Abstract
Purpose
Wider breast cancer (BC) treatment options, short consultation time with physicians, lack of knowledge, and poor coping skills at the time of diagnosis may affect patients’ decisions causing treatment delays and non-adherence. To address this gap, a breast care nurse video orientation program was started. Our aim was to evaluate the video on patients’ knowledge, satisfaction, and treatment adherence.
Methods
The video was developed using the BC delay explanatory model. A self-administered pre- and post-survey on 241 newly diagnosed BC patients in University Malaya Medical Center was performed. The Wilcoxon matched paired signed rank test was used to evaluate patients’ pre and post perceived knowledge using a Likert scale 0 to 4 (0 = “no knowledge,” 4 = “a great degree of knowledge”). Treatment adherence among participants were measured after 1-year follow-up.
Results
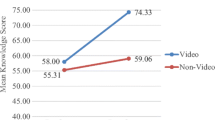
Eighty percent of the patients reported that the video met or exceeded their expectations. In total 80.5% reported that the video was very effective and effective in improving their perspective on BC treatments. There was improvement in perceived knowledge for treatment options (mean scores; M = 0.93 versus M = 2.97) (p < 0.001) and also for perceived knowledge on types of operation, information on chemotherapy, radiotherapy, hormone therapy, healthy diet, physical activity after treatments, and care of the arm after operation(p < 0.001). In total 89.4%, 79.3%, and 85.9% adhered to surgical, chemotherapy, and radiotherapy recommended treatment, respectively.
Conclusion
The video improved patients’ perceived knowledge and satisfaction. The program improved access not only to new BC patients but also the public and found sustainable using the YouTube platform.
Similar content being viewed by others
References
Ahmad NA et al (2017) Prevalence and determinants of disability among adults in Malaysia: results from the National Health and Morbidity Survey (NHMS) 2015. BMC Public Health 17(1):756
Abdullah NA et al (2013) Survival rate of breast cancer patients in Malaysia: a population-based study. Asian Pac J Cancer Prev 14(8):4591–4594
Taib NA, Yip CH, Low WY (2014) A grounded explanation of why women present with advanced breast cancer. World J Surg 38(7):1676–1684
Richard MA, Westcombe AM, Love SB et al (1999) Influences of delay on survival in patients with breast cancer: a systematic review. Lancet 353:1119–1126
Lim JN et al (2015) Barriers to early presentation of self-discovered breast cancer in Singapore and Malaysia: a qualitative multicentre study. BMJ Open 5(12):e009863
Dahlui M et al (2013) Breast screening and health issues among rural females in Malaysia: how much do they know and practice? Prev Med 57(Suppl):S18–S20
Yeoh ZY et al (2018) Feasibility of patient navigation to improve breast cancer care in Malaysia. J Glob Oncol 4:1–13
Blodt S et al (2018) Understanding the role of health information in patients’ experiences: secondary analysis of qualitative narrative interviews with people diagnosed with cancer in Germany. BMJ Open 8(3):e019576
Padrnos L et al (2018) Living with cancer: an educational intervention in cancer patients can improve patient-reported knowledge deficit. J Cancer Educ 33(3):653–659
Chan CM et al (2015) Prevalence and characteristics associated with default of treatment and follow-up in patients with cancer. Eur J Cancer Care (Engl) 24(6):938–944
Cheng ML et al (2019) Adherence rate and the factors contribute toward the surgical adherence of breast cancer in Malaysia. Breast J. https://doi.org/10.1111/tbj.13617
Chan CMH et al (2014) Default of cancer treatment association with psychological distress and desire for psychological support. J Clin Oncol 32(15):9567–9567. https://doi.org/10.1200/jco.2014.32.15_suppl.9567
Puts MT et al (2014) Factors influencing adherence to cancer treatment in older adults with cancer: a systematic review. Ann Oncol 25(3):564–577
Freund KM et al (2014) Impact of patient navigation on timely cancer care: the patient navigation research program. J Natl Cancer Inst 106(6). https://doi.org/10.1093/jnci/dju115
Bleicher RJ et al (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330–339
Rastogi P et al (2008) Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol 26(5):778–785
(EBCTCG)., E.B.C.T.C.G (2012) Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100000 women in 123 randomised trials. Lancet 379(9814):432–444
Srokowski TR et al (2008) Completion of adjuvant radiation therapy among women with breast cancer. Cancer 113(1):22–29
Gupta D, Bhatnagar S, Mishra S (2007) Defaulting oncology patient in a multispecialty state-run hospital in India. Am J Hosp Palliat Care 24(1):59–62
Chalela P et al (2018) Empowering Latina breast cancer patients to make informed decisions about clinical trials: a pilot study. Transl Behav Med 8(3):439–449
Gabitova G, Burke NJ (2014) Improving healthcare empowerment through breast cancer patient navigation: a mixed methods evaluation in a safety-net setting. BMC Health Serv Res 14:407
Keim-Malpass J et al (2018) Impact of patient health literacy on surgical treatment of breast cancer. Breast J 24(4):633–636
Jean-Pierre P et al (2011) Understanding the processes of patient navigation to reduce disparities in cancer care: perspectives of trained navigators from the field. J Cancer Educ 26(1):111–120
Freund KM et al (2008) National Cancer Institute Patient Navigation Research Program: methods, protocol, and measures. Cancer 113(12):3391–3399
Campbell C et al (2010) Implementing and measuring the impact of patient navigation at a comprehensive community cancer center. Oncol Nurs Forum 37(1):61–68
Koh C, Nelson JM, Cook PF (2011) Evaluation of a patient navigation program. Clin J Oncol Nurs 15(1):41–48
Schlueter DF et al (2010) A qualitative evaluation of the Avon Foundation Community Education and Outreach Initiative Patient Navigation Program. J Cancer Educ 25(4):571–576
Tang W et al (2017) Health literacy and functional exercise adherence in postoperative breast cancer patients. Patient Prefer Adherence 11:781–786
Raj A, Ko N, Battaglia TA et al (2012) Patient navigation for underserved patients diagnosed with breast cancer. Oncologist 17:1027–1031
Amudha P, Hamidah H, Ananth N et al (2018) Effective Communication between nurses and doctors: barriers as perceived by nurses. J Nurs Care 2167–1168. https://doi.org/10.4172/2167-1168.1000455
Freeman HP (2012) The origin, evolution, and principles of patient navigation. Cancer Epidemiol Biomark Prev 21(10):1614–1617
Stanley S et al (2013) Reducing barriers to breast cancer care through Avon patient navigation programs. J Public Health Manag Pract 19(5):461–467
Inthira Purusothaman LPH (2013) Development of concept among clinical nurses practitioners (CNS) in Malaysia. Malays J Nurs 5(1):12–15. https://ejournal.lucp.net/index.php/mjn/article/view/540/507
Information and Navigation for Treatment of Breast Cancer in University Malaya Medical Centre https://www.youtube.com/watch?v=iYJJPV_5nw4&t=5s. Accessed 14 Aug 2020
Acknowledgments
The authors wish to thank UMMC doctors, nurses, technical staff, hospital administration staff, and volunteers who contributed to the project.
Funding
The making of the CD was funded by the Breast Cancer Research Incentive Funds, and the printing of CD was funded by the Department of Surgery and Oncology Dept., UMMC. The study was also supported by High Impact Research Grant (UM.C/HIR/MOHE/06) from the Ministry of Education, Malaysia.
Author information
Authors and Affiliations
Contributions
Conception and design: Nur Aishah Taib, Ranjit Kaur, and Tania Islam
Collection and assembly of data: See Mee Hoong, Suniza Jamaris, Suhaida Musthaffa, Noraizam Abdullah Din, Zarinah Abd Rahman, Kamar Noraini bt Mohamed, Jasmine Filza, Mao Li Cheng, Faizah Harun, Gwo Fuang Ho, and Tania Islam
Data analysis and interpretation: Tania Islam and Nur Aishah Taib
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
Corresponding author
Ethics declarations
The completion and return of the questionnaire was regarded as consent to participate in this study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Islam, T., Musthaffa, S., Hoong, S.M. et al. Development and evaluation of a sustainable video health education program for newly diagnosed breast cancer patients in Malaysia. Support Care Cancer 29, 2631–2638 (2021). https://doi.org/10.1007/s00520-020-05776-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05776-4