Abstract
Background
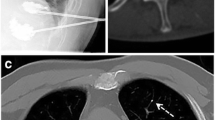
Percutaneous vertebroplasty has been a good option to treat vertebral metastases. The pelvic bone is a common site of spread for many cancers. Using follow-up data for 126 patients, we evaluated the safety and efficacy of percutaneous osteoplasty (POP) to treat pelvic bone metastases.
Materials and Methods
In this retrospective study, 126 patients (mean age 57.45 ± 11.46 years old) with 178 lesions were treated using POP. The visual analog scale (VAS), Oswestry Disability Index (ODI), and the changes in the patient’s use of painkillers were used to evaluate pain and quality of life before the procedure, and at 3 days and 1, 3, 6, 9, and 12 months after the procedure.
Results
Technical success was achieved in all patients. The mean VAS scores decreased significantly from 6.87 ± 1.33 before the procedure to 3.33 ± 1.94 by day 3 after the procedure (P < 0.05), 2.26 ± 1.59 at 1 month (P < 0.05), 1.89 ± 1.53 at 3 months (P < 0.05), 1.87 ± 1.46 at 6 months (P < 0.05), 1.90 ± 1.47 at 9 months (P < 0.05), and 1.49 ± 1.17 at 12 months (P < 0.05). The ODI also changed after the procedure, with significant differences between baseline scores and at each follow-up examination (P < 0.05). Pain relief was achieved in 118 patients (93.65%); however, pain relief was not obvious in seven patients (5.56%), and pain was aggravated in one patient (0.79%). Extraosseous cement leakage occurred in 35 patients (27.78%) without causing any clinical complications.
Conclusion
Percutaneous osteoplasty is a safe and effective choice for patients with painful osteolytic pelvic bone metastases. It can relieve pain, reduce disability, and improve function.
Level of Evidence
Level 3b, retrospective study.



Similar content being viewed by others
References
Galibert P, Deramond H, Rosat P, et al. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987;33(2):166–8.
Tian QH, Wu CG, Gu YF, et al. Combination radiofrequency ablation and percutaneous osteoplasty for palliative treatment of painful extraspinal bone metastasis: a single-center experience. J Vasc Interv Radiol JVIR. 2014;25(7):1094–100.
Tian QH, He CJ, Wu CG, et al. Comparison of percutaneous cementoplasty with and without interventional internal fixation for impending malignant pathological fracture of the proximal femur. Cardiovasc Interv Radiol. 2016;39(1):81–9.
Sun G, Jin P, Li M, et al. Percutaneous cementoplasty for painful osteolytic humeral metastases: initial experience with an innovative technique. Skelet Radiol. 2011;40(10):1345–8.
Onate Miranda M, Moser TP. A practical guide for planning pelvic bone percutaneous interventions (biopsy, tumour ablation and cementoplasty). Insights Into Imaging. 2018;9(3):275–85.
Amin RM, Micheal R, Amit J, et al. Risk factors for nonroutine discharge in adult spinal deformity surgery. Spine J. 2018;19(2):357–63.
Baek SJ, Hur H, Min BS, et al. The characteristics of bone metastasis in patients with colorectal cancer: a long-term report from a single institution. World J Surg. 2016;40(4):982–6.
Rief H, Bischof M, Bruckner T, et al. The stability of osseous metastases of the spine in lung cancer–a retrospective analysis of 338 cases. Radiat Oncol. 2013;8(1):200.
Clarencon F, Jean B, Pham HP, et al. Value of percutaneous radiofrequency ablation with or without percutaneous vertebroplasty for pain relief and functional recovery in painful bone metastases. Skelet Radiol. 2013;42(1):25–36.
Botton E, Edeline J, Rolland Y, et al. Cementoplasty for painful bone metastases: a series of 42 cases. Med Oncol. 2012;29(2):1378–83.
Laitinen MK, Parry MC, Albergo JI, et al. Is computer navigation when used in the surgery of iliosacral pelvic bone tumours safer for the patient? Bone Jt J. 2017;99-B(2):261–6.
Puget J, Utheza G. Reconstruction of the iliac bone using the homolateral femur after resection for pelvic tumor. Orthop Traumatol Surg Res. 2014;100(1):43–7.
Matcuk GR Jr, Mahanty SR, Skalski MR, et al. Stress fractures: pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol. 2016;23(4):365–75.
Chow R, Hoskin P, Hollenberg D, et al. Efficacy of single fraction conventional radiation therapy for painful uncomplicated bone metastases: a systematic review and meta-analysis. Ann Palliat Med. 2017;6(2):125–42.
Chan S, Rowbottom L, McDonald R, et al. Pelvic insufficiency fractures in women following radiation treatment: a case series. Ann Palliat Med. 2016;5(3):233–7.
Prieto-Alhambra D, Avilés FF, Judge A, et al. Burden of pelvis fracture: a population-based study of incidence, hospitalisation and mortality. Osteoporos Int. 2012;23(12):2797–803.
Trumm CG, Pahl A, Helmberger TK, et al. CT fluoroscopy-guided percutaneous vertebroplasty in spinal malignancy: technical results, PMMA leakages, and complications in 202 patients. Skelet Radiol. 2012;41(11):1391–400.
Liu XW, Jin P, Liu K, et al. Comparison of percutaneous long bone cementoplasty with or without embedding a cement-filled catheter for painful long bone metastases with impending fracture. Eur Radiol. 2017;27(1):120–7.
Clarencon F, Jean B, Pham HP, et al. Value of percutaneous radiofrequency ablation with or without percutaneous vertebroplasty for pain relief and functional recovery in painful bone metastases. Skeletal Radiol. 2013;42(1):25–36.
Botton E, Edeline J, Rolland Y, et al. Cementoplasty for painful bone metastases: a series of 42 cases. Med Oncol. 2012;29(2):1378–83.
Wei Z, Hui W, Ji-Hong H, et al. Palliative pain relief and safety of percutaneous radiofrequency ablation combined with cement injection for bone metastasis. Jpn J Clin Oncol. 2018;48(8):753–9.
Hartung MP, Tutton SM, Hohenwalter EJ, et al. Safety and efficacy of minimally invasive acetabular stabilization for periacetabular metastatic disease with thermal ablation and augmented screw fixation. J Vasc Interv Radiol. 2016;27(5):682–8.
Kang HG, Roh YW, Kim HS. The treatment of metastasis to the femoral neck using percutaneous hollow perforated screws with cement augmentation. J Bone Jt Surg Br. 2009;91(8):1078–82.
Kim JH, Kang HG, Kim JR, et al. Minimally invasive surgery of humeral metastasis using flexible nails and cement in high-risk patients with advanced cancer. Surg Oncol. 2011;20(1):e32–7.
Cho HS, Park IH, Jeon IH, et al. Direct application of MR images to computer-assisted bone tumor surgery. J Orthop Sci. 2011;16(2):190–5.
Fayad LM, Jacobs MA, Wang X, et al. Musculoskeletal tumors: how to use anatomic, functional, and metabolic MR techniques. Radiology. 2012;265(2):340–56.
Kim YJ, Lee JW, Kim KJ, et al. Percutaneous vertebroplasty for intravertebral cleft: analysis of therapeutic effects and outcome predictors. Skeletal Radiol. 2010;39(8):757–66.
Burgard CA, Dinkel J, Strobl F, et al. CT fluoroscopy-guided percutaneous osteoplasty with or without radiofrequency ablation in the treatment of painful extraspinal and spinal bone metastases: technical outcome and complications in 29 patients. Diagn Interv Radiol. 2018;24:158–65.
Lee JH, Kim SY, Ok HG, et al. Extraspinal percutaneous osteoplasty for the treatment of painful bony metastasis. J Kor Med Sci. 2018;33:61.
Wallace AN, Huang AJ, Vaswani D, et al. Combination acetabular radiofrequency ablation and cementoplasty using a navigational radiofrequency ablation device and ultrahigh viscosity cement: technical note. Skelet Radiol. 2016;45(3):401–5.
Guzik G. Cemented reconstruction of acetabular ceiling using the vertebroplasty set in treatment of metastatic lesions. Ortop Traumatol Rehabil. 2014;16(2):129–37.
Kim YI, Kang HG, Kim SK, et al. Clinical outcome prediction of percutaneous cementoplasty for metastatic bone tumor using (18)F-FDG PET-CT. Ann Nucl Med. 2013;27(10):916–23.
Zhang J, Yang Z, Wang J, et al. Study of treatment using percutaneous acetabuloplasty and interstitial implantation of (125)I seeds for patients with metastatic periacetabular tumors. World J Surg Oncol. 2012;10(1):250.
Acknowledgements
This work was sponsored by grant Natural Fund from Shanghai Science and Technology Commission (Grant numbers 18ZR1429400, 19411971800), China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, HF., Wu, CG., Tian, QH. et al. Application of Percutaneous Osteoplasty in Treating Pelvic Bone Metastases: Efficacy and Safety. Cardiovasc Intervent Radiol 42, 1738–1744 (2019). https://doi.org/10.1007/s00270-019-02320-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-019-02320-8