Abstract
Purpose
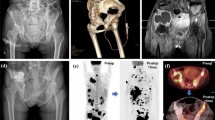
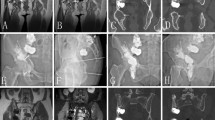
To compare the clinical efficacies of percutaneous osteoplasty (POP) and combination therapy with percutaneous osteoplasty and transcatheter arterial chemoembolization (POPTACE) for the treatment of pelvic bone metastases.
Methods
A retrospective study of 100 patients with pelvic bone metastases who had been treated by POP (n = 50) and POPTACE (n = 50) was conducted in this work. The clinical efficacies of these two treatments were evaluated by comparing their pain and functional abilities and bone metastases ability at the pre- and post-operative time points.
Results
POPTACE and POP treatments had no significant differences (P > 0.05) in VAS scores and KPS scores. Concerning tumor response, a partial response in 37 of 50 (74%) patients at 1 month for the POPTACE group and a partial response in 26 of 50 (52%) patients at 1 month for the POPC group were observed (P = 0.04). Although POPTACE and POP treatments had significant and similar ability in pain relief and functional recovery ability for the treatment of pelvic bone metastases, POPTACE treatment had a significantly better tumor response ability (partial response and stable response) compared with POP treatment.
Conclusion
Both POP and POPTACE were effective methods for the treatment of pelvic bone metastases. Moreover, these initial outcomes suggest POPTACE treatment may be better than POP treatment. POPTACE treatment has great value and is worth promoting vigorously in orthopedics clinics.





Similar content being viewed by others
References
Healey JH, Brown HK (2000) Complications of bone metastases. Cancer. 88(S12):2940–2951
Picci P, Manfrini M, Fabbri N, Gambarotti M, Vanel D (2014) Atlas of musculoskeletal tumors and tumorlike lesions. Springer Publisher, Berlin
Galibert P, Deramond H (1990) Percutaneous acrylic vertebroplasty as a treatment of vertebral angioma as well as painful and debilitating diseases. Chirurgie. 116(3):326–334
Kim Y-Y, Rhyu K-W (2010) Recompression of vertebral body after balloon kyphoplasty for osteoporotic vertebral compression fracture. Eur Spine J 19(11):1907–1912
Ee GWW, Lei J, Guo CM, Yeo W, Tan SB, Tow PBB, Chen LTJ, Yue WM (2015) Comparison of clinical outcomes and radiographic measurements in four different treatment modalities for osteoporotic compression fractures: retrospective analysis. J Spinal Disord Tech 28(6):E328–EE35
Chen C, Li D, Wang Z, Li T, Liu X, Zhong J (2016) Safety and efficacy studies of vertebroplasty, kyphoplasty, and mesh-container-plasty for the treatment of vertebral compression fractures: preliminary report. PLoS One 11(3):e0151492
Yevich S, Tselikas L, Gravel G, de Baere T, Deschamps F (2018) Percutaneous cement injection for the palliative treatment of osseous metastases: a technical review. Semin Interv Radiol 35(4):268–280
Liu X-w, Jin P, Liu K et al (2017) Comparison of percutaneous long bone cementoplasty with or without embedding a cement-filled catheter for painful long bone metastases with impending fracture. Eur Spine J 27(1):120–127
Rosenbluth PR, Grossman R, Arias B (1960) Accurate placement of artificial emboli: a problem in the treatment of cerebral angiomas by the embolization method. J Am Med Assoc 174(3):308–309
Guan Y-S, He Q, Wang M-Q (2012) Transcatheter arterial chemoembolization: history for more than 30 years. ISRN Gastroenterol 2012:8
Chiras J, Adem C, Vallée J-N, Spelle L, Cormier E, Rose M (2004) Selective intra-arterial chemoembolization of pelvic and spine bone metastases. Eur Spine J 14(10):1774–1780
Koike Y, Takizawa K, Ogawa Y, Muto A, Yoshimatsu M, Yagihashi K, Nakajima Y (2011) Transcatheter arterial chemoembolization (TACE) or embolization (TAE) for symptomatic bone metastases as a palliative treatment. Cardiovasc Interv Radiol 34(4):793–801
Fu’an W, Lifu W, Shuxiang W et al (2011) Intravascular chemoembolization combined with percutaneous vertebroplasty for the treatment of metastatic vertebral tumors: an analysis of its clinical application. J Interv Radiol 20(12):1003–1006
Tian Q-H, Shi L-N, Wu C-G, Wang J, Wang J-B, Cheng Y-S (2017) Percutaneous vertebroplasty combined with transcatheter arterial infusion/chemoembolization for the treatment of spinal metastases. Iran J Radiol 14(3):1–6
S Z-F, D G, H S-C, G J-H (2012) Treatment effect of combination interventional therapy on vertebral metastasis. Chin J Interv Imaging Ther 9(8):575–578
Chen Y, Yan Z, Wang J, Wang X, Cheng J, Gong G, Luo J (2013) Transarterial chemoembolization for pain relief in patients with hypervascular painful metastatic spinal tumors refractory to percutaneous vertebroplasty. J Cancer Res Clin Oncol 139(8):1343–1348
Müller DA, Capanna R (2015) The surgical treatment of pelvic bone metastases. Adv Orthopedics 2015:1–10
Liu H-F, Wu C-G, Tian Q-H, Wang T, Yi F (2019) Application of percutaneous osteoplasty in treating pelvic bone metastases: efficacy and safety. Cardiovasc Interv Radiol 42(12):1738–1744
Longo UG, Loppini M, Denaro L, Brandi ML, Maffulli N, Denaro V (2010) The effectiveness and safety of vertebroplasty for osteoporotic vertebral compression fractures. A double blind, prospective, randomized, controlled study. Clin Cases Miner Bone Metab 7(2):109–113
Yamada K, Matsumoto Y, Kita M, Yamamoto K, Kohda W, Kobayashi T, Takanaka T (2007) Clinical outcome of percutaneous osteoplasty for pain caused by metastatic bone tumors in the pelvis and femur. J Anesth 21(2):277–281
Sun G, Jin P, Liu X-w, Li M, Li L (2014) Cementoplasty for managing painful bone metastases outside the spine. Eur Spine J 24(3):731–737
Ren B, Wang W, Shen J, Li W, Ni C, Zhu X (2019) Transarterial chemoembolization (TACE) combined with sorafenib versus tace alone for unresectable hepatocellular carcinoma: a propensity score matching study. J Cancer 10(5):1189–1196
Bourdel N, Alves J, Pickering G, Ramilo I, Roman H, Canis M (2015) Systematic review of endometriosis pain assessment: how to choose a scale? Hum Reprod Update 21(1):136–152
Crooks V, Waller S, Smith T, Hahn TJ (1991) The use of the Karnofsky Performance Scale in determining outcomes and risk in geriatric outpatients. J Gerontol 46(4):M139–MM44
Costelloe CM, Chuang HH, Madewell JE, Ueno NT (2010) Cancer response criteria and bone metastases: RECIST 1.1, MDA and PERCIST. J Cancer 1:80–92
Galibert P, Deramond H, Rosat P, Le Gars D (1987) Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 33(2):166–168
Dong R, Chen L, Tang T, Gu Y, Luo Z, Shi Q, Li X, Zhou Q, Yang H (2013) Pain reduction following vertebroplasty and kyphoplasty. Int Orthop 37(1):83–87
Jiao S, Subudhi SK, Aparicio A et al (2019) Differences in tumor microenvironment dictate T helper lineage polarization and response to immune checkpoint therapy. Cell 179(5):1177–90.e13
Acknowledgments
The authors would like to sincerely thank the patients who participated in this feasibility study.
Funding
This research has been supported by research grants from the National Natural Science Foundation of China (81671799) and the Science and Technology Plan of Jinan Municipal Health Commission (2017-1-31).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards and were approved by the Ethics Committees of the two hospitals (ChiCTR1900022474). We have obtained consent from all the patients.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Zhang, L., Wang, B., Cao, P. et al. Combination therapy with percutaneous osteoplasty and transcatheter arterial chemoembolization for the treatment of pelvic bone metastases: preliminary report. Support Care Cancer 29, 2529–2536 (2021). https://doi.org/10.1007/s00520-020-05783-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05783-5