Abstract
Purpose
The Japanese Society of Medical Oncology (JSMO) published a guideline (GL) on febrile neutropenia (FN) in 2017. This study aims to identify promoting factors and disincentives for complying with GL recommendations according to attributes of doctors providing chemotherapy.
Methods
A questionnaire survey was conducted with SurveyMonkey™ for physician members of the Japanese Association of Supportive Care in Cancer and relevant academic organizations. Each question had four options (always do, do in more than half of patients, do in less than half, do not at all) and a free description form. Responses were analyzed according to the respondents’ attributes.
Result
Seven hundred eighty-eight out of retrieved 801 responses were available for analysis. Multivariable analysis demonstrated that the percentage of GL users was higher among women and Japanese Society of Clinical Oncology members. The overall compliance rate was higher among women, JSMO members, and board-certified medical oncologists. Internists emphasized the significance of collecting blood cultures at FN onset, and surgeons stressed the importance of G-CSF prophylaxis. Hematologists were less likely to adhere to recommendations on risk assessment of FN by the Multinational Association of Supportive Care in Cancer score and administration of gammaglobulin products. However, those are acceptable due to the characteristics of their practice. Eight recommendations had no difference in compliance rates between users and non-users, some of whose statements were ambiguous and discretionary.
Conclusion
Women were more likely to use and adhere to GL. The recommendations should be developed considering the characteristics of specialty and subspecialty and avoiding ambiguity and discretionary statements.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
We previously published the first report of a questionnaire survey on penetration and application of the Japanese Guidelines (GL) on febrile neutropenia (FN), and revised the second edition published by the Japanese Society of Medical Oncology (JSMO) [1]. It demonstrated that 86.7% of respondents knew and used GL; the medians of the complete and complete plus partial compliance rates, which denote the response of “always do” and “always do” plus “do in more than half of patients” in the questionnaire, were 46.4% (range: 7.0–92.8) and 77.8% (range: 35.4–98.7), respectively, in twenty recommendations. The complete compliance rates were less than 30% in seven recommendations. Some of them are feared to deteriorate the quality of FN management, such as the risk assessment of FN with the Multinational Association of Supportive Care in Cancer (MASCC) score at onset (Q2), administration of therapeutic G-CSF (Q11), and primary prophylactic G-CSF (ppG-CSF)(Q16) (Table 1, Supple Table). It is essential to know facilitating factors and disincentives affecting compliance to promote evidence-based supportive care in cancer. Some of them with low compliance rates appeared to relate to some attributes of the respondents. Link H et al. reported that adherence to guidelines was influenced by doctors’ specialty and clinical experience and chemotherapeutic regimens [2]. This study aims to identify attributes and characteristics of the respondents and features of the recommendations that affected compliance and to propose how to enhance compliance with guidelines.
Materials and methods
Design of the questionnaire
The questionnaire consisting of twenty-one questions on GL and seven on attributes of respondents was surveyed from March to May 2020 through SurveyMonkey™ for the members of the Japanese Association of Supportive Care in Cancer (JSCC), JSMO, the Japanese Society of Hematology (JSH), and the Japanese Breast Association (JBA) (Table 1). The precise methods of surveillance were reported previously [1]. Each question had four options, (1) always do, (2) do in more than half of patients, (3) do in less than half of patients, and (4) do not at all, and a free description form, except for Q1. The options of Q1 were (1) have a printed GL and apply it to clinical practice, (2) have a download format of GL and apply it to clinical practice, (3) know GL but do not use it, (4) do not know GL. Respondents who chose options 1 and 2 are defined as GL users (USR), while those who chose options 3 and 4 as non-user (NUSR). Each question asked whether a respondent does what GL recommends, except for Q11, 12, 14, and 17. The responses to those questions represent the level of compliance with GL. The answers to “always do” and “do in more than half of patients” suggest complete and partial compliance, respectively. In contrast, Q11, 12, 14, and 17 asked whether a respondent does what GL does not recommend, and the same goes for the answers to “do not at all” and “do in less than half of patients.”
Parameters for analyses
The specialties of respondents were divided into two categories: physician (PHS), meaning internist, and surgeon (SRG), who traditionally provide chemotherapy in their specialties and manage associated adverse effects, including FN. PHS was further divided into hematologist (HEM) and medical oncologist (ONC), including genuine medical oncologists, pulmonologists, gastroenterologists, pediatricians. SRG was also divided into breast surgeons (BRS) and surgeons other than breast surgery (NBS), including gastroenteric surgeons, thoracic surgeons, gynecologists, urologists. The details of respondents’ specialties were mentioned in the previous report [1]. The analyses included two societies and two certifications related to cancer chemotherapy that may influence the use and compliance. These are JSMO, which focuses on internists, and the Japanese Society of Clinical Oncology (JSCO), which focuses on surgeons, as well as the Board-Certified Medical Oncologist (BCMO) accredited by JSMO and the Board-Certified General Clinical Oncologist (BCGCO) accredited by the Japanese Board of Cancer Therapy.
Statistical analyses
The collected responses were statistically analyzed with Microsoft Excel, R, EZR [3], Python, and Statcel 3. Microsoft Excel was applied to the aggregation of the collected data and the calculation of frequency. R and EZR were used to cross-tabulation table analyses with Fisher’s exact probability test, Mann–Whitney’s U test, correlation analysis, estimation of phi coefficient, binominal logistic linear regression analysis, and multivariable linear regression analysis. Statcel 3, an add-in application of Microsoft Excel, was applied to the Kruskal–Wallis test and Chi-square test. Heatmaps were produced by Python with numpy, pandas, and matplotlib.
Results
Evaluable seven hundred eighty-eight responses were extracted from collected eight hundred and one responses, excluding those of a pharmacist and twelve physicians who did not manage FN patients in their specialty.
Characteristics of the respondents associated with GL usage
A hundred and five respondents (13.3%) did not know or use GL. The average complete compliance rates (CCR) in USR and NUSR were 44.5% and 37.5% (P < 0.001), and complete plus partial compliance rates (C + PCR) were 77.5% and 64.5% (P < 0.001) by Mann–Whitney’s U test. The demographics of the respondents were analyzed with cross-tabulation table analysis with Fisher’s exact test and binomial logistic linear regression analysis (Table 2). Fisher’s exact test demonstrated that NUSR were significantly more in males, the age group of equal to or older than 50 years old (age≧50), non-members of JSMO or JSCO, and doctors who were not BCMO under 5% significant level. The male gender weakly correlated to age≧50 with a phi-coefficient of 0.252 (P < 0.001). JSMO member (including both USR and NUSR) moderately correlated to BCMO (USR + NUSR) with a phi-coefficient of 0.451 (P < 0.001).
Binomial logistic regression analysis was applied to examine the relation between the use of GL as an objective variable and the seven explanatory variables as follows: male, age≧50, PHS, JSMO and JSCO member, BCMO, and BCGCO. The result indicated that the usage was significantly lower in males with an odds ratio = 0.435 (95% confidence interval, CI: 0.230–0.823, P = 0.0105) and higher in JSCO members with an odds ratio = 1.870 (95%CI: 1.180–2.990, P = 0.00834) when removed impacts of potentially confounding roles of the other six variables. There was no correlation between the two parameters, with a phi-coefficient of 0.0546 (P = 0.125).
The frequency of USR over 50 years old were 83.2% (242/291) in men and 87.1% (27/31) in women (P = 0.799, Fisher’s exact test) and under 50 were 86.6% (279/322) and 93.8% (135/144) (P = 0.0256, Fisher’s exact test), respectively. Percentages of USR in academic societies were as follows: JSMO 88.8%, JSCO 89.7%, JSCC 90.5%, JSH 88.3%, JBA 85.0%, and those were not significantly different (P = 0.31, Fisher’s exact test).
Status of compliance with GL’s recommendations
We analyzed compliance status in six hundred eighty-three USR with the Mann–Whitney’s U test, Kruskal–Wallis test, and multivariable linear regression analysis. When compared characteristics in an attribute with a significant level of 5%, CCR was significantly higher in age < 50, PHS, ONC, JSMO members, and BCMO. C + PCR was significantly higher in females, PHS, JSMO members, and BCMO (Table 3). Female doctors accounted for 18.2% (77/422) and 26.8% (98/366) in PHS and SRG (P = 0.0046, Fisher’s exact test). Gender did not correlate with PHS with correlation coefficients of 0.122 (P = 0.0134). Ten pediatricians participated in the survey. Seven of them were USR. Their CCR and C + PCR were markedly low as 21.4% and 47.9%, respectively.
The multivariable analysis was applied to examine the association between CCR and C + PCR as objective variables and the seven explanatory variables of male, age≧50, PHS, members of JSMO and JSCO, BCMO, and BCGCO. CCR was significantly higher in BCMO when removed impacts of potentially confounding roles of the other six variables. And C + PCR was higher in JSMO members and BCMO and lower in males, significantly (Table 4).
JSMO member (including USR only) was moderately correlated with BCMO (USR only) with a correlation coefficient of 0.456 (P < 0.0001) and PHS with a correlation coefficient of 0.583 (P < 0.0001). Male did not correlate with JSMO member and BCMO with correlation coefficients of 0.0954 (P = 0.0126) and 0.0395 (P = 0.302).
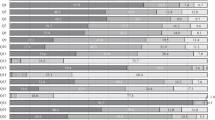
Heatmaps of the CCR and C + PCR
CCR and C + PCR of each characteristic are demonstrated in Figure as heatmaps processed from the data of the supplemental table. Differences of CCR and C + PCR between two characteristics in an attribute were analyzed with cross-tabulation table analyses with Fisher’s exact test. The results are indicated in the supplemental table. Except for the NUSR line, all the data are derived from those of USR.
Discussion
In the previous report, we demonstrated and discussed the results of question-based analysis [1]. This report discusses the results based on the respondent’s attribute and explores clues to interventions corresponding to the characteristics of each attribute. Five discussion points were extracted from the findings as follows.
Higher rates of USR and compliance in female doctors
Gender was one of the two significant influencing factors on GL usage revealed by the binomial logistic regression analysis. And it was one of the three explanatory variables extracted in the multivariable regression analysis on C + PCR. The percentage of USR and C + PCR in females was significantly higher than in males (Tables 2 and 3). The respondent consisted of 613 (77.8%) men and 175 (22.2%) women (Table 2). According to the Ministry of Health, Labor, and Welfare’s 2018 data, female doctors comprise 21.9% of the total doctors in Japan, and the ratio decreases to 13.2% only for those over 50 years old. The percentage of women among respondents and the correlation between male and age≧50 are considered reflections of the current demographic of doctors in Japan (https://www.mhlw.go.jp/toukei/saikin/hw/ishi/18/dl/kekka-1.pdf). Therefore, the results of the survey are regarded as free of methodological gender bias. It is reasonable to conclude that female doctors use and comply with GL more than male doctors.
The higher compliance rate among female doctors appears to be a common feature worldwide and across specialties compared to male doctors [4, 5]. Tsugawa Y et al. described in their report that female physicians might be more likely to adhere to guidelines. And they also referred to the better practice patterns of female physicians, including providing preventive care, using patient-centered communication, performing as well or better on standardized examinations, and providing psychosocial counseling to their patients. Besides, they reported that mortality and readmission rates for elderly hospitalized patients treated by female internists were lower than those by male internists as the results of their investigation. We could not find any description of why female doctors are more compliant with guidelines in previous investigations. It is out of reach to speculate the difference between both genders. Although it is difficult to intervene in gender-specific characteristics, the publication of these results may help change male doctors’ attitudes about GL use and compliance.
The influence of academic societies and board-certification
JSCO members were extracted as one of the two significant influencing factors on GL usage by the binomial logistic regression analysis (Table 2). JSCO members were not invited to the study directly. However, almost all of them (99.3%) belonged to at least one of the four aforementioned societies. We cannot clearly explain the association between JSCO membership and GL use, but this is probably due to the particular relation between JSCO and the other societies in this survey rather than the membership itself. JSMO members and BCMO were each identified as one of the three significant explanatory variables on C + PCR by the multivariable regression analysis (Table 4). The impact of these characteristics on C + PCR is considered smaller than gender according to the estimated regression coefficients as around 3.
The pattern of difference in compliance with each recommendation between JSMO members and non-members is almost identical to that between PHS and SRG, as discussed below (Figure and Supple Table). This is presumably due to a moderate correlation between JSMO members and PHS. The CCR for all questions except Q16 in BCMO and C + PCR were significantly higher than or equal to those in non-BCMO. In particular, C + PCR of Q2, the risk assessment for FN at the onset with MASCC score, was 64.5%, the highest among other attributes. These findings mean that BCMO is considered a reliable indicator of high GL compliance. Alternatively, BCGCO seems to have little effect on compliance.
These results may be explained by the fact that JSMO issued GL and accredits BCMO. JSMO’s educational role may function to promote evidence-based clinical practice in compliance with GL. It is necessary to send a strong message to doctors providing chemotherapy about GL compliance through not only JSMO but also other relevant academic societies. Besides, patient education on FN and infections associated with chemotherapy is an effective promotion measure, and academic societies should take the lead in this effort.
Differences in compliance rate according to specialty and subspecialty
A survey of G-CSF adherence in Germany revealed that specialty influenced doctors’ adherence to guidelines. Pulmonologists were less adherent to GL than other specialists, including hematologists-oncologists and gynecologists, though the cause was uncovered [2]. In such a case, it is assumed that there is some attribute-related barrier to compliance.
Between PHS and SRG, the overall CCR and C + PCR of PHS were higher as 45.5% vs. 43.0% (P = 0.0308) and 79.0% vs. 75.5% (P = 0.0108) (Table 3). The CCR and C + PCR of Q3-6 were significantly higher in PHS, while so were those of Q16 in SRG (Fig. 1 and Supple Table). The CCR of Q3 and 4 (strong recommendations) in PHS vs. SRG were 66.8% vs. 41.4% (P < 0.001) and 84.8% vs. 53.4% (P < 0.001). The C + PCR of Q16 (weak recommendation) in PHS vs. SRG were 54.0% and 68.3% (P < 0.001). The findings indicate that PHS places more importance on blood culture collection than SRG. SRG is more likely to emphasize the prevention of FN development than PHS. Since 78.3% of SRG were BRS, the pattern of compliance in SRG reflected BRS as mentioned below.
Heatmaps of the CCR and C + PCR for each recommendation according to the attributes and characteristics of responders. *, significantly higher than the counterpart. NUSR, non-user; USR, user; PHS, physician; SRG, surgeon; HEM, hematologist; ONC, medical oncologist; BRS, breast surgeon; NBS, surgeons other than breast surgery; JSMO, Japanese Society of Medical Oncology; BCMO, board-certified medical oncologist; BCGCO, board-certified general clinical oncologist
Between HEM and ONC, the overall CCR of HEM was lower as 41.5% vs. 47.0% (P = 0.0021) and the C + PCR was comparable as 78.0% vs. 79.0% (P = 0.2735) (Table 3). The C + PCR for Q2 and 12 (weak recommendations) were significantly lower in HEM (34.5% and 85.0% vs. 61.0% and 96.6%, both P < 0.001) (Fig. 1 and Supple Table). In hematologic malignancies, chemotherapy frequently causes severe neutropenia and immunocompromised condition with hypogammaglobulinemia. Therefore, the patients are generally at high risk when FN develops and more require intravenous gammaglobulin than in the other specialties. These are probable reasons for low compliance with Q2 and 12 in HEM, which are features of their practice and should not be seen as problems. Other HEM’s characteristics were more screening for lung tuberculosis and less vaccination for influenza. These may be related to a high prevalence of immunocompromised patients in hematologic diseases. The C + PCR of Q16 in HEM vs. ONC was 68.2% vs. 48.3% (P < 0.001). The disincentive for Q16 in ONC is considered to reflect the economic issues indicated in the free comments reported previously [1].
The overall CCR and C + PCR were markedly low in pediatricians. It was probably due to GL recommendations mainly based on the evidence of studies in adult patients.
Between BRS and NBS, the overall CCR and C + PCR were not different (Table 3). However, the patterns of compliance with each recommendation were slightly different. BRS took two sets of blood culture samples considerably less than NBS (CCR: Q3: 36.0% vs. 61.2%, P < 0.001; Q4: 48.8% vs. 70.1%, P = 0.002) (Fig. 1 and Supple Table). The CCR and C + PCR of Q15 (strong recommendation) were higher in BRS as 43.8% vs. 28.4% (P = 0.025) and 84.7% vs. 71.6% (P = 0.014). Those of Q16 were 22.3% vs. 9.0% (P = 0.014) and 73.1% vs. 50.7% (P < 0.001). In general, FN in breast cancer is as frequent and severe as other solid tumors such as lung cancer and gynecological malignancies [6, 7]. Some of the chemotherapy regimens in breast cancer are moderate to high risk for developing FN, and BRS emphasizes ppG-CSF since they treat patients’ ambulatory. Consequently, they have few opportunities to experience bloodstream infection in FN, which may have contributed to the low compliance rate with the recommendations on blood cultures.
There are reportedly seven barriers against physicians’ adherence to practice guidelines: lack of awareness, lack of familiarity, lack of agreement, lack of outcome expectancy, lack of self-efficacy, lack of motivation, and external barriers, including patient factors, guideline factors, and environmental factors [8]. These findings suggest that the specificity of specialty and subspecialty may be another barrier that should be considered when developing multidisciplinary guidelines.
Low compliance rates about collecting blood culture
The CCR and C + PCR of Q3 and 4 were significantly lower in SRG than PHS, further in BRS than NBS, as mentioned above (Fig. 1 and Suppl Table). HEM marked the highest CCR and C + PCR, which are comparable to the previous report of Kimura S et al. indicating that 92% of HEM collected two sets of blood culture at FN onset in acute myeloid leukemia [9]. The incidence of bloodstream infection in FN was 8.3–11.8% in acute myeloid leukemia and 3% in non-Hodgkin lymphoma reportedly [10,11,12]. This is the reason why HEM almost routinely takes blood cultures in FN. That in FN of solid tumors has been unknown because of very low incidence. Blood cultures are essential for diagnosing bloodstream infections, but false positives can harm patients through unnecessary antibiotics and hospitalization and cost medical resources humanly and financially. Considering those matters, BRS may dare not to take blood cultures in low-risk FN patients. Previous studies have demonstrated that an algorithm to reduce the overuse of blood cultures effectively prevents unnecessary blood cultures [13, 14]. In the algorithm, immunocompromised patients were excluded. However, if the pretest probability is sufficiently low, it may be safely omitted even in patients receiving chemotherapy. Whether it is possible to skip the collection of blood cultures from low-risk FN patients is an emerging issue that should be investigated.
Recommendations with no different compliance between USR and NUSR
We noted the difference in compliance between USR and NUSR. C + PCR was significantly higher in USR in twelve recommendations (Fig. 1 and Supple Table). It is considered fairly reasonable. However, the remaining eight recommendations, Q8, 10–14, 17, and 18, had no difference in compliance between them. The reasons are probably at least one of the following: (1) a recommendation is challenging or controversial to implement in clinical practice or requires a change in the inertia of conventional practice, (2) a recommendation should or should not be implemented as a matter of course regardless of GL, or (3) a recommendation is highly discretionary to doctors due to ambiguous and non-specific expression. Q11 falls into the first category. GL weakly recommends not to use therapeutic G-CSF but suggests using it in case of expecting deterioration. A meta-analysis has demonstrated that therapeutic G-CSF does not improve survival but shortens the duration of neutropenia and makes faster recovery from fever [15]. Therefore, it is acceptable for doctors to use therapeutic G-CSF in FN patients as long as it does not harm them. The barriers to compliance are probably due to the conflicting content and the ambiguous standard of decision-making [8]. Q18 falls into the second category. The screening of hepatitis B virus (HBV) makers is an essential examination to prevent de novo hepatitis B that potentially progresses to fatal fulminant hepatitis [16]. Overlooking it may cause the doctor to be sued. That is the driving force to adhere to the recommendation at the C + PCR of 99.0% and 97.1% for USR and NUSR. Q12–14 and 17 are also allocated to the second category. Except for Q13, they commonly recommend not doing something that is considered of little benefit. Q8 and 10 fall into the third category. Considering the low compliance rate of risk assessment of FN by the MASCC score (Q2), the ambulatory treatment of FN patients is considered at doctors’ discretion rather than based on the GL. About Q10, although GL weakly recommends continuing the initial therapy in stable and persistent FN, the definition of “stable” is unclear. And we sometimes experience a rapid aggravation of a stable FN patient to fatal illness. Whether implementing or not those recommendations is likely to be left to the doctor’s discretion. The influence of those recommendations on doctors’ clinical practice may have been limited.
Grol R et al. reported lower compliance rates in the recommendations that were vague and non-specific or that demanded a change in the existing practice routine [17, 18]. Recommendations need to be as free as possible from ambiguous and non-specific expressions or expressions that allow for great discretion by the attending physician.
This study clarified the difference in compliance among attributes and the characteristics of recommendations that affected compliance. These results may provide useful suggestions for revising GL. This study is expected to help other researchers develop and evaluate guidelines. Meanwhile, questionnaires are quick, labor-saving, low-cost, and can be applied for many recommendations at once, though their accuracy varies. Therefore, these results could deviate from the actual practices.
Data availability
Not applicable.
Code availability
The R and Python codes used in this study were not created specifically for this study but were those commonly used for statistical analysis. Therefore, there is nothing, in particular, that should be deposited as code.
References
Akiyama N, Okamura T, Yoshida M, et al (2021) A questionnaire survey on evaluation for prevention and compliance of the Japanese Guidelines on Febrile Neutropenia among hematology-oncology physicians and surgeons. Support Care Cancer 29: 6831-6839. https://doi.org/10.1007/s00520-021-06277-8.
Link H, Kerkmann M, Holtmann L et al (2011) G-CSF guideline adherence in Germany an update with a retrospective and representative sample survey. Support Care in Cancer 27:1459–1469. https://doi.org/10.1007/s00520-018-4481-x
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Tsugawa Y, Jena AB, Figueroa JF et al (2017) Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs. female physicians. JAMA Intern Med 177:206–213. https://doi.org/10.1001/jamainternmed.2016.7875
Baumhäkel M, Müller U, Böhm M (2009) Influence of gender of physicians and patients on guideline-recommended treatment of chronic heart failure in a cross-sectional study. Eur J Heart Fail 11:299–303. https://doi.org/10.1093/eurjhf/hfn041
Aapro MS, Bohlius J, Cameron DA et al (2011) 2010 update of EORTC guidelines for the use of granulocyte-colony stimulating factor to reduce the incidence of chemotherapy-induced febrile neutropenia in adult patients with lymphoproliferative disorders and solid tumours. Eur J Cancer 47:8–32. https://doi.org/10.1016/j.ejca.20110.10.013
NCCN Guidelines Hematopoietic Growth Factors. Version 4.20211-May 20, 2021. https://www.nccn.org/professionals/physician_gls/pdf/growthfactors.pdf.
Cabana MD, Rand SC, Powe NR et al (1999) Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 282:1458–1465. https://doi.org/10.1001/jama.282.15.1458
Kimura S, Fujita H, Handa H et al (2020) Real-world management of infection during chemotherapy for acute leukemia in Japan: from the results of a nationwide questionnaire-based survey by the Japan Adult Leukemia Study Group. Int J Hematol 112:409–417. https://doi.org/10.1007/s12185-020-02921-x
Kato H, Fujita H, Akiyama N et al (2018) Infectious complications in adults undergoing intensive chemotherapy for acute myeloid leukemia in 2001–2005 using the Japan Adult Leukemia Study Group AML201 protocols. Support Care Cancer 26:4187–4198. https://doi.org/10.1007/s00520-018-4292-0
Yoshida M, Akiyama N, Fujita H et al (2011) Analysis of bacteremia/fungemia and pneumonia accompanying acute myelogenous leukemia from 1987 to 2001 in the Japan Adult Leukemia Study Group. Int J Hematol 93:66–73. https://doi.org/10.1007/s12185-010-0746-y
Rummel MJ, Niederle N, Maschmyer G et al (2013) Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: an open-label, multicentre, randomized, phase3 non-inferiority trial. Lancet 381:1203–1210. https://doi.org/10.1016/S0140-6736(12)61763-2
Pawlowicz A, Holland C, Zou B et al (2015) Implementation of an evidence-based algorithm reduces blood culture overuse in an adult emergency department. Gen Int Med Clin Innnov 1:20–25. https://doi.org/10.15761/GIMCI.1000108
Shapiro NI, Wolfe RE, Wright SB et al (2008) (2008) Who needs a blood culture? A prospectively derived and validated prediction rule. J Emerg Med 35:255–264. https://doi.org/10.1016/j.jemermed.2008.04.001
Mhaskar R, Clark OAC, Lyman G, et al (2014) Colony-stimulating factors for chemotherapy-induced febrile neutropenia. Cochrane Database Syst Rev. 2014:CD003039. https://doi.org/10.1002/14651858.CD003039.pub2.
Lubel JS, Angus PW (2010) Hepatitis B reactivation in patients receiving cytotoxic chemotherapy: diagnosis and management. J Gastroenterol Hepatol 25:864–871. https://doi.org/10.1111/j.1440-1746.2010.06243.x
Barth JH, Misra S, Aakre KM et al (2016) (2016) Why are clinical practice guidelines not followed? Clin Chem Lab Med 54:1133–1139. https://doi.org/10.1515/cclm-2015-0871
Grol R, Dalhuijsen J, Thomas S et al (1998) Attributes of clinical guidelines that influence use of guidelines in general practice: observational study. Brit Med J 317:858–861. https://doi.org/10.1136/bmj.317.7162.858
Acknowledgements
The authors sincerely appreciated the physicians and surgeons who voluntarily responded to the questionnaire.
Funding
This study was supported by the Health, Labor and Welfare Sciences Research Grants. Program Grant Number: 21EA1006.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception, design of the study, revising the draft.
Chief of the study (Coordination, funding, and data collection): Sadamoto Zenda.
Principal investigator (analysis, interpretation, and drafting): Nobu Akiyama.
Drafting the manuscript: Nobu Akiyama, Takuho Okamura, and Minoru Yoshida, Shun-ichi Kimura.
Supervisor (conception and design): Kazuo Tamura.
Corresponding author
Ethics declarations
Ethics approval
This study is not required to be reviewed by an ethical committee because it is designed as a questionnaire to doctors about the daily clinical practice on GL, and respondents voluntarily answered the questions on the website.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Akiyama, N., Okamura, T., Yoshida, M. et al. Difference of compliance rates for the recommendations in Japanese Guideline on Febrile Neutropenia according to respondents’ attributes: the second report on a questionnaire survey among hematology-oncology physicians and surgeons. Support Care Cancer 30, 4327–4336 (2022). https://doi.org/10.1007/s00520-022-06834-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-06834-9