper-body symptoms and activity limitations [22], this finding is highly pertinent, supporting ballet as an ideal dance style/ activity to minimise the burden of UBM after breast cancer.
The large, but statistically insignificant change in self-reported MVPA should be noted. Participants recorded an average of four additional hours of weekly MVPA, including walking and moderate to vigorous intensity household, transportation, occupational, and leisure activities post-intervention. This may be attributed to the atypically high volume of home maintenance activities (e.g. moving house) reported post-intervention and atypically low baseline MVPA levels due to COVID-19 restrictions.
One feature distinguishing the present study from previous dance interventions was the online delivery. Some aspects of the group class experience were lost by moving online, and this may account in part for the lack of substantial changes in outcome measures, for example, the opportunity to form relationships with other class participants. Previous literature has identified this as a key contributor to the psychosocial benefits of taking part in a group/partnered dance intervention, but this was diminished in the current study because of the online delivery [15, 17, 27]. In addition, due to the space limitations of attending classes from home and the reduced capacity for monitoring participants, the intended intensity and technical correctness of ballet exercises may not have been achieved, contributing to reduced physiological adaptation. The present study was not designed to determine the effectiveness of classical ballet and was thus unable to demonstrate that online delivery attenuated changes in secondary outcome measures. However, findings from another exercise intervention for breast cancer survivors conducted during the COVID-19 pandemic suggests that this might be a reasonable assumption [30]. According to Winters-Stone et al. (2021), a resistance training intervention delivered online demonstrated inferior effectiveness to the equivalent intervention delivered face-to-face, despite achieving higher rates of adherence and retention, and comparable safety [30].
In lieu of a sufficient sample size and control group, the extent to which changes could be attributed to the intervention was inferred. Exploratory analyses sought to elucidate the effect of rate of attendance on changes in secondary outcomes. This may have led to an over- or underestimation of intervention effectiveness as attendance only accounts for one aspect of program engagement. Other factors, such as exercise compliance and social interaction with classmates, may have contributed to program engagement and the magnitude of changes in secondary outcome measures.
Despite the limitations associated with study design, the “Ballet after breast cancer” program demonstrated many strengths. This was the first program to deliver classical ballet classes following a traditional format, to breast cancer survivors after primary treatment. In spite of the restrictions imposed on the study due to the COVID-19 pandemic, the program demonstrated unanticipated strengths. Online delivery was attractive to individuals unable/unwilling to attend in-person classes for reasons including safety, availability, time commitment, and travel. Furthermore, the sense of routine, social interaction, and regular physical activity the program provided may have curtailed an otherwise significant increase in stress, social isolation, sedentary behaviour, and impaired QOL, as has been observed globally during the pandemic [8, 42]. The potential acute effects of each ballet class should also be considered, in light of suggestions of improvements in positive affect, self-esteem, social/community connectedness, and depressive symptoms following a single session of ballet, jazz, or modern dance attended online during the pandemic [43].
Conclusions
Classical ballet is a feasible and acceptable mode of activity after breast cancer, leading to qualitative reports of improved physical and psychosocial wellbeing. The “Ballet after breast cancer” study provided preliminary evidence to suggest ballet can contribute to improving shoulder ROM and reducing sedentary activity. Delivering the program online helped to overcome several barriers which prevent engagement in physical and social activities after breast cancer, including barriers related to the COVID-19 pandemic. The findings of this study exposed avenues for investigating the comparative effectiveness of ballet and honing its implementation after breast cancer.
Data availability
The datasets generated in the present study are available from the corresponding author on reasonable request.
References
Australian Institute of Health and Welfare (2021) Cancer data in Australia. AIHW, Canberra
Australian Institute of Health and Welfare (2020) BreastScreen Australia monitoring report. AIHW: Canberra. p. 1-156
Ditsch N et al (2019) AGO recommendations for the diagnosis and treatment of patients with early breast cancer: update 2019. Breast Care 14(4):224–245. https://doi.org/10.1159/000501000
Blanchard CM, Courneya KS, Stein K (2008) Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. JCO 26(13):2198–2204. https://doi.org/10.1200/JCO.2007.14.6217
Hayes SC et al (2019) The exercise and sports science Australia position statement: exercise medicine in cancer management. J Sci Med Sport 22(11):1175–1199. https://doi.org/10.1016/j.jsams.2019.05.003
Krok-Schoen JL et al (2022) Correlates of physical activity among older breast cancer survivors: findings from the Women’s Health Initiative LILAC study. J Geriatric Oncol 13(2):143–151. https://doi.org/10.1016/j.jgo.2021.11.012
Clifford BK et al (2018) Barriers and facilitators of exercise experienced by cancer survivors: a mixed methods systematic review. Support Care Cancer 26(3):685–700. https://doi.org/10.1007/s00520-017-3964-5
Violant-Holz V et al (2020) Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health 17(24):9419. https://doi.org/10.3390/ijerph17249419
Brown M et al (2021) Impact of COVID-19 on an established physical activity and behaviour change support programme for cancer survivors: an exploratory survey of the Macmillan Move More service for Northern Ireland. Support Care Cancer: Off J Multi Assoc Support Care Cancer 29(10):6135–6143. https://doi.org/10.1007/s00520-021-06165-1
Natalucci V et al (2021) Special attention to physical activity in breast cancer patients during the first wave of COVID-19 pandemic in Italy: the DianaWeb cohort. J Pers Med 11(5):381. https://doi.org/10.3390/jpm11050381
Quiroga Murcia C et al (2010) Shall we dance? An exploration of the perceived benefits of dancing on well-being. Arts Health 2(2):149–163. https://doi.org/10.1080/17533010903488582
Loo L et al (2019) Using a cultural dance program to increase sustainable physical activity for breast cancer survivors—a pilot study. Complement Ther Med 47:102197. https://doi.org/10.1016/j.ctim.2019.102197
Kaltsatou A, Mameletzi D, Douka S (2011) Physical and psychological benefits of a 24-week traditional dance program in breast cancer survivors. J Bodyw Mov Ther 15(2):162–167
Sturm I et al (2014) Effect of dance on cancer-related fatigue and quality of life. Support Care Cancer 8:2241–2249. https://doi.org/10.1007/s00520-014-2181-8
Boing L et al (2018) Benefits of belly dance on quality of life, fatigue, and depressive symptoms in women with breast cancer - a pilot study of a non-randomised clinical trial. J Bodyw Mov Ther 22(2):460–466. https://doi.org/10.1016/j.jbmt.2017.10.003
Bruyneel A-V (2019) Effects of dance activities on patients with chronic pathologies: scoping review. Heliyon 5(7):e02104. https://doi.org/10.1016/j.heliyon.2019.e02104
Rudolph I et al (2018) Ballroom dancing as physical activity for patients with cancer: a systematic review and report of a pilot project. J Cancer Res Clin Oncol 4:759–770. https://doi.org/10.1007/s00432-018-2606-8
Pisu M et al (2017) A dance intervention for cancer survivors and their partners (RHYTHM). J Cancer Surviv 3:350. https://doi.org/10.1007/s11764-016-0593-9
Fong Yan A et al (2018) The effectiveness of dance interventions on physical health outcomes compared to other forms of physical activity: a systematic review and meta-analysis. Sports Med 48(4):933–951. https://doi.org/10.1007/s40279-017-0853-5
Rodrigues-Krause JMSP, Krause MP, Reischak-Oliveira AP (2019) Dancing for healthy aging: functional and metabolic perspectives. Altern Ther Health Med 25(1):44–63
Ryman R (1997) Royal Academy of Dancing, The Foundations of Classical Ballet Technique. Royal Academy of Dancing
Hayes S et al (2010) Upper-body morbidity following breast cancer treatment is common, may persist longer-term and adversely influences quality of life. Health Qual Life Outcomes 8(1):92. https://doi.org/10.1186/1477-7525-8-92
Bläsing B, Puttke M, and Schack T (2010) The neurocognition of dance: mind, movement and motor skills. 1st ed. 2010: Hove, East Sussex England; New York: Psychology Press. https://doi.org/10.4324/9780203852637
Ali-Haapala A, Moyle G, Kerr G (2020) Pleasurable challenges: competing with the ageing body and mind through Ballet for Seniors. Leis Stud 39(4):532–544. https://doi.org/10.1080/02614367.2019.1670720
Phillips SM et al (2017) Relationship between self-reported and objectively measured physical activity and subjective memory impairment in breast cancer survivors: role of self-efficacy, fatigue and distress. Psychooncol 26(9):1390–1399. https://doi.org/10.1002/pon.4156
Worthen-Chaudhari L et al (2019) Partnered, adapted argentine tango dance for cancer survivors: a feasibility study and pilot study of efficacy. Clin Biomech (Bristol, Avon) 70:257–264. https://doi.org/10.1016/j.clinbiomech.2019.08.010
Molinaro J, Kleinfeld M, Lebed S (1986) Physical therapy and dance in the surgical management of breast cancer. a clinical report. Phys Ther 66(6):967–969. https://doi.org/10.1093/ptj/66.6.967
Kaltsatou A, Mameletzi D, Douka S (2011) Physical and psychological benefits of a 24-week traditional dance program in breast cancer survivors. J Bodyw Mov Ther 2:162. https://doi.org/10.1016/j.jbmt.2010.03.002
Boing L et al (2017) Dance as treatment therapy in breast cancer patients – a systematic review. Rev Bras Ativ Fís Saúde 22:319–331. https://doi.org/10.12820/rbafs.v.22n4p319-331
Winters-Stone KM et al (2021) Delivering exercise medicine to cancer survivors: has COVID-19 shifted the landscape for how and who can be reached with supervised group exercise. Support Care Cancer 30(3):1–4. https://doi.org/10.1007/s00520-021-06669-w
Guidarelli C et al (2022) Remote administration of physical performance tests among persons with and without a cancer history: establishing reliability and agreement with in-person assessment. J Geriatric Oncol 13:00017. https://doi.org/10.1016/j.jgo.2022.02.002
Brady MJ et al (1997) Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. JCO 15(3):974–986. https://doi.org/10.1200/JCO.1997.15.3.974
Beaton DE et al (2001) Measuring the whole or the parts?: validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity. J Hand Ther 14(2):128–142. https://doi.org/10.1016/S0894-1130(01)80043-0
Angst F et al (2011) Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and Its Short Version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society Standardized Shoulder Assessment Form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI). Arthritis Care Res 63(S11):S174–S188. https://doi.org/10.1002/acr.20630
Craig CL et al (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395. https://doi.org/10.1249/01.Mss.0000078924.61453.Fb
American Thoracic Society (2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166(1):111–117. https://doi.org/10.1164/ajrccm.166.1.at1102
Carminatti M et al (2019) Effects of belly dancing on body image and self-esteem in women with breast cancer – pilot study. Rev Bras Med Esporte 6:464–468. https://doi.org/10.1590/1517-869220192506220067
Karkou V et al (2021) Dancing with health: quality of life and physical improvements from an EU collaborative dance programme with women following breast cancer treatment. Front Psychol 12(381):635578. https://doi.org/10.3389/fpsyg.2021.635578
Sivvas G et al (2020) The effect of a program of Greek traditional dances on fatigue in women who survived breast cancer. Arch Hell Med 37:219–226
Letton ME, Thom JM, Ward RE (2020) The effectiveness of classical ballet training on health-related outcomes: a systematic review. J Phys Act Health 17(5):566–574. https://doi.org/10.1123/jpah.2019-0303
Leite B et al (2021) Can belly dance and mat Pilates be effective for range of motion, self-esteem, and depressive symptoms of breast cancer women? Complement Ther Clin Pract 45:101483. https://doi.org/10.1016/j.ctcp.2021.101483
Stanton R et al (2020) Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health 17(11):4065. https://doi.org/10.3390/ijerph17114065
Humphries A et al (2022) Enhancing Mental Health and Social Connection Through an Acute Online Dance Intervention. PREPRINT (Version 1) available at Research Square [https://doi.org/10.21203/rs.3.rs-1149930/v1]
Acknowledgements
The authors wish to acknowledge the following study contributors: UNSW Undergraduate Exercise Physiology students Lara Alexander, Paige Winder, and Monica Dinh for their assistance with processing study questionnaire and shoulder range of motion data; UNSW StatsCentral consultant Dr Gordana Popovic for her assistance with statistical analysis; and Kathryn from the Translational Cancer Research Network Consumer Advisory Panel for her feedback regarding the design of the Ballet program. The authors also wish to thank the “Ballet after breast cancer” program participants for their invaluable contribution to the study and acknowledge the recruitment support of community breast cancer support groups and organisations including Breast Cancer Network Australia, Pink Hope Australia, Cancer Voices NSW, Cancer Council NSW, and YWCA “Encore”.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions The conduct of this study was supported by the UNSW School of Health Sciences. Eliza Macdonald received a tuition fee offset via the Australian Government Research Training Program Scholarship program. No additional funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Study conception and design were performed by Eliza Macdonald, Dr Briana Clifford, A/Prof David Simar, and Dr Rachel Ward. Material preparation and data collection were performed by Eliza Macdonald. Data analyses were performed by Eliza Macdonald and Dr Rachel Ward. The manuscript draft was prepared by Eliza Macdonald and reviewed by Dr Rachel Ward, Dr Briana Clifford, and A/Prof. David Simar. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval for this study was granted by the UNSW Human Research Ethics Committee (HC200758).
Consent to participate
Written informed consent was obtained from all study participants upon enrolment.
Consent to publish
Written informed consent to publish participant data was obtained upon enrolment. Participants provided written informed consent for the publication of images in Online Resource 1.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Macdonald, E.R., Clifford, B.K., Simar, D. et al. Ballet after breast cancer: investigating the feasibility and acceptability of a novel 16-week classical ballet intervention for breast cancer survivors. Support Care Cancer 30, 9909–9919 (2022). https://doi.org/10.1007/s00520-022-07420-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07420-9