Abstract
Purpose
To synthesize the characteristics and effects of couple-based intervention on sexuality and the quality of life (QOL) of cancer patients and their intimate partners and its implications for future research and practice.
Methods
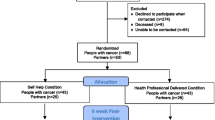
A systematic review and meta-analysis of randomized and non-randomized controlled studies of interventions was conducted in nine English databases and two Chinese databases, with identification of related studies published in English and Chinese. The quality of the studies was assessed using the tools of the Effective Public Health Practice Project.
Results
A total of 33 articles were identified for systematic review and 23 articles were identified for meta-analysis. For patients, the effect size was 0.42 (Hedges’s g, 95% CI = 0.05–0.78, p = 0.03) for physical health. For partners, the effect size was 0.52 (Hedges’s g, 95% CI = 0.06–0.98, p = 0.03) for sexual relationships. However, moderate to high heterogeneity was reported. Effects on sexual function, sexual self-concept, and mental health for couples were not significant.
Conclusion
Couple-based interventions had small to medium-sized effects on physical health for cancer patients. Partners could derive medium effects for improvement in sexual relationships from couple-based intervention. Future research should pay more attention to sexual self-concept in cancer patients and target types of cancer that are more likely to compromise sexuality and QOL.
PROSPERO registration
The systematic review and meta-analysis has been registered in PROSPERO with registration number: CRD42019119047.





Similar content being viewed by others
Change history
26 May 2020
Sentence incorrect.
References
Wang F, Luo D, Fu L, Zhang H, Wu S, Zhang M, Zhou H, Sun T, Chen X (2017) The efficacy of couple-based interventions on health-related quality of life in cancer patients and their spouses: a meta-analysis of 12 randomized controlled trials. Cancer Nurs 40:39–47. https://doi.org/10.1097/NCC.0000000000000356
Badr H, Carmack CL, Milbury K, Temech M (2013) Psychosocial interventions for couples coping with cancer: a systematic review. In: Psychological aspects of cancer. Springer, pp 177–198
Li Q, Loke AY (2013) A spectrum of hidden morbidities among spousal caregivers for patients with cancer, and differences between the genders: a review of the literature. Eur J Oncol Nurs 17:578–587. https://doi.org/10.1016/j.ejon.2013.01.007
Badr H, Taylor CLC (2009) Sexual dysfunction and spousal communication in couples coping with prostate cancer. Psychooncology 18:735–746. https://doi.org/10.1002/pon.1449
Scott JL, Kayser K (2009) A review of couple-based interventions for enhancing women’s sexual adjustment and body image after cancer. Cancer J 15:48–56. https://doi.org/10.1097/PPO.0b013e31819585df
Avis NE, Crawford S, Manuel J (2005) Quality of life among younger women with breast cancer. J Clin Oncol 23:3322–3330. https://doi.org/10.1200/JCO.2005.05.130
Bakker RM, Mens JWM, de Groot HE, Tuijnman-Raasveld CC, Braat C, Hompus WC, Poelman JG, Laman MS, Velema LA, de Kroon CD, van Doorn H, Creutzberg CL, ter Kuile M (2017) A nurse-led sexual rehabilitation intervention after radiotherapy for gynecological cancer. Support Care Cancer 25:729–737. https://doi.org/10.1007/s00520-016-3453-2
Bober SL, Recklitis CJ, Michaud AL, Wright AA (2017) Improvement in sexual function after ovarian cancer: sexual therapy and rehabilitation after treatment for ovarian cancer (START-OC). J Clin Oncol 35:210–210. https://doi.org/10.1200/JCO.2017.35.5_suppl.210
Jun E-Y, Kim S, Chang S-B, Oh K, Kang HS, Kang SS (2011) The effect of a sexual life reframing program on marital intimacy, body image, and sexual function among breast cancer survivors. Cancer Nurs 34:142–149. https://doi.org/10.1097/NCC.0b013e3181f1ab7a
Giesler RB, Given B, Given CW, Rawl S, Monahan P, Burns D, Azzouz F, Reuille KM, Weinrich S, Koch M, Champion V (2005) Improving the quality of life of patients with prostate carcinoma: a randomized trial testing the efficacy of a nurse-driven intervention. Cancer 104:752–762. https://doi.org/10.1002/cncr.21231
Molassiotis A, Chan CWH, Yam BMC, Chan ES, Lam CS (2002) Life after cancer: adaptation issues faced by Chinese gynaecological cancer survivors in Hong Kong. Psychooncology 11:114–123. https://doi.org/10.1002/pon.540
Carter J, Lacchetti C, Andersen BL, Barton DL, Bolte S, Damast S, Diefenbach MA, DuHamel K, Florendo J, Ganz PA, Goldfarb S, Hallmeyer S, Kushner DM, Rowland JH (2018) Interventions to address sexual problems in people with Cancer: American Society of Clinical Oncology clinical practice guideline adaptation of Cancer Care Ontario guideline. J Clin Oncol 36:492–511. https://doi.org/10.1200/JCO.2017.75.8995
Li Q, Loke AY (2014) A systematic review of spousal couple-based intervention studies for couples coping with cancer: direction for the development of interventions. Psychooncology 23:731–739. https://doi.org/10.1002/pon.3535
Scott JL, Halford WK, Ward BG (2004) United we stand? The effects of a couple-coping intervention on adjustment to early stage breast or gynecological cancer. J Consult Clin Psychol 72:1122–1135. https://doi.org/10.1037/0022-006X.72.6.1122
Nelson CJ, Emanu JC, Avildsen I (2015) Couples-based interventions following prostate cancer treatment: a narrative review. Transl Androl Urol 4:232–242. https://doi.org/10.3978/j.issn.2223-4683.2015.04.04
Badr H, Krebs P (2013) A systematic review and meta-analysis of psychosocial interventions for couples coping with cancer. Psychooncology 22:1688–1704. https://doi.org/10.1002/pon.3200
Baik OM, Adams KB (2011) Improving the well-being of couples facing cancer: a review of couples-based psychosocial interventions. J Marital Fam Ther 37:250–266. https://doi.org/10.1111/j.1752-0606.2010.00217.x
Jonsdottir JI, Jonsdottir H, Klinke ME (2018) A systematic review of characteristics of couple-based intervention studies addressing sexuality following cancer. J Adv Nurs 74:760–773. https://doi.org/10.1111/jan.13470
WHO (2018) Cancer today. http://gco.iarc.fr/today/fact-sheets-populations
Cleary V, Hegarty J (2011) Understanding sexuality in women with gynaecological cancer. Eur J Oncol Nurs 15:38–45. https://doi.org/10.1016/j.ejon.2010.05.008
Ware J (1994) SF-36 physical and mental health summary scales: a user’s manual. Health Institute New England Medical Center, Boston
Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG (2012) Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias tool and the effective public health practice project quality assessment tool: methodological research. J Eval Clin Pract 18:12–18. https://doi.org/10.1111/j.1365-2753.2010.01516.x
Thomas BH, Ciliska D, Dobbins M, Micucci S (2004) A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid-Based Nurs 1:176–184. https://doi.org/10.1111/j.1524-475X.2004.04006.x
Borenstein M, Hedges L, Higgins J, Rothstein H (2005) Comprehensive meta-analysis
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2011) Introduction to meta-analysis. Wiley
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Eribaum, Hillsdale
Leta S, Alemayehu G, Seyoum Z, Bezie M (2016) Prevalence of bovine trypanosomosis in Ethiopia: a meta-analysis. Parasit Vectors 9:139. https://doi.org/10.1186/s13071-016-1404-x
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Manne SL, Kissane DW, Nelson CJ, Mulhall JP, Winkel G, Zaider T (2011) Intimacy-enhancing psychological intervention for men diagnosed with prostate cancer and their partners: a pilot study. J Sex Med 8:1197–1209. https://doi.org/10.1111/j.1743-6109.2010.02163.x
Baucom DH, Porter LS, Kirby JS, Gremore TM, Wiesenthal N, Aldridge W, Fredman SJ, Stanton SE, Scott JL, Halford KW, Keefe FJ (2009) A couple-based intervention for female breast cancer. Psychooncology 18:276–283. https://doi.org/10.1002/pon.1395
Northouse LL, Mood DW, Schafenacker A, Montie JE, Sandler HM, Forman JD, Hussain M, Pienta KJ, Smith DC, Kershaw T (2007) Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer 110:2809–2818. https://doi.org/10.1002/cncr.23114
Decker CL, Pais S, Miller KD, Goulet R, Fifea BL (2012) A brief intervention to minimize psychosexual morbidity in dyads coping with breast cancer. Oncol Nurs Forum 39:176–185. https://doi.org/10.1188/12.ONF.176-185
Chunyan C, Yaqing L, Liqun T (2015) Influence of life boat club mode of health education on quality of life of patients with breast cancer and their spouses. Chin Nurs Res 29:2070–2075. https://doi.org/10.3969/j.issn.1009-6493.2015.17.008
Winters-Stone K, Lyons K, Dobek J, Dieckmann NF, Bennett JA, Nail L, Beer TM (2016) Benefits of partnered strength training for prostate cancer survivors and spouses: results from a randomized controlled trial of the exercising together project. J Cancer Surviv 10:633–644. https://doi.org/10.1007/s11764-015-0509-0
Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW (2010) Interventions with family caregivers of cancer patients: meta-analysis of randomized trials. CA Cancer J Clin 60:317–339. https://doi.org/10.3322/caac.20081
Pisu M, Demark-Wahnefried W, Kenzik KM, Oster RA, Lin CP, Manne S, Alvarez R, Martin MY (2017) A dance intervention for cancer survivors and their partners (RHYTHM). J Cancer Surviv 11:350–359. https://doi.org/10.1007/s11764-016-0593-9
Porter LS, Gao X, Lyna P, Kraus W, Olsen M, Patterson E, Puleo B, Pollak KI (2018) Pilot randomized trial of a couple-based physical activity videoconference intervention for sedentary cancer survivors. Health Psychol 37:861–865. https://doi.org/10.1037/hea0000608
Campbell LC, Keefe FJ, Scipio C et al (2007) Facilitating research participation and improving quality of life for African American prostate cancer survivors and their intimate partners: a pilot study of telephone-based coping skills training. Cancer Interdiscip Int J Am Cancer Soc 109:414–424. https://doi.org/10.1002/cncr.22355
Reese JB, Porter LS, Regan KR et al (2014) A randomized pilot trial of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer. Psychooncology 23:1005–1013. https://doi.org/10.1002/pon.3508
McCorkle R, Siefert ML, Dowd MF et al (2007) Effects of advanced practice nursing on patient and spouse depressive symptoms, sexual function, and marital interaction after radical prostatectomy. Urol Nurs 27:65–77
Shields CG, Rousseau SJ (2004) A pilot study of an intervention for breast cancer survivors and their spouses. Fam Process 43:95–107. https://doi.org/10.1111/j.1545-5300.2004.04301008.x
Chen H-L, Liu K, You Q-S (2017) Effects of couple based coping intervention on self-efficacy and quality of life in patients with resected lung cancer. Patient Educ Couns 100:2297–2302
Manne SL, Kashy DA, Zaider T, Kissane D, Lee D, Kim IY, Heckman CJ, Penedo FJ, Murphy E, Virtue SM (2019) Couple-focused interventions for men with localized prostate cancer and their spouses: a randomized clinical trial. Br J Health Psychol 24:396–418. https://doi.org/10.1111/bjhp.12359
Robertson J, McNamee P, Molloy G, Hubbard G, McNeill A, Bollina P, Kelly D, Forbat L (2016) Couple-based psychosexual support following prostate cancer surgery: results of a feasibility pilot randomized control trial. J Sex Med 13:1233–1242. https://doi.org/10.1016/j.jsxm.2016.05.013
Chambers SK, Occhipinti S, Schover L, Nielsen L, Zajdlewicz L, Clutton S, Halford K, Gardiner RA, Dunn J (2015) A randomised controlled trial of a couples-based sexuality intervention for men with localised prostate cancer and their female partners. Psycho-Oncology 24:748–756. https://doi.org/10.1002/pon.3726
McLean LM, Walton T, Rodin G, Esplen MJ, Jones JM (2013) A couple-based intervention for patients and caregivers facing end-stage cancer: outcomes of a randomized controlled trial. Psychooncology 22:28–38. https://doi.org/10.1002/pon.2046
Xin Z, Zhao Weiyu FD (2014) Effect of psychological intervention on the postoperative quality of life of patients with breast cancer and their spouses. Hainan Med J 25:776–778. https://doi.org/10.3969/j.issn.1003-6350.2014.05.0304
Canada AL, Neese LE, Sui D, Schover LR (2005) Pilot intervention to enhance sexual rehabilitation for couples after treatment for localized prostate carcinoma. Cancer Interdiscip Int J Am Cancer Soc 104:2689–2700. https://doi.org/10.1002/cncr.21537
Badr H, Herbert K, Chhabria K, Sandulache VC, Chiao EY, Wagner T (2019) Self-management intervention for head and neck cancer couples: results of a randomized pilot trial. Cancer 125:1176–1184. https://doi.org/10.1002/cncr.31906
Badr H, Herbert K, Bonnen MD, Asper JA, Wagner T (2018) Dyadic coping in patients undergoing radiotherapy for head and neck cancer and their spouses. Front Psychol 9:1780. https://doi.org/10.3389/fpsyg.2018.01780
Nho J-H, Kim YH, Kook H-J (2019) Effect of a web-based sexual health enhancement program for women with gynecologic cancer and their husbands. Int J Sex Heal 1–10. https://doi.org/10.1080/19317611.2019.1565792
Fu W, Hong LL, Liu CY et al (2007) Research on effects of psychological intervention on quality of life of cancer patients and their spouses. Chin J Cancer Prev Treat 14:1770–1774
Lambert SD, McElduff P, Girgis A, Levesque JV, Regan TW, Turner J, Candler H, Mihalopoulos C, Shih STF, Kayser K, Chong P (2016) A pilot, multisite, randomized controlled trial of a self-directed coping skills training intervention for couples facing prostate cancer: accrual, retention, and data collection issues. Support Care Cancer 24:711–722. https://doi.org/10.1007/s00520-015-2833-3
McCaughan E, Curran C, Northouse L, Parahoo K (2018) Evaluating a psychosocial intervention for men with prostate cancer and their partners: outcomes and lessons learned from a randomized controlled trial. Appl Nurs Res 40:143–151. https://doi.org/10.1016/j.apnr.2018.01.008
Kuijer RG, Buunk BP, De Jong GM et al (2004) Effects of a brief intervention program for patients with cancer and their partners on feelings of inequity, relationship quality and psychological distress. Psychooncology 13:321–334. https://doi.org/10.1002/pon.749
Nicolaisen A, Hagedoorn M, Hansen DG, Flyger HL, Christensen R, Rottmann N, Lunn PB, Terp H, Soee K, Johansen C (2018) The effect of an attachment-oriented couple intervention for breast cancer patients and partners in the early treatment phase: a randomised controlled trial. Psychooncology 27:922–928. https://doi.org/10.1002/pon.4613
Jing W, Dongxue S (2016) The application of individualized nursing intervention in improving the quality of life of breast cancer patients and their spouses. Hainan Med J 27:2576–2578. https://doi.org/10.3969/j.issn.1003
Hsiao F-H, Jow G-M, Kuo W-H, Yang PS, Lam HB, Chang KJ, Lee JJ, Huang CS, Lai YM, Chen YT, Liu YF, Chang CH (2016) The long-term effects of mindfulness added to family resilience-oriented couples support group on psychological well-being and cortisol responses in breast cancer survivors and their partners. Mindfulness (N Y) 7:1365–1376. https://doi.org/10.1007/s12671-016-0578-9
Arden-Close E, Gidron Y, Bayne L, Moss-Morris R (2013) Written emotional disclosure for women with ovarian cancer and their partners: randomised controlled trial. Psychooncology 22:2262–2269. https://doi.org/10.1002/pon.3280
Chambers SK, Occhipinti S, Stiller A, Zajdlewicz L, Nielsen L, Wittman D, Oliffe JL, Ralph N, Dunn J (2019) Five-year outcomes from a randomised controlled trial of a couples-based intervention for men with localised prostate cancer. Psychooncology 28:775–783. https://doi.org/10.1002/pon.5019
Farivar SS, Cunningham WE, Hays RD (2007) Correlated physical and mental health summary scores for the SF-36 and SF-12 health survey, V.I. Health Qual Life Outcomes 5:54. https://doi.org/10.1186/1477-7525-5-54
Thornton AA, Perez MA, Meyerowitz BE (2004) Patient and partner quality of life and psychosocial adjustment following radical prostatectomy. J Clin Psychol Med Settings 11:15–30. https://doi.org/10.1023/B:JOCS.0000016266.06253.95
Boehmer U, Miao X, Ozonoff A (2011) Cancer survivorship and sexual orientation. Cancer 117:3796–3804. https://doi.org/10.1002/cncr.25950
Hamed SGA, El-Etreby RR, Mahgoub NA et al (2019) Impact of psycho-educational program on body image concerns and mental adjustment among post mastectomy women. Int J Nurs Didact 9:48–57. https://doi.org/10.15520/IJND.V9I01.2423
Walker LM, Wassersug RJ, Robinson JW (2015) Psychosocial perspectives on sexual recovery after prostate cancer treatment. Nat Rev 12:167–176. https://doi.org/10.1038/nrurol.2015.29
Buffart LM, Kalter J, Sweegers MG et al (2017) Effects and moderators of exercise on quality of life and physical function in patients with cancer: an individual patient data meta-analysis of 34 RCTs. Cancer Treat Rev 52:91–104. https://doi.org/10.1016/J.CTRV.2016.11.010
Schover LR, Canada AL, Yuan Y, Sui D, Neese L, Jenkins R, Rhodes MM (2012) A randomized trial of internet-based versus traditional sexual counseling for couples after localized prostate cancer treatment. Cancer 118:500–509. https://doi.org/10.1002/cncr.26308
Chow KM, Chan JCY, Choi KKC, Chan CWH (2016) A review of psychoeducational interventions to improve sexual functioning, quality of life, and psychological outcomes in gynecological cancer patients. Cancer Nurs 39:20–31. https://doi.org/10.1097/NCC.0000000000000234
Montgomery Sklar E (2017) Body image, weight, and self-concept in men. Am J Lifestyle Med 11:252–258. https://doi.org/10.1177/1559827615594351
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. No funding support. The corresponding author has full control of all primary data and agrees to allow the journal to review the data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Li, M., Chan, C.W.H., Chow, K.M. et al. A systematic review and meta-analysis of couple-based intervention on sexuality and the quality of life of cancer patients and their partners. Support Care Cancer 28, 1607–1630 (2020). https://doi.org/10.1007/s00520-019-05215-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05215-z