Abstract
Introduction
Nowadays, more than 80% of newly diagnosed classical Hodgkin lymphoma (HL) patients can be cured and become long-term survivors due to risk and response-adapted treatment strategies. A well-known side effect is cognitive dysfunction that appears in HL patients after chemotherapy. In the present study, we aimed to measure cognitive dysfunction in our HL patients in this study and to find potential correlations between patient-related factors, the signs and symptoms of their diseases, or therapeutic factors.
Methods
We carried out a computer-assisted assessment (CANTAB) of cognitive dysfunction in 118 patients. We examined the domains of visual memory, attention, working memory, and planning.
Results
The median age of 64 females and 54 males at diagnosis was 29 (13–74) and 41 (21–81) years at the completion of CANTAB. Fifty-two percent of all patients showed cognitive impairment. Attention was impaired in 35% of patients, the working memory and planning were impaired in 25%, while visual memory was affected in 22%. All the three functions showed a significant association with inactive employments status. A close correlation was found between visual memory/working memory and planning, higher age at HL diagnosis or the completion of CANTAB test, and disability pensioner status.
Discussion
Our investigation suggests that patients with inactive employment status and older age require enhanced attention. Their cognitive function and quality of life can be improved if they return to work or, if it is not possible, they receive a cognitive training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hodgkin lymphoma (HL) primarily affects active young adults: a significant portion of patients were working-age young adults at the time of diagnosis. Therefore, the social and economic implications of the disease outweigh its incidence rate. In 2020, 83087 new HL patients were diagnosed worldwide, and thus HL accounted for 0.4% of total cancer cases [1]. The incidence rate is 2–3/100,000 inhabitants in Hungary, which means approximately 2–300 newly diagnosed cases each year [2, 3]. Due to up-to-date methods of clinical investigation and risk- and response-adapted therapy, more than 80% of patients with HL show long-term survival and recovery. Parallel to this, treatment-related long-term complications have come to the fore. The long-term survival rate is mainly decreased by developing second malignancies and the appearance of organ damage (heart, lungs, thyroid gland, etc.). Nowadays, the quality of survivorship is becoming more prominent. Therefore, treatment-related side effects must be focused on, but health-related quality of life and patients’ return to work after successful treatment should also be considered [4]. Based on literature data, cancer-related cognitive impairment (CRCI) is a common adverse effect experienced by patients during and after chemotherapy (chemobrain) for non-central nervous system cancer/lymphoma [5]. Many factors influence CRCI. Treatment-related factors include the type of chemotherapy and its direct and indirect neurotoxicity caused by these, which can occur even if the blood-brain barrier is intact. Non-chemotherapy-related factors include age, education, depression, and psychological stress. In addition, the type of disease must also be considered, as not all hematological disorders require immediate treatment (indolent malignancies) [6,7,8]. CRCI mainly affects the functions of the domains of attention, working memory, and planning [7, 9, 10]. There are few published data available on cured HL patients [6, 11, 12]. Our study aimed to measure cognitive dysfunction in our regularly followed-up HL patients, finding potential correlations between patient-related factors, specific signs and symptoms of their diseases, and therapeutic factors.
Methods
Subjects and data collection
A cross-sectional survey was conducted at the Division of Hematology of the University of Debrecen. We designed the study for approximately 100 of the 301 patients who had been regularly followed up. Exclusion criteria were lack of signed informed consent, age under 18 years at the time of the survey, and the presence of central and peripheral nervous system involvement with HL. Altogether, 118 adult HL survivors were identified between June 1, 2012, and January 31, 2016, at our outpatient clinic diagnosed with HL between January 1, 1969, and July 1, 2013. Age, gender distribution, clinical stage, and type of treatment of the selected patients were no different from that of our population of Hodgkin lymphoma patients. Based on the hospital records of the patients, diseases diagnosed before the initiation of HL treatment were defined as comorbidities, whereas treatment-related side effects were defined as conditions diagnosed in the follow-up phase after HL treatment.
Treatment protocols
Primary chemotherapy involved CV(O)PP (cyclophosphamide, vinblastine (vincristine), procarbazine, and prednisolone) before. After 1990, COPP/ABV (cyclophosphamide, vincristine, procarbazine, prednisolone/adriamycin, bleomycin, and vinblastine) was used. Since 1999, the ABVD (adriamycin, bleomycin, vinblastine, and dacarbazine) protocol has been most frequently applied. In cases of relapse, DHAP (dexamethasone, cytarabine, and cisplatin), ICE (ifosfamide, carboplatin, etoposide), or IGEV (ifosfamide, gemcitabine, vinorelbine) regimens and autologous hemopoetic stem cell transplant are included. Radiotherapy of the involved or extended field, mantle, and inversed Y or (sub)total nodal type was administered by a telecobalt device before, 2000, and by a linear accelerator afterwards. Extended and involved-field radiotherapy was used before (mean dose, 40 Gy) and after 1998 (mean dose, 33 Gy), respectively (Supplementary Table 1).
Study design and assessment
Subjects were asked to perform a series of 13 computerized neuropsychological tests of the Cambridge Neuropsychological Test Automated Battery (CANTAB, Cambridge Cognition, Cambridge, UK). CANTAB has been used and proved to be a useful tool to assess cognitive functions in various neurological and psychiatric disorders [13, 14]. Subjects were seated at a comfortable height, approximately 0.5 m from the monitor, and were instructed to carry out the tasks by touching the screen. After an initial explanation and completing a simple “motor screening task” successfully (touching the center point of flashing crosses on the screen), subjects were given the following tests in the following order (the technical description of the tests can be found on the Cambridge Cognition’s website: http://www.cantab.com):
-
Big Little Circle (BLC): a two-stimuli visual discrimination and category achievement test. Spatial working memory (SWM): this task assesses the subject’s ability to retain spatial information and manipulate remembered items in working memory.
-
Reaction time (RTI): The task is designed to measure the subject’s speed of response to a visual target where the stimulus is either predictable (simple reaction time) or unpredictable (choice reaction time). A manual switch is used for the task.
-
Spatial span (SSP): A computerized version of the Corsi blocks, a test of span for spatial items similar to “digit span” tests for verbal items.
-
Pattern recognition memory (PRM): An examination of visual recognition memory in a 2-choice forced discrimination paradigm.
-
Spatial recognition memory (SRM): This task tests visual-spatial memory in a 2-choice forced discrimination paradigm.
-
Paired associate learning (PAL): Assessment of simple visual pattern and visuospatial associative learning, which contains aspects of a delayed response procedure and a conditional learning task. Successful performance in the PAL test requires both the elaboration of “frontal strategies” and the “mnemonic processes” of the medial temporal lobe. They should pay attention to both the stimuli and their spatial position.
-
Intra/extradimensional shift task (IED): A test of rule acquisition and reversal, featuring visual discrimination and attentional set-shifting and analogous to a category change in the Wisconsin Card Sorting Test.
-
Match to sample visual search (MTS): A two-stimuli visual discrimination and category achievement test.
-
Delayed matching to sample (DMS): This task tests visual memory in a 4-choice delayed recognition memory paradigm.
-
Stockings of Cambridge (SOC): The task is analogous to the “Tower of London” test and assesses the subject’s ability to engage in spatial problem-solving. This test makes substantial demands on executive function.
-
Rapid visual information processing (RVP): It is a visual continuous performance task, using digits rather than letters. Results were compared to the internal normative database of CANTAB, involving 3,000 healthy volunteers, and were matched for age groups and gender. CANTAB tests were previously validated among healthy Hungarian volunteers showing no statistically significant differences in the cognitive performance compared to the internal normative database [13, 15].
We examined the domains of visual memory (PAL, DMS, SRM), functions of attention (IED, RTI, RVP, PRM), working memory, and planning (SSP, SWM, SOC). Although the CANTAB battery emphasizes assessment of frontostriatal functions (SWM, IED, SOC, and SWP), it also includes tests sensitive to temporal lobe (PAL, DMS, PRM, SSP) function [16].
Questionnaires
HL survivors were asked to complete a standardized, self-administered, and validated Hungarian questionnaire, which included items on socio-demographic status (place of residence, marital status, educational level, employment, important life events after lymphoma treatment) and psychiatric treatment (date and type of medication) at the time of diagnosis, as well as the scales listed below. Data on the disease and its treatment were based on hospital records.
The Hungarian version of the Hospital Anxiety and Depression Scale (HADS-14) has been used in studies of distress among cancer patients in general. Each of the 14 items is scored on a 4-point scale (0–3). Sum scores for the anxiety and depression subscales are calculated by simple addition. The constructors of HADS recommended two possible cut-offs (8 or higher or 11 or higher on either scale) for case definition. In this study, caseness refers to the lower cut-off [17, 18].
The General Health Questionnaire (GHQ-12) is the most extensively used screening instrument for common mental disorders, in addition to being a general measure of psychiatric well-being. Each item is scored on a 4-point scale (corresponding to a symptom present: “not at all,” “same as usual,” “rather more than usual,” or “much more than usual”). It can be scored in a bimodal fashion (0–0–1–1), when final scores range from 0 to 12. According to this method, patients scoring five or more are considered: at risk of anxiety/depression [19].
The validated Hungarian version of the abbreviated Sense of Coherence (SOC-13) scale was used in the present survey to measure the overall capacity to cope with stressful situations. All 13 items are answerable on a Likert scale from 1 to 7, and total scores vary between 13 and 91. A higher score indicates a stronger SOC [19].
The Perceived Stress Scale (PSS) is the most widely used psychological instrument for measuring stress perception. Scores for the 4-item form range from 0 to 16. Potential responses range from 0 (never) to 4 (very often), and positively stated items are reverse coded before items are summed up with higher scores indicating more perceived stress [20].
The Dysfunctional Attitude Scale form A (DAS-A) is designed to measure the presence and intensity of dysfunctional attitudes. The higher the score, the more dysfunctional attitudes are characteristic of an individual. The 17 items are divided into two subscales: perfectionism and dependency. Each item is scored on a Likert scale from 1 to 7. Sum scores for either subscale are calculated by simple addition [21]. All questionnaires employed in the survey have been validated and extensively used in the international literature [22,23,24,25].
Statistical analysis
Statistical analysis was performed using IBM SPSS 26 software. Data are described by the mean, standard deviation frequencies, and percentages. Categorical variables were compared between groups using chi-squared or Fisher’s exact test, as appropriate. Continuous variables were evaluated by independent samples t-test, Mann-Whitney test, and ANOVA or Kruskal-Wallis test. Spearman’s correlations were used measuring the relationship between two variables. Multiple/binary logistic regression (enter and forward likelihood ratio methods) was performed among HL survivors to identify predictors of cognitive dysfunctions. Odds ratios (OR) with 95% confidence intervals (CI) were estimated for the logistic regression models. Significance level was set at p<0.05. Since no control group was available, the participants’ Z-scores of all CANTAB subtests were calculated from median scores based on the normative database of 3000 healthy volunteers. The index scores of the patients and those of the normative database were compared using a one-tailed non-parametric t-test. Statistical analysis was carried out using GraphPad Prism 4.00 for Windows software (GraphPad Software, San Diego, CA, USA, http://www.graphpad.com). We regarded as having reduced cognitive function patients who performed worse than the normal population by 1.5 standard deviations or if the results of at least one test were already positive [9].
Results
Patient characteristics
One hundred twenty patients were asked to participate in our study. The refusal rate was below 5%. A total of 118 adult HL survivors completed the survey (64 females, 54%). The median age of the survivors at the time of diagnosis was 29 years at the time of diagnosis (range 13–74) and 41 years when the neurocognitive survey was performed (range 21–81). After the diagnosis, this investigation took place 11 years (range 0.4–44). The baseline characteristics of the survivors are presented in Table 1.
The measurement of neurocognitive function
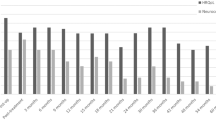
The pattern of median Z-scores of the CANTAB tests and their difference from the control scores measured in subjects with HL are presented in Figure 1.
Difference between HL survivors (n=118) and the control CANTAB volunteers. DMS, simultaneous and delayed matching; PAL, paired association learning; SRM, spatial recognition memory; IED, intra/extra dimensional shift; PRM, pattern recognition memory; RTI, reaction time; RVP, rapid visual information processing; SOC, stocking of Cambridge; SSP, spatial span; SWM, spatial working memory
As a next step, we investigated whether there are associations between positive neurocognitive subtest results (visual paired associate learning, reaction time and psychomotor speed, rapid visual processing) and patient-related factors, specific signs and symptoms of their diseases, or therapeutic factors. The PAL test was found significantly impaired in HL subjects at an older age at diagnosis and completion of the survey. The performance on RTI was prolonged in patients who were at an advanced stage with higher ECOG PS at diagnosis. A psychomotor RTI was strongly associated with the advanced stage at diagnosis. RVP test detected a significant impairment in patients at an older age at the time of HL diagnosis or when the survey was completed in village dwellers and patients with inactive employment status. These results are presented in Supplementary Table 2.
Fifty-two percent of all patients (n=62) showed cognitive impairment based on at least one positive subtest. Attention was impaired in 35% (42/118) of patients. Working memory and planning were damaged in 25% (30/118), while the visual memory was affected in 22% (26/118 patients) (Figure 2). One domain was found positive in 36 patients (30%, 36/118), two domains in 16 patients (14%, 16/118), and three in 10 patients (8%, 10/118). We defined severe mental vulnerability as having abnormal cognitive functions in all the three domains. The ten most affected HL survivors were at an older age at HL diagnosis (>=30 years, p<0.001) or when the survey was completed (>=40 years, p<0.001), had disability pension status (p=0.044), or used central nervous system drug (p=0.0239) (data not shown).
All three cognitive domain’s functions showed significant correlations with inactive employment status. On the one hand, a close correlation was found between visual memory and age at diagnosis, the time of examination, and disability pension status. On the other hand, working memory and planning showed a close association with the age at diagnosis, the time of examination, and disability pension status (Table 2.).
Independent predictive factors for domains of cognitive functions
Multivariate logistic regression analysis was carried out by starting with all potential determinant variables and eliminating the non-significant ones. Independent variables of visual memory and working memory/planning were age at diagnosis of HL and the age when the CANTAB survey was performed. The functions of all the three cognitive domains were associated with inactive employment status (Table 3).
Correlation between cognitive function tests and mental health questionnaires
The correlation between the cognitive and mental health tests is summarized in Table 4. Unfortunately, due to printing error, item 10 in the HADS questionnaire was missing 2 answer options (labeled 2 and 3). Twenty-eight percent of patients (n=33) gave a positive answer (greater than 0) to the question printed incorrectly. If the additional questions 2 and 3 had received a positive response, our results could have been further improved. Misprinting of the question could not have led to a false-positive result due to the nature of the questionnaire.
Discussion
Treatment of HL has become one of the success stories of oncohematology over the past decades. This has resulted in a continuously increasing HL survivor rates in patients at risk for long-term complications and health-related quality-of-life impairment. HL primarily affects active young adults: the median age of a significant portion of patients at the time of diagnosis was around 40 years. Therefore, the social and economic implications of the disease outweigh its incidence rate [26, 27]. Neuropsychological (NP) studies have shown cognitive dysfunction in 13–70% of patients receiving chemotherapy (solid cancers/hematological malignancies). However, 15–35% may experience permanent deficits well beyond the active treatment phase [28, 29]. CRCI is associated with a decrease in quality of life; reduced ability to work, read, or drive; and decreased social functioning. A significant proportion of clinical trials were performed among solid cancer patients (the most common type of breast cancer). However, most clinical trials in hematological disorders focus on survivors of acute lymphoblastic leukemia and primary central nervous system lymphoma [6, 30].33 There are few published data available on HL survivors [6, 11, 12, 31].
The present study results show that several cognitive domains are already impaired in long-term HL survivors. These data are consistent with the findings of previous studies [5, 11, 32, 33], made among survivors examined at least 5 years after completing chemotherapy. Based on the results of reaction time (RTI) and psychomotor speed subtests, there was a clear association with the advanced stage, which might emphasize the role and the cycles of chemotherapies among HL survivors. Our findings regarding reaction time are similar to preliminary data [12, 34], which had detected that receiving a lower number of chemotherapy cycles was associated with better neurocognitive performance. There are no literature data on ECOG PS in HL patients.
More than half of our long-term HL patients (52%, n=62) showed impairment based on at least one cognitive domain. Attention (and processing speed) was impaired in 35% of patients, working memory and planning (executive function) were damaged in 25%, while visual memory (memory and learning) was affected in 22%. A research group from Israel found impaired cognitive functions by CANTAB among their HL survivors (51 patients): executive functions were damaged in 41% of subjects, memory and learning in 28%, processing speed in 22%, and attention in 12%. Treatment completion of HL survivors was 6 months to 5 years [12]. Mariegaard et al. published that 39% of lymphoma survivors (115 patients, 65 with HL) showed impairment on executive function tests made with self-reported cognitive questionnaires (the mean period time elapsed after the completion of treatment was 29.6 months [31]. The remarkable differences between executive functions might be related to the period time elapsed from the treatment.
We identified associations between objective neurocognitive deficits (all three cognitive domains) and inactive employment status. Krull et al. reported favorable data on employment status and cognitive dysfunction in childhood HL survivors. Their analysis revealed that unemployed status (10 patients, compared with employed survivors) was related to significantly reduced motor speed, more severe impairments in working memory, and task efficiency [33]. Kiserud et al. reported that 102 unemployed people of 281 subjects with long-term survival after autologous hemopoietic stem cell transplant had poorer cognitive functions. Ehrhard et al. also confirmed that unemployed childhood non-Hodgkin lymphoma (NHL) survivors (187 patients) showed reduced processing speed, similar to our findings [35].
According to our results, being older at diagnosis or when completing the survey and disability pension status was related to poorer cognitive function. Preliminary data suggest that cancer and its treatment may compromise the normal aging process and increase cognitive impairment in those who are at the age of 65 years or older [11, 36]. However, the majority of HL survivors were in early and middle adulthood, so further research will have to justify additional factors which might lead to cognitive impairment.
We demonstrated significant reductions across a number of HRQOL domains in long-term HL survivors, which was related to neurocognitive impairment. The depression scale of HADS is correlated with reaction time assessments. At this time, we do not know that reduced cognitive function is a consequence or the cause of depression. The results published by Ehrhardt et al. suggest that objectively measured processing speed and survivor-reported executive function are associated with worse HRQOL among NHL survivors [37]. An Italian research group published that both subjectively and objectively assessed cognitive measures correlated negatively with most assessed HRQOL domains, indicating that the quality of life is worse when cognitive functioning is poor [38]. Based on previous results, impaired cognitive functions and poorer mental health might have a strong relationship. Recent data supporting a trend toward improved neurocognitive function after cognitive rehabilitation may provide means to find early detection and intervention strategies to improve HRQOL impairment among long-term lymphoma (HL) survivors [37, 39].
Our study is not without limitations. The main limitations of this research were its cross-sectional design, the absence of baseline neuropsychiatric (NP) tests, lack of matched healthy control population, and neuroimaging examination.
Conclusions
According to literature data, NP tests to measure cognitive function often take more than 4 h and require trained investigators. CANTAB is a simple NP test, covering a wide range of cognition (visual memory, attention, work memory, and planning function), independent of language and culture, and can be performed within 2 h. Our analysis showed a clear association between clinical stage and reaction time, emphasizing the role of the number of chemotherapy cycles. Attention impairments were the most pronounced in our patients. Our investigation suggests that an older age and inactive employment status require enhanced attention. Their cognitive functions and, through that, their quality of life can be improved if they return to work or, if it is not possible, they may receive cognitive training. Our results draw attention to the fact that cognitive impairment is a real problem in patients with cured HL, similarly to other malignant diseases. Further longitudinal clinical studies could help characterize the neurocognitive outcomes of HL survivors.
Code availability
Not applicable.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
Cancer Registry of National Institute of Oncology. Rákregiszter Statisztika, www.onkol.hu/en/rakregiszter-statisztika (Accessed 1 Aug 2019).
Pinczés L, Miltényi Z, Jóna Á et al (2016) How the epidemiology of Hodgkin lymphoma changed in Debrecen, Hungary. Med Res Arch 4:1–13
Magyari F, Kósa K, Berecz R et al Employment status and health related quality of life among Hodgkin-lymphoma survivors’- results based on data from a major treatment center in Hungary. Health Qual Life Outcomes 15. https://doi.org/10.1186/s12955-017-0758-x
Ahles TA, Saykin AJ, Furstenberg CT et al (2002) Neuropsychologic impact of standard-dose systemic chemotherapy in long-term survivors of breast cancer and lymphoma. J Clin Oncol 20:485–493
Williams AM, Zent CS, Janelsins MC (2016) What is known and unknown about chemotherapy-related cognitive impairment in patients with haematological malignancies and areas of needed research. Br J Haematol 174:835–846
Pendergrass JC, Targum SD, Harrison JE (2018) Cognitive impairment associated with cancer: a brief review. Innov Clin Neurosci 15:36–44
Franceschetti S, Annunziata MA, Agostinelli G et al (2021) Late neurological and cognitive sequelae and long-term monitoring of classical Hodgkin lymphoma and diffuse large b-cell lymphoma survivors: a systematic review by the Fondazione Italiana Linfomi. Cancers (Basel) 13:3401
Wefel JS, Vardy J, Ahles T et al (2011) International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol 12:703–708
Allegra A, Innao V, Basile G et al Post-chemotherapy cognitive impairment in hematological patients: current understanding of chemobrain in hematology. Expert Rev Hematol 13. https://doi.org/10.1080/17474086.2020.1738213
Wouters H, Baars JW, Schagen SB (2016) Neurocognitive function of lymphoma patients after treatment with chemotherapy. Acta Oncol 1–5
Trachtenberg E, Mashiach T, Ben Hayun R et al (2018) Cognitive impairment in Hodgkin lymphoma survivors. Br J Haematol 182:670–678
Bartók E, Berecz R, Glaub T et al (2001) Számítógépes neurokognitív vizsgálati programcsomag magyarországi validálása. Validation of the computerized neurocognitive test battery (CANTAB) in Hungary. Psychiatr Hung 16:125–133
Foltynie T, Brayne CEG, Robbins TW et al (2004) The cognitive ability of an incident cohort of Parkinson’s patients in the UK. The CamPaIGN study. Brain 127:550–560
Égerházi A, Berecz R, Bartók E et al (2007) Automated neuropsychological test battery (CANTAB) in mild cognitive impairment and in Alzheimer’s disease. Prog Neuro-Psychopharmacol Biol Psychiatry 31:746–751
Sweeney JA, Kmiec JA, Kupfer DJ (2000) Neurological impairments in bipolar and unipolar mood disorders on the CANTAB neurocognitive battery. Biol Psychiatry 48:674–684. https://doi.org/10.1016/s0006-3223(00)009100
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Muszbek K, Szekely A, Balogh ÉM et al (2006) Validation of the Hungarian translation of hospital anxiety and depression scale. Qual Life Res. https://doi.org/10.1007/s11136-005-3627-8
Balajti I, Vokó Z, Ádány R et al Validation of the Hungarian versions of the abbreviated sense of coherence (SOC) scale and the general health questionnaire (GHQ-12). Mentálhigiéné Pszichoszomatika. https://doi.org/10.1556/mental.8.2007.2.4
Stauder A, Konkoly-Thege B (2006) Characteristics of the Hungarian version of the perceived stress scale (PSS). Mentalhig Pszichoszomatika 7:203–216
Weissman Arlene NBAT (2007) The dysfunctional attitude scale. In: Perczel Forintos Dóra KZAG (ed) Questioners in clinical psychology (Hungarian). Budapest, Budapest
Annunziata MA, Muzzatti B, Altoé G (2011) Defining hospital anxiety and depression scale (HADS) structure by confirmatory factor analysis: a contribution to validation for oncological settings. Ann Oncol 22:2330–2333
De Fazio P, Cerminara G, Ruberto S et al (2017) Hospitalization and other risk factors for depressive and anxious symptoms in oncological and non-oncological patients. Psychooncology 26:493–499
Hall DL, Lennes IT, Pirl WF et al (2017) Fear of recurrence or progression as a link between somatic symptoms and perceived stress among cancer survivors. Support Care Cancer 25:1401–1407
Hu K, Eriksson M, Wengström Y et al (2020) Sense of coherence and risk of breast cancer. Elife 9:e61469
Smith A, Crouch S, Lax S et al (2015) Lymphoma incidence, survival and prevalence 2004-2014: sub-type analyses from the UK’s Haematological Malignancy Research Network. Br J Cancer 112:1575–1584
Halbsguth TV, FH-H (2015) In: Andreas E, Younes A (eds) Hodgkin lymphoma: a comprehensive overview. Quality of life (chapter). Springer, pp 365–373
Janelsins MC, Kesler SR, Ahles TA et al (2014) Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int Rev Psychiatry 26:102–113
Asher A, Myers JS (2015) The effect of cancer treatment on cognitive function. Clin Adv Hematol Oncol 13:441–450
Wefel JS, Kesler SR, Noll KR et al (2015) Clinical characteristics, pathophysiology, and management of noncentral nervous system cancer-related cognitive impairment in adults. CA Cancer J Clin 65:123–138
Mariegaard J, Wenstrup J, Lim KZM et al Prevalence of cognitive impairment and its relation to mental health in Danish lymphoma survivors. Support Care Cancer 29. https://doi.org/10.1007/s00520-020-05857-4
Joly F, Henry-Amar M, Arveux P et al (1996) Late psychosocial sequelae in Hodgkin’s disease survivors: a French population-based case-control study. J Clin Oncol 14:2444–2453
Krull KR, Sabin ND, Reddick WE et al (2012) Neurocognitive function and CNS integrity in adult survivors of childhood Hodgkin lymphoma. J Clin Oncol 30:3618–3624
Baudino B, D’agata F, Caroppo P et al (2012) The chemotherapy long-term effect on cognitive functions and brain metabolism in lymphoma patients. Q J Nucl Med Mol Imaging Off Publ Ital Assoc Nucl Med [and] Int Assoc Radiopharmacol (IAR) [and] Sect Soc Radiopharm 56:559–568
Kiserud CE, Fagerli UM, Smeland KB et al Pattern of employment and associated factors in long-term lymphoma survivors 10 years after high-dose chemotherapy with autologous stem cell transplantation. Acta Oncol (Madr) 55. https://doi.org/10.3109/0284186X.2015.1125015
Mandelblatt JS, Jacobsen PB, Ahles T Cognitive effects of cancer systemic therapy : implications for the care of older patients and survivors. 32. https://doi.org/10.1200/JCO.2014.55.1259
Ehrhardt MJ, Mulrooney DA, Li C et al Neurocognitive, psychosocial, and quality-of-life outcomes in adult survivors of childhood non-Hodgkin lymphoma. Cancer 124. https://doi.org/10.1002/cncr.31019
Muzzatti B, Cattaruzza N, Piccinin M et al Cognitive function in long-term lymphoma survivors: relationship between subjective reports and objective assessments and with quality of life. Psychol Health Med. https://doi.org/10.1080/13548506.2020.1770815
Zeng Y, Cheng ASK, Chan CCH Meta-analysis of the effects of neuropsychological interventions on cognitive function in non-central nervous system cancer survivors. Integr Cancer Ther 15. https://doi.org/10.1177/1534735416638737
Acknowledgements
We want to thank all patients who so generously participated in this study. The authors would like to acknowledge Katalin Hodosi for her support in the statistical analysis.
Funding
Open access funding provided by University of Debrecen.
Author information
Authors and Affiliations
Contributions
Data was analyzed by FM, AI, TI, and IV. The paper was written by FM and IV. The study was supervised by KK, RB, and AÉ. The manuscript was approved by ZSM, ZSS and ÁI. FM and IV contributed equally to this study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for the study was obtained from the certified Medical Ethics Committee of the University of Debrecen, Hungary. The participating patients signed the consent.
Consent to participate
The participating patients signed the consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

Supplementary Table 1.
The treatment protocols based on the stage of the disease A(E)BVD: adriamycin (epirubicin), bleomycin, vinblastine, and dacarbazine; CV(O)PP: cyclophosphamide, vinblastine [vincristine], procarbazine, and prednisolone; COPP/ABV: cyclophosphamide, vincristine, procarbazine, prednisolone/adriamycin, bleomycin, and vinblastine; Other protocols include MOPP: mustargen, vincristine, procarbazin, prednisolone, OEPA: vincristine, etoposide, prednisone, and doxorubicin (PNG 57 kb)

Supplementary Table 2.
Associations between cognitive subtests results and patient/treatment-related factors among HL survivors (PNG 779 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Magyari, F., Virga, I., Simon, Z. et al. Assessment of cognitive function in long-term Hodgkin lymphoma survivors, results based on data from a major treatment center in Hungary. Support Care Cancer 30, 5249–5258 (2022). https://doi.org/10.1007/s00520-022-06918-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-06918-6