Abstract
Purpose
To identify fall predictors and develop an assessment tool to be used for screening hospitalized cancer patients at risk for fall.
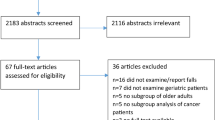
Methods
A retrospective case–control study was conducted in 2018 at a cancer center in Northern Italy. The study participants were 448 adult cancer patients admitted to the oncology ward from 2009 to 2013. The case group consisted of 112 patients presenting at least one fall, while controls were randomly chosen by matching each case for age, sex, and admission period with three patients who did not fall. Data for the fall predictors were extracted from the electronic medical records. Conditional logistic regression was used to evaluate the association between patient’s characteristics and fall risk.
Results
The overall prevalence of patients having at least one candidate fall predictor was high (98%). Seven of the studied variables showed an independent association with fall risk at multivariate analysis. These were tumor site, the presence of neurologic diseases, gait imbalance disorders, fatigue, and the assumption of certain medications such as diuretics, hypnotics, and opioids (odds ratios and 95% confidence intervals in brackets were 3.78 (1.78–8.13), 2.26 (1.08–4.77), 4.22 (1.87–9.52), 2.76 (1.45–5.26), 2.66 (1.52–4.66), 2.41 (1.20–4.85), and 3.03 (1.68–5.45), respectively).
Conclusions
In this study, we identified falling risk factors in an Italian population of hospitalized cancer patients and developed a new risk assessment tool. An external validation is necessary before implementing our screening tool in clinical practice.

Similar content being viewed by others
Data availability
All data relevant to the study are included in the article or uploaded as supplemental information. The authors confirm that the data supporting the findings of this study are available within the article (and/or) its supplemental materials. The authors have full control of primary data and agree to allow the journal to review their data if requested.
References
National Patient Safety Agency NPSA (2007) The third report from the Patient Safety Observatory: slips trips and falls in hospital available from: https://cupdf.com/document/falls.html
Mikos M, Banas T, Czerw A, Banas B, Strzępek Ł, Curyło M (2021) Hospital inpatient falls across clinical departments. Int J Environ Res Public Health 18(15):8167. https://doi.org/10.3390/ijerph18158167
Capone LJ, Albert NM, Bena JF, Tang AS (2012) Predictors of a fall event in hospitalized patients with cancer. Oncol Nurs Forum 39(5):E407–E415. https://doi.org/10.1188/12.ONF.E407-E415
Allan-Gibbs R (2010) Falls and hospitalized patients with cancer: a review of the literature. Clin J Oncol 14(6):784–792. https://doi.org/10.1188/10.CJON.784-792
Spoelstra SL, Given BA, Schutte DL, Sikorskii A, You M, Given CW (2013) Do older adults with cancer fall more often? A comparative analysis of falls in those with and without cancer. Oncol Nurs Forum 40(2):E69-78. https://doi.org/10.1188/13.ONF.E69-E78
Holley S (2002) A look at the problem of falls among people with cancer. Clin J Oncol Nurs 6(4):193–197. https://doi.org/10.1188/02.CJON.193-197
O’Connell B, Cockayne M, Wellman D, Baker L (2005) Fall risk factors and the nature of falls in inpatient oncology and palliative care settings. Contemp Nurse 18(3):247–257. https://doi.org/10.5172/conu.18.3.247
Pautex S, Herrmann FR, Zulian GB (2008) Factors associated with falls in patients with cancer hospitalized for palliative care. J Palliat Med 11(6):878–884. https://doi.org/10.1089/jpm.2007.0241
Stone CA, Lawlor PG, Kenny RA (2011) How to identify patients with cancer at risk of falling: a review of the evidence. J Palliat Med 14(2):221–230. https://doi.org/10.1089/jpm.2010.0326
Wildes TM, Dua P, Fowler SA, Miller JP, Carpenter CR, Avidan MS, Stark S (2015) Systematic review of falls in older adults with cancer. J Geriatr Oncol 6(1):70–83. https://doi.org/10.1016/j.jgo.2014.10.003
Weed-Pfaff SH, Nutter B, Bena JF, Forney J, Field R, Szoka L, Karius D, Akins P, Colvin CM, Albert NM (2016) Validation of predictors of fall events in hospitalized patients with cancer. Clin J Oncol Nurs 20(5):E126–E131. https://doi.org/10.1188/16.CJON.E126-E131
Tsai LY, Campbell M, Chen CJ, Hsieh RK, Chien HH, Tsai JM (2017) Falls and related injuries in hospitalized patients with cancer in Taiwan. J Nurs Res 4:310–318. https://doi.org/10.1097/JNR.0000000000000174
Jun MD, Lee KM, Park SA (2018) Risk factors of falls among inpatients with cancer. Int Nurs Rev 65(2):254–261. https://doi.org/10.1111/inr.12381
Zhang X, Sun M, Liu S, Leung CH, Pang L, Popat UR, Champlin R, Holmes HM, Valero V, Dinney CP, Tripathy D, Edwards BJ (2018) Risk factors for falls in older patients with cancer. BMJ Support Palliat Care 8(1):34–37. https://doi.org/10.1136/bmjspcare-2017-001388
Lorca LA, Sacomori C, Balagué-Ávila VP, Pino-Márquez LP, Quiroz-Vidal FA, Ortega L (2019) Incidence and risk of falls in patients treated for hematologic malignancies in the intensive hematology unit. Rev Lat Am Enfermagem 29(27):e3145. https://doi.org/10.1590/1518-8345.2953-3145
Sattar S, Alibhai SM, Spoelstra SL, Fazelzad R, Puts MT (2016) Falls in older adults with cancer: a systematic review of prevalence, injurious falls, and impact on cancer treatment. Support Care Cancer 24(10):4459–4469. https://doi.org/10.1007/s00520-016-3342-8
Sattar S, Kenis C, Haase K, Burhenn P, Stolz-Baskett P, Milisen K, Ayala AP, Puts MTE (2020) Falls in older patients with cancer: Nursing and Allied Health Group of International Society of Geriatric Oncology review paper. J Geriatr Oncol 11(1):1–7. https://doi.org/10.1016/j.jgo.2019.03.020
Sattar S, Haase K, Kuster S, Puts M, Spoelstra S, Bradley C, Wildes TM, Alibhai S (2021) Falls in older adults with cancer: an updated systematic review of prevalence, injurious falls, and impact on cancer treatment. Support Care Cancer 29(1):21–33. https://doi.org/10.1007/s00520-020-05619-2
Lamb SE, Jørstad-Stein EC, Hauer K, Becker C, Prevention of Falls Network Europe and Outcomes Consensus Group (2005) Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc 53(9):1618–1622. https://doi.org/10.1111/j.1532-5415.2005.53455.x
Burns Z, Khasnabish S, Hurley AC et al (2020) Classification of Injurious Fall Severity in Hospitalized Adults. J Gerontol A Biol Sci Med Sci 25;75(10):e138-e144. https://doi.org/10.1093/gerona/glaa004. PMID: 31907532
Health Research & Educational Trust. (2016, October). Preventing patient falls: a systematic approach from the Joint Commission Center for Transforming Healthcare project. Chicago, IL: Health Research & Educational Trust. https://www.aha.org/ahahret-guides/2016-10-04-preventing-patient-falls. Accessed 26 June 2021
NICE (2019). Delirium: prevention, diagnosis and management. Available from: www.nice.org.uk/CG103. Accessed 26 June 2021
Pepe MS, Fan J, Seymour CW (2013) Estimating the receiver operating characteristic curve in studies that match controls to cases on covariates. Acad Radiol 20(7):863–873. https://doi.org/10.1016/j.acra.2013.03.004
Fischer ID, Krauss MJ, Dunagan WC, Birge S, Hitcho E, Johnson S, Costantinou E, Fraser VJ (2005) Patterns and predictors of inpatient falls and fall-related injuries in a large academic hospital. Infect Control Hosp Epidemiol 26(10):822–827. https://doi.org/10.1086/502500
Dharmarajan TS, Avula S, Norkus EP (2007) Anemia increases risk for falls in hospitalized older adults: an evaluation of falls in 362 hospitalized, ambulatory, long-term care, and community patients. J Am Med Dir Assoc 8(3 Suppl 2):e9–e15. https://doi.org/10.1016/j.jamda.2006.12.015
Winters-Stone KM, Horak F, Jacobs PG, Trubowitz P, Dieckmann NF, Stoyles S, Faithfull S (2017) Falls, functioning, and disability among women with persistent symptoms of chemotherapy-induced peripheral neuropathy. J Clin Oncol 10;35(23):2604–2612. https://doi.org/10.1200/JCO.2016.71.3552
Gewandter JS, Fan L, Magnuson A, Mustian K, Peppone L, Heckler C, Hopkins J, Tejani M, Morrow GR, Mohile SG (2013) Falls and functional impairments in cancer survivors with chemotherapy-induced peripheral neuropathy (CIPN): a University of Rochester CCOP study. Support Care Cancer 21(7):2059–2066. https://doi.org/10.1007/s00520-013-1766-y
Tofthagen C, Overcash J, Kip K (2012) Falls in persons with chemotherapy-induced peripheral neuropathy. Support Care Cancer 20(3):583–589. https://doi.org/10.1007/s00520-011-1127-7
Vela CM, Grate LM, McBride A, Devine S, Andritsos LA (2018) A retrospective review of fall risk factors in the bone marrow transplant inpatient service. J Oncol Pharm Pract 24(4):272–280. https://doi.org/10.1177/1078155217697485
Li Y, Zhang Q, Yang X, Zheng L, Yang J, Zhao H, Yang D (2018) Research of falls risk of taking central nervous system drugs in oncology inpatients. Curr Probl Cancer 42(2):261–267. https://doi.org/10.1016/j.currproblcancer.2018.01.008
Herzig SJ, Rothberg MB, Moss CR, Maddaleni G, Bertisch SM, Wong J, Zhou W, Ngo L, Anderson TS, Gurwitz JH, Marcantonio ER (2021) Risk of in-hospital falls among medications commonly used for insomnia in hospitalized patients. Sleep 13;44(9):zsab064. https://doi.org/10.1093/sleep/zsab064
DECRETO LEGISLATIVO 10 agosto 2018, n. 101 “Disposizioni per l'adeguamento della normativa nazionale alle disposizioni del regolamento (UE) 2016/679 del Parlamento europeo e del Consiglio, del 27 aprile 2016, relativo alla protezione delle persone fisiche con riguardo al trattamento dei dati personali, nonche' alla libera circolazione di tali dati e che abroga la direttiva 95/46/CE (regolamento generale sulla protezione dei dati). Retrieved from https://www.gazzettaufficiale.it/eli/id/2018/09/04/18G00129/sg Accessed 26 June 2021
Acknowledgements
The authors are grateful to Ing. Nicola Gentili for providing the electronic selection of controls.
Author information
Authors and Affiliations
Contributions
AZ, SM, GM, and MTM designed the study and provided the training of research nurses involved in the study. MG, GM, and IM were involved in data collection and registration. EP was responsible for data analysis. AZ, ON, and EP contributed to the drafting of the manuscript and all authors critically reviewed the draft and approved the final version for submission.
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by the relevant medical, scientific, and ethics committees of Area Vasta of Romagna (Prot. N. 2741/2013/1.5/113) and has been conducted in accordance with good clinical practice and the principles of the Helsinki Declaration.
Consent to participate
Given the retrospective nature of the study, it was not possible to obtain the informed consensus from patients because most of them were not reachable (dead or in critical conditions). In research centers and universities in Italy, the use of patient data for research purposes can be authorized by the General patients Authorization 2018 [32].
Consent for publication
Not applicable. Specific precautions were put in place to warranty the confidentiality of participants. In particular, the study data extracted from the EMRs were initially registered in a dedicated encrypted database with limited access to study nurses only. The completed database was permanently anonymized by deleting patients’ identity data and by assigning a unique numerical code to each study participant.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zeneli, A., Montalti, S., Masciangelo, I. et al. Fall predictors in hospitalized patients living with cancer: a case–control study. Support Care Cancer 30, 7835–7843 (2022). https://doi.org/10.1007/s00520-022-07208-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07208-x