Abstract
Objective
Two-third of colorectal cancer (CRC) survivors are overweight or obese. Psychological distress and low health-related quality of life (HRQoL) may be barriers to improving diet. We aimed to assess associations between psychological distress and HRQoL and the need for dietary support in CRC survivors with overweight or obesity.
Methods
All alive individuals diagnosed with CRC between 2000 and 2009, as registered by the Dutch population-based Eindhoven Cancer Registry, were eligible for participation and received a questionnaire. Multivariable logistic regression analyses were conducted to assess associations between HRQoL (EORTC QLQ-C30), symptoms of anxiety and depression (HADS), and self-reported need for dietary support (single-item).
Results
A total of 1458 completed the questionnaire (response rate 82%), and 756 (43%) had a BMI of 25.0 or higher and complete data on “need for dietary support” and were included for analyses. BMI ranged between 25.0 and 60.6 (mean, 28.9; SD, 3.6). The majority (71.7%) was overweight (BMI ≥ 25), and 28.3% obese (BMI ≥ 30). Twenty-one percent reported a need for dietary support which was associated with more psychological distress and lower HRQoL. Those who experienced symptoms of anxiety or depression were more likely to report a need for dietary support (27.6% and 28.7%) than those who did not experience symptoms of anxiety (12.3%; OR 2.02; 95% CI 1.22–3.35) or depression (13.5%; OR 1.96; 95% CI 1.19–3.22).
Conclusions
Results suggest that psychological distress and lower HRQoL should be taken into account while promoting a healthy diet in overweight or obese CRC survivors since these factors may hinder adherence to a healthy diet.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Colorectal cancer (CRC) survivors are recommended to meet lifestyle (i.e., dietary, physical activity [5]) and body weight recommendations to improve both short- and long-term health outcomes [24]. However, research has shown that lifestyle and body weight are suboptimal in CRC survivors [29, 37]. For example, observational studies have shown that about two-thirds of CRC survivors does not meet the recommendation on body fatness [29, 35, 37]. Since body fatness is a well-established independent risk factor for the development of CRC [18, 23], a large proportion of CRC survivors are overweight or obese at the time of diagnosis.
For individuals with overweight or obesity, receiving information or advice is typically not sufficient to be able to improve lifestyle and to maintain these improvements [11]. This implies a need for additional behavioral counseling aimed at self-regulation of lifestyle behavior to be able to adhere to lifestyle advice, rather than provision of lifestyle advice alone. For CRC survivors, receiving such support to be able to eat healthier (i.e., dietary support) is particularly relevant, due to the favorable effects dietary changes may have on frequently reported bowel complaints related to CRC and its treatment, such as diarrhea, increased stool frequency, incontinence, and intolerance of certain foods [9]. Previous research has shown that CRC survivors with overweight and obesity are more likely to report a need for dietary support to be able to eat healthier than those with a body mass index in the normal range [13]. However, dietary support is currently not routinely provided during follow-up care for CRC survivors with overweight and obesity [36].
Dietary support should be offered to CRC survivors with overweight or obesity, as health benefits may be achieved by sustained lifestyle changes in this specific target group in which multiple individual risk factors for morbidity and mortality co-occur. CRC [8], overweight, and obesity [7] have individually been related to an increased risk of diabetes mellitus type 2 [16], cardiovascular diseases [38], (second) primary cancers [20], and/or mortality [38]. A reduction of these risks may be achieved with lifestyle (including dietary) support leading to favorable changes in body weight and diet quality [14].
Dietary support for CRC survivors with overweight or obesity should incorporate support in dealing with CRC-related barriers to achieve and maintain dietary changes [25], including disease and treatment-related complaints [2, 13], such as psychological distress. Psychological distress is common in CRC survivors [19, 22] and in individuals with overweight or obesity [17], and has been associated with an unhealthier lifestyle [6, 31, 32] and a poorer health-related quality of life (HRQoL) in CRC survivors [15, 19]. In addition, HRQoL has been negatively associated with meeting lifestyle and body weight recommendations in CRC survivors [3, 12, 35]. Nevertheless, psychological distress and HRQoL are not commonly taken into account while promoting a healthy lifestyle in CRC survivors with overweight or obesity.
More insight into psychological distress and HRQoL among overweight or obese CRC survivors who report a need for dietary support will inform those providing dietary support in this particular target population about aspects that should be taken into account or incorporated while providing dietary support. Therefore, this study aimed to assess associations between the psychological distress and HRQoL and the need for dietary support in CRC survivors with overweight or obesity. Our hypothesis is that a higher level of psychological distress and a lower HRQoL is associated with a higher need for dietary support in CRC survivors with overweight or obesity.
Methods
Study design
To answer our research question, we used cross-sectional data from a larger, population-based prospective observational study, with yearly surveys in Dutch CRC survivors. Details on this longitudinal study can be found elsewhere [4]. The longitudinal study was approved by a Dutch Medical Ethical Committee.
Study population and setting
All patients diagnosed with CRC from January 2000 to June 2009 were sampled from the southern area of the Netherlands Cancer Registry (NCR). The NCR includes clinical data on all newly diagnosed cancer patients in the Netherlands. Patients with cognitive impairments, unverifiable addresses, and patients who died before the start of the study were excluded.
Patient Reported Outcomes Following Initial Treatment and Long term Evaluation of Survivorship (PROFILES) registry was used for data collection management (https://www.profilesregistry.nl) [33]. Using the PROFILES registry, data on patient-reported outcomes was collected via online or paper questionnaires and linked to clinical data from the NCR.
Data collection
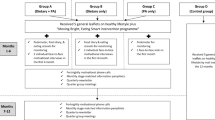
The study was set up in December 2010. The present study was performed with data collected in December 2012 as part of the third survey from this longitudinal study, which included an item on the need for dietary support. A total of 1774 eligible CRC patients were then invited for participation via a letter from their (ex-) attending specialist (Fig. 1) and were asked to complete a questionnaire. After 2 weeks, a reminder was sent. All participants provided written informed consent.
Flowchart of study participants. For this study, cross-sectional data from a larger longitudinal study among colorectal cancer survivors was used. A flowchart of the participants in the longitudinal study has been published elsewhere [4]. This current study involves data obtained from survey 3 in December 2012
Outcome measures
Need for dietary support
A single item was used to assess the need for dietary support. Participants were asked whether they agreed or disagreed with the statement “I feel the need for support to be able to eat healthier.”
Sociodemographic, cancer-, and health-related characteristics
Date of birth, sex, and clinical information including date of cancer diagnosis, tumor stage at diagnosis, tumor site, and primary cancer treatment were obtained from the NCR. Socio-economic status (SES) was based on fiscal data on the national economic value of residences and household income aggregated per postal code [34], and categorized into three categories: low, middle, and high. Data on marital status and received follow-up care after treatment at the time of the survey were self-reported using single survey items. “Having diabetes at the moment of the survey or during the 12 months before” (yes/ no) was measured with the adjusted Self-Administered Comorbidity Questionnaire (SCQ) [26]. Having a stoma was assessed by an item from the CRC-specific module of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-CR38) [30]. Self-reported body height (cm) and weight (kg) were used to calculate body mass index (BMI). BMI was categorized as underweight (BMI < 18.5 kg/m2), normal weight (18.5 ≤ BMI < 25 kg/m2), overweight (25 ≤ BMI < 30 kg/m2), or obesity (BMI ≥ 30 kg/m2).
Health-related quality of life
HRQoL was measured using the global quality of life scale and the five functional scales of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ-C30) version 3.0 [1]. The global quality of life scale consists of two items on a 7-point Likert scale, ranging from 1 = “Very bad” to 7 = “Excellent.” The five functional scales consist of items on a 4-point Likert scale, ranging from “Not at all” to “Very much”: physical functioning (5 items), role functioning (2 items), emotional functioning (4 items), cognitive functioning (2 items), and social functioning (2 items). For each scale, the RawScore was composed by calculating the mean of the scale items. According to the scoring manual, scores were transformed to a linear scale ranging from 0 to 100, with higher scores indicating better global quality of life and functioning [10].
Psychological distress
Psychological distress was assessed using the Hospital Anxiety and Depression Scale (HADS) [39]. The HADS consists of 14 items assessing self-reported symptoms of anxiety (7 items) and depression (7 items) in the past week. Each item is scored on a 4-point Likert scale, ranging from 0 to 3. A total score can be calculated for both symptoms of anxiety and symptoms of depression by adding up the scores on the 7 items. These total scores range from 0 to 21, with higher scores indicating more symptoms. A cut-off score of 8 or higher is used to indicate having symptoms of depression or anxiety [39].
Statistical analyses
Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 20. Differences in sociodemographic and clinical characteristics between those included in the population for analyses and those excluded were assessed using independent Student’s t tests for continuous variables and Chi-square tests for categorical variables. Since the variable age at the time of survey completion was not normally distributed, this variable was incorporated in the statistical analyses as a categorical variable. Age was categorized into the following categories based on the observed data distribution: 31–64, 65–69, 70–76, 77–87.
Mean (with standard deviations (SD)) and frequency tables were used to describe sociodemographic, cancer-related, and health-related characteristics. Frequency tables were used to describe psychological distress and cancer-specific HRQoL. Since cancer-specific HRQoL-scores were not normally distributed, scores on global QoL and functional scales were divided into categories for the statistical analyses based on EORTC QLQ-CR30 reference values [28]: “below average” (score between 0 and 66.6), “average” (score between 66.7 and 74.9), “above average” (score between 75.0 and 99.9), and “high” (score of 100).
Univariable logistic regression analyses were conducted, with the need for dietary support (yes/no) as dependent variable and one sociodemographic, cancer-related, or health-related characteristic as independent variable (see Table 1).
Logistic regression analyses were conducted to examine associations between HRQoL, psychological distress, and the need for dietary support. Univariable logistic regression analyses were conducted with need for support as dependent variable and a single HRQOL variable or psychological distress variable as independent variable. Multivariable logistic regression analyses were conducted with need for support as dependent variable, and as independent variables one cancer-specific HRQoL variable or psychological distress variable and all sociodemographic, cancer-related, and health-related characteristics that were found to be statistically significantly associated with the need for support in the univariable logistic regression analyses (age, sex, having a partner, having diabetes, degree of overweight) (see Table 2).
Results
Of the 1774 CRC survivors who were invited for participation, 1458 completed the questionnaire (response rate 82%), and 756 (43%) had a BMI of 25.0 or higher and complete data on “need for dietary support” and were included for analyses (Fig. 1). Compared to those included for analyses, those who were excluded were older (mean age 70.9, SD 9.5 vs. mean age 68.8, SD 9.4; p < 0.001), more often female (50.6 vs. 32.9%; p < 0.001), more often diagnosed with colon cancer (62.7 vs. 56.9%; p = 0.014), more often diagnosed at an earlier tumor stage (stage I 31.3%, stage II 38.5% vs. stage I 30.0% and stage II 34.1%; p = 0.038), and less often underwent chemotherapy (27.6 vs. 33.3%, p = 0.009). Those excluded did not differ from those included with regard to socio-economic status and time since diagnosis.
Age of CRC survivors in the population for analyses ranged from 35 to 87 years, with a mean age of 68.8 (SD 9.4) (Table 1). Most were male (67.1%) and living with a partner (79.8%). Time since diagnosis varied from 3 to 13 years (mean 6.8 years; SD 2.7). BMI ranged between 25.0 and 60.6 (mean 28.9; SD 3.6). The majority (71.7%) was classified as overweight (BMI ≥ 25) and 28.3% as obese (BMI ≥ 30).
Need for dietary support
A need for dietary support was reported by 21.2% (n = 160). Compared with those without a need for dietary support, CRC survivors who reported a need for dietary support were younger (mean age 66.5, SD = 10.6 vs. mean age 69.4, SD = 8.9), more often female (41.2 vs. 30.7%), less often had a partner (72.2 vs. 82.2%), more often had diabetes (28.8 vs. 16.9%), and were more often classified as obese (40.6 vs. 25.0%) (all p < 0.05; Table 1).
Health-related quality of life
All HRQoL domains were significantly associated with the need for dietary support. Univariable and multivariable logistic regression analyses showed comparable results and are discussed below (Table 2). A total of 69.7% of overweight and obese CRC survivors had either high (15.4%) or above average (54.3%) global QoL scores. Similarly, the majority of them had either high or above average scores across functional scales. The largest majorities of high and above average scores were observed in the emotional functioning (82.4%), the social functioning (77.0%), and the cognitive functioning (76.2%) scales.
Global quality of life
A total of 15.1% had a global QoL score below average. CRC survivors who reported a need for dietary support more often had a global QoL score below average (26.8%) than CRC survivors without a need for dietary support (12.1%). Compared with those with a global QoL score below average, those with a high global QoL score and those with a global QoL score above average were less likely to report a need for dietary support (high OR 0.42; 95% CI 0.20–0.88; above average OR 0.50; 95% CI 0.29–0.86; Table 2).
Functional scales
Among the functional scales, the largest proportions of below average scores were observed in the physical functioning (18.0%) and the role functioning (16.7%) scales. All functional scales were statistically significantly associated with the need for dietary support (Table 2).
CRC survivors who reported a need for dietary support more often had a physical functioning score below average (28.5%) than CRC survivors without a need for dietary support (15.2%). Compared with those with a physical functioning score below average, those with a high physical functioning score and those with a physical functioning score above average were less likely to report a need for dietary support (high OR 0.39; 95% CI 0.20–0.76; above average OR 0.54; 95% CI 0.31–0.94).
CRC survivors who reported a need for dietary support more often had a role functioning score below average (25.3%) than CRC survivors without a need for dietary support (14.4%). Compared with those with a role functioning score below average, those with a high role functioning score were less likely to report a need for dietary support (OR 0.51; 95% CI 0.29–0.88).
Psychological distress
Psychological distress was significantly associated with the need for dietary support. Univariable and multivariable logistic regression analyses showed comparable results (Table 2). Symptoms of anxiety were reported by 15.5% of CRC survivors. Those who experienced symptoms of anxiety were more likely to report a need for dietary support (27.6%) than those who did not experience symptoms of anxiety (12.3%; OR 2.02; 95% CI 1.22–3.35).
Symptoms of depression were reported by 16.7%. Participants with symptoms of depression were more likely to report a need for dietary support (28.7%) compared with those without symptoms of depression (13.5%; OR 1.96; 95% CI 1.19–3.22).
Discussion
To the best of our knowledge, this is the first study on the associations of psychological distress and HRQoL with the need for dietary support among CRC survivors with overweight or obesity. We observed that those with symptoms of anxiety and depression and a lower HRQoL (all domains) were more likely to report a need for dietary support compared to those without a need for dietary support.
Previous research on psychological health and lifestyle behavior among CRC survivors has shown an association between higher psychological distress and an unhealthier lifestyle [6, 31, 32]. Trudel-Fitzgerald et al. [31] found that among women with CRC from the Nurses’ Health Study prospective cohort in the USA, higher levels of anxiety and depression symptoms were associated with subsequent unhealthier lifestyle in the 10 years following CRC diagnosis [31]. Although, to our knowledge, no other study has specifically assessed the association between psychological distress and diet quality among CRC survivors, two studies have assessed the association between psychological distress and physical (in)activity in CRC survivors [6, 32]. In a prospective survey among Australian CRC survivors, it was found that those who experienced anxiety were at greater risk of physical inactivity. In addition, CRC survivors with higher levels of initial anxiety were less likely to increase their levels of self-reported physical activity at subsequent time points, whereas depression was not found to be related to increases in physical activity [6]. Similarly, a population-based cross-sectional study in Canadian and Western Australian colon cancer survivors showed that higher levels of accelerometer-assessed moderate-to-vigorous intensity physical activity were associated with lower levels of anxiety, but not with symptoms of depression [32].
Previous studies on the association between HRQoL and lifestyle in CRC survivors found that a higher HRQOL was associated with favorable lifestyle or meeting lifestyle recommendations [3, 12, 27, 35], and suggest a positive association between a higher HRQoL and the number of lifestyle recommendations that are being met. Associations seem to be strongest between physical activity and physical HRQoL domain scores (e.g., physical functioning) [27]. Few studies have specifically examined the association between HRQoL and adherence to dietary recommendations or diet quality among CRC survivors [7, 9, 18, 27]. Whereas Grimmett et al. [12] found that a higher global QoL and physical, role, and cognitive function was associated with fruit and vegetable intake in CRC survivors [9, 35, 36] found that HRQoL and HRQoL domains were not associated with adherence to the dietary recommendations shortly after diagnosis [7]. Both studies did not assess the need for dietary support.
Limitations and strengths
Several limitations need to be taken into account while interpreting our findings. First, the underrepresentation of stage IV CRC survivors observed in our study sample limits the generalizability of our findings to CRC survivors diagnosed at stage IV. Second, due to a lack of power, we were unable to include both psychological distress variables and HRQoL domains in the multivariable logistic regression analyses [21], while ideally we would have included these variables since previous research has shown an association between psychological distress and HRQoL in CRC survivors [15, 19]. Third, the need for dietary support was assessed with a single item which could have been less clear for patients and resulted in less nuanced results compared to the assessment of needs with a scale or questionnaire. Also, one should remember that the expression of a need for dietary support does not automatically mean poor adherence to dietary guidelines. It should be noted that our findings may have possibly been influenced by selection bias. Those included in our study sample were less often female compared with those excluded from our study sample while our findings show that females were more likely to report a need for dietary support. Thus, there may have been an underestimation of the proportion of those in need for dietary support in our study sample. On the other hand, the proportion of those in need for support may have been overestimated since those included in our study sample were younger compared with those excluded while our findings show that being younger was associated with a need for dietary support.
Also, the cross-sectional nature of this study limits the determination of causal associations. Finally, although we did not observe an association between time since diagnosis and the perceived need for dietary support to be able to eat healthier in our study among survivors varying in time since diagnosis (range 3 to 13 years), the need for dietary support most likely will vary over time for the individual CRC survivor, as will perceived levels of psychological distress. Future longitudinal observational studies could provide valuable information on fluctuations over time and individual differences in the need for support, psychological distress, and HRQoL which can inform decisions on when to provide what type of dietary and/or psychological support.
Strengths of this study that are worth mentioning include the relatively large population-based study sample with a high response rate, obtained via the well-established PROFILES registry [33], and the use of standardized, validated, commonly used questionnaires to assess psychological distress and HRQoL [1, 39].
Implications
Our finding that higher psychological distress and a lower HRQoL were associated with the need for dietary support suggests that these factors, which may hinder adherence to a healthy diet, should be taken into account while promoting a healthy diet in overweight or obese CRC survivors. Ideally, multidisciplinary support should be offered to CRC survivors with overweight and obesity, using a more holistic approach than currently is applied in clinical oncological care, to promote a healthy lifestyle and physical and psychological health.
Conclusion
This study showed that psychological distress and a lower HRQoL across all domains were associated with the need for dietary support in CRC survivors with overweight or obesity. Results suggest that perceived psychological and physical health should be taken into account while promoting a healthy diet in overweight or obese CRC survivors since these factors may hinder adherence to a healthy diet.
Data availability
Data from the PROFILES registry are freely available for non-commercial scientific research, subject to submission of a study question, privacy and confidentiality restrictions, and registration (www.profilesregistry.nl).
References
Aaronson NK, Ahmedzai S, Bergman B et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Anderson AS, Steele R, Coyle J (2013) Lifestyle issues for colorectal cancer survivors–perceived needs, beliefs and opportunities. Support Care Cancer 21(1):35–42
Blanchard CM, Courneya KS, Stein K (2008) Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. J Clin Oncol 26(13):2198–2204
Bours MJ, Beijer S, Winkels RM, van Duijnhoven FJ, Mols F, Breedveld-Peters JJ et al (2015) Dietary changes and dietary supplement use, and underlying motives for these habits reported by colorectal cancer survivors of the Patient Reported Outcomes Following Initial Treatment and Long-Term Evaluation of Survivorship (PROFILES) registry. Br J Nutr 114(2):286–296
Buffart LM, Galvao DA, Brug J et al (2014) Evidence-based physical activity guidelines for cancer survivors: current guidelines, knowledge gaps and future research directions. Cancer Treat Rev 40(2):327–340
Chambers SK, Lynch BM, Aitken J et al (2009) Relationship over time between psychological distress and physical activity in colorectal cancer survivors. J Clin Oncol 27(10):1600–1606
Collaborators GBDO, Afshin A, Forouzanfar MH et al (2017) Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 377(1):13–27
De Marco MF, Janssen-Heijnen ML, van der Heijden LH et al (2000) Comorbidity and colorectal cancer according to subsite and stage: a population-based study. Eur J Cancer 36(1):95–99
Denlinger CS, Barsevick AM (2009) The challenges of colorectal cancer survivorship. J Natl Compr Canc Netw 7(8): 883–893; quiz 894
Fayers PM, Aaronson NK, Bjordal K et al (2001) The EORTC QLQC30 Scoring Manual. Reportno. Report Number|, Date. Place Published|: Institution|
Franz MJ, VanWormer JJ, Crain AL et al (2007) Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc 107(10):1755–1767
Grimmett C, Bridgewater J, Steptoe A et al (2011) Lifestyle and quality of life in colorectal cancer survivors. Qual Life Res 20(8):1237–1245
Hoedjes M, de Kruif A, Mols F et al (2017) An exploration of needs and preferences for dietary support in colorectal cancer survivors: a mixed-methods study. PLoS ONE 12(12):e0189178
Hoedjes M, van Stralen MM, Joe STA et al (2017) Toward the optimal strategy for sustained weight loss in overweight cancer survivors: a systematic review of the literature. J Cancer Surviv 11(3):360–385
Jansen L, Herrmann A, Stegmaier C et al (2011) Health-related quality of life during the 10 years after diagnosis of colorectal cancer: a population-based study. J Clin Oncol 29(24):3263–3269
Khaledi M, Haghighatdoost F, Feizi A et al (2019) The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. https://doi.org/10.1007/s00592-019-01295-9
Mannan M, Mamun A, Doi S et al (2016) Is there a bi-directional relationship between depression and obesity among adult men and women? Systematic review and bias-adjusted meta analysis. Asian J Psychiatr 21:51–66
McMichael AJ (2008) Food, nutrition, physical activity and cancer prevention. Authoritative report from World Cancer Research Fund provides global update. Public Health Nutr 11(7):762–763
Mols F, Schoormans D, de Hingh I et al (2018) Symptoms of anxiety and depression among colorectal cancer survivors from the population-based, longitudinal PROFILES Registry: Prevalence, predictors, and impact on quality of life. Cancer 124(12):2621–2628
Ng AK, Travis LB (2008) Second primary cancers: an overview. Hematol Oncol Clin North Am 22(2): 271–289, vii
Peduzzi P, Concato J, Kemper E et al (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379
Peng YN, Huang ML, Kao CH (2019) Prevalence of depression and anxiety in colorectal cancer patients: a literature review. Int J Environ Res Public Health 16(3)
Renehan AG, Tyson M, Egger M et al (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371(9612):569–578
Research WCRFAIfC (2018) Diet, nutrition, physical activity and cancer: a global perspective. Reportno. Report Number|, Date. Place Published|: Institution|
Rock CL, Doyle C, Demark-Wahnefried W et al (2012) Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. https://doi.org/10.3322/caac.21142
Sangha O, Stucki G, Liang MH et al (2003) The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum 49(2):156–163
Schlesinger S, Walter J, Hampe J et al (2014) Lifestyle factors and health-related quality of life in colorectal cancer survivors. Cancer Causes Control 25(1):99–110
Scott NW, Fayers PM, Aaronson NK et al (2008) EORTC QLQ-C30 reference values. Reportno. Report Number|, Date. Place Published|: Institution|
Soerjomataram I, Thong MS, Korfage IJ et al (2012) Excess weight among colorectal cancer survivors: target for intervention. J Gastroenterol. https://doi.org/10.1007/s00535-012-0567-2
Sprangers MA, te Velde A, Aaronson NK (1999) The construction and testing of the EORTC colorectal cancer-specific quality of life questionnaire module (QLQ-CR38). European Organization for Research and Treatment of Cancer Study Group on Quality of Life. Eur J Cancer 35(2):238–247
Trudel-Fitzgerald C, Tworoger SS, Poole EM et al (2018) Psychological symptoms and subsequent healthy lifestyle after a colorectal cancer diagnosis. Health Psychol 37(3):207–217
Vallance JK, Boyle T, Courneya KS et al (2015) Accelerometer-assessed physical activity and sedentary time among colon cancer survivors: associations with psychological health outcomes. J Cancer Surviv 9(3):404–411
van de Poll-Franse LV, Horevoorts N, van Eenbergen M et al (2011) The Patient Reported Outcomes Following Initial treatment and Long term Evaluation of Survivorship registry: scope, rationale and design of an infrastructure for the study of physical and psychosocial outcomes in cancer survivorship cohorts. Eur J Cancer 47(14):2188–2194
van Duijn C, Keij I (2002) Sociaal-economische status indicator op postcode niveau (Socioeconomic status indicator on zip code level). Maandstatistiek van de bevolking 50:32–35
van Veen MR, Mols F, Bours MJL et al (2019a) Adherence to the World Cancer Research Fund/American Institute for Cancer Research recommendations for cancer prevention is associated with better health-related quality of life among long-term colorectal cancer survivors: results of the PROFILES registry. Support Care Cancer. https://doi.org/10.1007/s00520-019-04735-y
van Veen MR, Mols F, Smeets L et al (2019b) Colorectal cancer survivors’ beliefs on nutrition and cancer; correlates with nutritional information provision. Support Care Cancer. https://doi.org/10.1007/s00520-019-04934-7.
Winkels RM, van Lee L, Beijer S et al (2016) Adherence to the World Cancer Research Fund/American Institute for Cancer Research lifestyle recommendations in colorectal cancer survivors: results of the PROFILES registry. Cancer Med. https://doi.org/10.1002/cam4.791
Writing Group M, Mozaffarian D, Benjamin EJ et al (2016) Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 133(4):e38-360
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370
Funding
This publication was funded by the Dutch Cancer Society/Alpe D’HuZes (VUL 2011–5234), and was based on studies supported by the Dutch Cancer Society/Alpe D’HuZes (UM 2012–5653) and a VENI grant (#451–10-041) from the Netherlands Organization for Scientific Research, The Hague, The Netherlands.
Author information
Authors and Affiliations
Contributions
FM and SB designed the study; FM collected the data. MH and DR drafted the manuscript. All authors provided input into revisions of the manuscript and have approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Medical Ethical Research Committee of the Máxima Medical Center, Eindhoven, the Netherlands (ethics approval number 0822).
Consent to participate
All patients signed informed consent.
Consent for publication
All authors provided consent for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramp, D., Mols, F., Ezendam, N. et al. Psychological distress and lower health-related quality of life are associated with need for dietary support among colorectal cancer survivors with overweight or obesity. Support Care Cancer 29, 7659–7668 (2021). https://doi.org/10.1007/s00520-021-06306-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06306-6