Abstract
Purpose
Among the prognostic factors relevant to the condition of oncological patients, nutritional status (NS) has the greatest single impact on quality of life (QL). The goals of our study were to evaluate the influence of NS, weight loss (WL), and the presence of cachexia, prior to the initiation of chemotherapy, on the patient’s QL.
Methods
Adult patients (aged ≥ 18 years) diagnosed with solid tumours for whom chemotherapy was started between April 2016 and June 2017 were eligible for inclusion in the study. They were asked to complete a QL questionnaire (Functional Assessment of Cancer Treatment (FACT-G)) at the beginning. The presence or absence of cachexia was evaluated at the outset, following the definition proposed by Fearon and nutritional assessment by the Patient-Generated Subjective Global Assessment (PG-SGA) scale.
Results
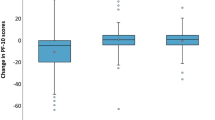
A total of 177 patients completed the FACT-G, the 60% receiving curative therapy. At the start of the treatment, 58.2% of patients had experienced WL, with an average of 4.4 ± 7.4%, and 19% were at risk of malnutrition. Patient who presented cachexia at diagnosis, were treated with palliative intention, had a Nutriscore ≥ 5 points or presented malnutrition in accordance with PG-SGA had a poorer QL (p < 0.05). Greater WL was associated with a worsened QL (p = 0.001). Breast cancer patients presented an inverse correlation between the %WL and the initial score in the FACT-G (r = − 0.304, p = 0.023), whereas no such correlation was observed for the other types of tumour (r = − 0.012, p = 0.892).
Conclusions
These results underline the relation of NS before starting chemotherapy and QL. Greater WL was associated with a worsened QL, especially in women with breast cancer.

Similar content being viewed by others
References
Segura A, Pardo J, Jara C, Zugazabeitia L, Carulla J, de Las PR et al (2005) An epidemiological evaluation of the prevalence of malnutrition in Spanish patients with locally advanced or metastatic cancer. Clin Nutr 24:801–814. https://doi.org/10.1016/j.clnu.2005.05.001
Planas M, Álvarez-Hernández J, León-Sanz M, Celaya-Pérez S, Araujo K, García de Lorenzo A et al (2016) Prevalence of hospital malnutrition in cancer patients: a sub-analysis of the PREDyCES study. Support Care Cancer 24(1):429–435. https://doi.org/10.1007/s00520-015-2813-7
Seo SH, Kim SE, Kang YK, Ryoo BY, Ryu MH, Jeong JH et al (2016) Association of nutricional status-related indices and chemotherapy-induced adverse events in gastric cancer patients. BMC Cancer 16(1):900. https://doi.org/10.1186/s12885-016-2934-5
Aaldriks AA, van der Geest LG, Giltay EJ, le Cessie S, Portielje JE, Tanis BC et al (2013) Frailty and malnutrition predictive of mortality risk in older patients with advanced colorectal cancer receiving chemotherapy. J Geriatr Oncol 4(3):218–226. https://doi.org/10.1016/j.jgo.2013.04.001
Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Maeda S, Haraguchi N et al (2015) Prevalence of Malnutrition Among Gastric Cancer Patients Undergoing Gastrectomy and Optimal Preoperative Nutritional Support for Preventing Surgical Site Infections. Ann Surg Oncol 22(3):S778–S785. https://doi.org/10.1245/s10434-015-4820-9
Bozzetti F, Gianotti L, Braga M, Di Carlo V, Mariani L (2007) Postoperative complications in gastrointestinal cancer patients: the joint role of the nutritional status and the nutritional support. Clin Nutr 26(6):698–709. https://doi.org/10.1016/j.clnu.2007.06.009
Van Cutsem E, Arends J (2005) The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs 9(2):S51–S63. https://doi.org/10.1016/j.ejon.2005.09.007
Gellrich NC, Handschel J, Holtmann H, Krüskemper G (2015) Oral cancer malnutrition impacts weight and quality of life. Nutrients 7(4):2145–2160. https://doi.org/10.3390/nu7042145
Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME (2004) Cancer: disease and nutrition are key determinants of patients´ quality of life. Support Care Cancer 12(4):246–252. https://doi.org/10.1007/s00520-003-0568-z
Gómez-Candela C, Canales Albendea MA, Palma Milla S, de Paz AR, Díaz Gómez J, Rodríguez-Durán D et al (2012) Intervención nutricional en el paciente oncohematológico. Nutr Hosp 27(3):669–680. https://doi.org/10.3305/nh.2012.27.3.5863
Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR et al (1980) Prognostic effect of weight loss prior to chemotherapy in cancer patients. Am J Med 69:491–497
World Health Organization (1995) World Health Organization Quality of life Assessment (WHOQOL): Position paper from the World Health Organization. Soc Sci Med 41:1403–1409
Wanden-Berghe C, Cheikh Moussa K, Sanz-Valero J (2015) La calidad de vida y el estado nutricional. Nutr Clin Med IX(2):133–144. https://doi.org/10.7400/NCM.2015.09.2.5026
Isenring E, Bauer J, Capra S (2003) The scored Patient-Generated Subjective Global Assessment (PG-SGA) and its association with quality of life in ambulatory patients receiving radiotherapy. Eur J Clin Nutr 57(2):305–309. https://doi.org/10.1038/sj.ejcn.1601552
Álvaro Sanz E, Garrido Siles M, Rey Fernández L, Villatoro Roldán R, Rueda Domínguez A, Abies J (2019) Nutritional risk and malnutrition rates at diagnosis of cancer in patients treated in out patient settings: Early intervention protocol. Nutrition 57:148–153. https://doi.org/10.1016/j.nut.2018.05.021
Dapueto JJ, Servente L, Francolino C, Hahn EA (2005) Determinants of Quality of Life in Patients with Cancer. Cancer 103(5):1072–1081. https://doi.org/10.1002/cncr.20870
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A et al (1993) The Functional Assessment of Cancer Therapy Scale: development and validation of the general measure. J Clin Oncol 11(3):570–579. https://doi.org/10.1200/JCO.1993.11.3.570
Moinpour CM, Feigl P, Metch B, Hayden KA, Meyskens FL Jr, Crowley J (1989) Quality of life end points in cancer clinical trials: review and recommendations. J Natl Cancer Inst 81(7):485–495. https://doi.org/10.1093/jnci/81.7.485
Fonseca M, Schlack C, Mera E, Muñoz O, Peña L. (2013). mEvaluación de la calidad de vida en pacientes con cáncer terminal. Rev Chil Cir 65(4): 321-8. https://doi.org/10.4067/S0718-40262013000400006. https://scielo.conicyt.cl/scielo.php?script=sci_arttext&pid=S0718-40262013000400006&lng=es. Accessed 2019 Ago 31
FACT-G Scoring Guiedlines. Version 4. www.facit.org Accessed 20 may 2016
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12:489–495. https://doi.org/10.1016/S1470-2045(10)70218-7
Arribas L, Hurtós L, Sendrós MJ, Peiró I, Salleras N, Fort E, Sanchez-Migallon JM (2017) Nutriscore: A new nutritional screening tool for oncological outpatients. Nutrition 33:297–303. https://doi.org/10.1016/j.nut.2016.07.015
McMillan DC (2013) The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev 39(5):534–540. https://doi.org/10.1016/j.ctrv.2012.08.003
Dehkordi A, Heydarnejad MS, Fatehi D (2009) Quality of life in cancer patients undergoing chemotherapy. Oman Med J 24(3):204–207. https://doi.org/10.5001/omj.2009.40
Oñate-Ocaña LF, Ochoa-Carrillo FJ (2013) Evaluación de la calidad de vida relacionada con la salud en pacientes con cáncer. Gaceta Mexicana de Oncología 12(6):379–381
Popovic M, Lao N, Bedard G, Zeng L, Zhang L, Cella D et al (2013) Quality of Life in Patients with Advanced Cancer Using the Functional Assessment of Cancer Therapy-General Assessment Tool: A Literature Review. World J Oncol 4(1):8–17. https://doi.org/10.4021/wjon594w
Lis CG, Gupta D, Lammersfeld CA, Markman M, Vashi PG (2012) Role of nutritional status in predicting quality of life outcomes in cancer – a systematic review of the epidemiological literature. Nutr J 24(11):27. https://doi.org/10.1186/1475-2891-11-27
Luckett T, King MT, Butow PN, Oguchi M, Rankin N, Price MA, Hackl NA, Heading G (2011) Choosing between the EORTC QLQ-C30 and FACT-G for measuring health-related quality of life in cancer clinical research: issues, evidence and recommendations. Ann Oncol 22(10):2179–2190. https://doi.org/10.1093/annonc/mdq721
Vanhoutte G, van de Wiel M, Wouters K, Sels M, Bartolomeeussen L, De Keersmaecker S et al (2019) Cachexia in cancer: what is in the definition? BMJ open gastroenterol 3(1):e000097. https://doi.org/10.1136/bmjgast-2016-000097
Bauer JD, Capra S (2005) Nutrition intervention improves outcomes in patients with cancer cachexia receivingchemotherapy—a pilot study. Support Care Cancer 13(4):270–274. https://doi.org/10.1007/s00520-004-0746-7
Ravasco P, Monteiro-Grillo I, Marques Vidal P, Camilo ME (2005) Impact of nutrition on outcome: A prospective randomized controlled trial in patients with head and neck cancer undergoing radiotherapy. Head Neck 27(8):659–668. https://doi.org/10.1002/hed.20221
Garcia-Peris P, Paron L, Velasco C, de la Cuerda C, Camblo M, Breton I et al (2007) Long-term prevalence of oropharyngeal dysphagia in head and neck cancer patients: Impact on quality of life. Clin Nutr 26(26):710–717. https://doi.org/10.1016/j.clnu.2007.08.006
Takayama K, Atagi S, Imamura F, Tanaka H, Minato K, Harada T (2016) Quality of life and survival survey of cancer cachexia in advanced non-small cell lung cancer patients-Japan nutrition and QOL survey in patients with advanced non-small cell lung cancer study. Support Care Cancer 24(8):3473–3480. https://doi.org/10.1007/s00520-016-3156-8
Lester J, Crosthwaite K, Stout R, Jones RN, Holloman C, Shapiro C, Andersen BL (2015) Oncol Nurs Forum 42(1):E17–E23. https://doi.org/10.1188/15.ONF.E17-E23
Engel J, Kerr J, Schlesinger-Raab A, Sauer H, Hölzel D (2004) Quality of life following breast conserving therapy or mastectomy: results of a 5-year prospective study. Breast J10(3):223–231. https://doi.org/10.1111/j.1075-122X.2004.21323.x
Salas S, Mercier S, Moheng B, Olivet S, Garcia ME, Hamon S et al (2017) Nutritional status and quality of life of cancer patients needing exclusive chemotherapy: a longitudinal study. Health Qual Life Outcomes 15(1):85. https://doi.org/10.1186/s12955-017-0660-6
Handschel J, Naujoks C, Hofer M, Kruskemper G (2013) Psychological aspects affect quality of life in patients with oral squamous cell carcinomas. Psychooncology 22(3):677–682. https://doi.org/10.1002/pon.3052
Handschel J, Naujoks C, Kubler NR, Kruskemper G (2012) Fear of recurrence significantly influences quality of life in oral cancer patients. Oral Oncol 48(12):1276–1280. https://doi.org/10.1016/j.oraloncology.2012.06.015
August DA, Huhmann MB, American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors (2009) A.S.P.E.N. clinical guidelines: nutrition support therapy during adult anticancer treatment and in hematopoietic cell transplantation. JPEN J Parenter Enteral Nutr 33(5):472–500. https://doi.org/10.1177/0148607109341804
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F et al (2017) ESPEN guidelines on nutrition in cancer patients. Clin Nutr 36(1):11–48. https://doi.org/10.1016/j.clnu.2016.07.015
Acknowledgements
The authors of the work want to thank the hospital day and Pharmacy Service staff (specially Begoña Tortajada Goitia) and patients for their collaboration. We thank the research team at the Agencia Sanitaria Costa del Sol for their support. The present study is part os a PhD. Research programme being conducted at the University of Málaga. This work was partially presented at the III announcement of the SEFH-ROVI to the development of the hospital pharmacy, getting one award to best work. The award has been delivered at the 64 National Congress of the Spanish Society of Hospital Pharmacy held in Seville, Spain, in October 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Agencia Sanitaria Costa del Sol Ethics Committee. All patients provided written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Álvaro Sanz, E., Abilés, J., Garrido Siles, M. et al. Impact of weight loss on cancer patients’ quality of life at the beginning of the chemotherapy. Support Care Cancer 29, 627–634 (2021). https://doi.org/10.1007/s00520-020-05496-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05496-9