Abstract
Purpose
Breast cancer is associated with high levels of psychological distress. Mindfulness-based stress reduction (MBSR) has proven to be effective in reducing distress in cancer patients. In several studies, patients who are currently undergoing somatic anticancer treatment are excluded from participating in MBSR. Little is known about what would be the most suitable stage of disease to offer MBSR. We examined whether stage of disease facilitated and/or hindered participation in MBSR for breast cancer patients.
Method
A mixed method design was used. Self-report questionnaires on psychological distress (HADS) and quality of life (EORTC QLQ-C30) were administered before and after MBSR. Five focus groups and three semi-structured individual interviews were conducted. Qualitative data were analyzed with the constant comparative method in order to develop a grounded theory.
Results
Sixty-four females participated in MBSR. In 52 patients who completed the questionnaires, psychological distress improved significantly. Qualitative data showed that participating in MBSR both during and after anticancer treatment has specific advantages and disadvantages. Interestingly, being emotionally ready to take part in MBSR seems equally important as physical ability. Informing patients at an early stage seemed to strengthen autonomy and self-management skills.
Conclusions
In contrast to the common practice to tailoring the timing of MBSR to physical impairments or demands of the anticancer treatment, our findings revealed that emotional readiness is equally important to take into account. These findings might support professionals in their choices whether and when to inform and refer patients to MBSR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer among women with an estimated 1.67 million new cancer cases each year [1]. The invasive treatment and physical symptoms have a major impact on patients’ wellbeing. Henselmans [2] showed that during active anticancer treatment, 33% of breast cancer patients suffer from psychological distress, 15% of patients experience distress directly after treatment in the reentry phase, and another 15% remain distressed for several years. So, psychological consequences of the cancer and/or its treatment seem to be long-lasting [3]. Psychological interventions have been shown to be effective in reducing these symptoms [4,5,6]. An innovative intervention in cancer patients is mindfulness-based stress reduction (MBSR). Mindfulness is defined as intentionally paying attention to present-moment experiences in an accepting and non-judgmental way [7]. Recent meta-analyses concluded that MBSR and other mindfulness-based interventions (MBIs) are effective in decreasing psychological distress in cancer patients [8, 9], including reductions of anxiety and depressive symptoms and improvement of quality of life.
With a few exceptions [10], in clinical practice and research settings, MBSR is mostly offered after the active anticancer treatment phase [11,12,13]. As anticancer treatment poses a burden on patients mental and physical wellbeing [2, 3], it can interfere with participation in psychosocial group interventions. When patients miss several sessions, the intervention might not be as effective.
Consequently, although one third of women experience psychological distress during active anticancer treatment, they often need to wait before they can participate in MBSR. Interestingly, a recent meta-analysis on uptake and adherence of psychological interventions for cancer patients demonstrated that patients were more likely to accept an intervention close to their diagnosis [14]. Patients who were offered a psychological intervention during active anticancer treatment were not, however, more likely to drop out than those who received a support offer before treatment.
Little is known about what patients themselves experience as the most suitable time to participate in psychosocial interventions such as MBSR. The aim of this study is to explore how patients experience the possible benefits and impediments of participation in MBSR during different stages of their anticancer treatment. This could be of help to practitioners and researchers in their choices about what is a suitable time to enroll patients in MBSR.
Materials and methods
Setting and study population
Patients with breast cancer were recruited at the departments of oncology of the Radboud University Medical Centre in Nijmegen, hospital Rijnstate in Arnhem, and through the website of a funding agency for breast cancer patients (www.pinkribbon.nl) from September 2012 to March 2014. Patients were included when they had been diagnosed with breast cancer, were at least 18 years old, and able to understand and use the Dutch language. No further eligibility criteria or sampling techniques were used. All participants provided written informed consent. The local ethics committee indicated that as this was an uncontrolled cohort study of an intervention already used in clinical care, no formal approval was required (registration number CMO 2012/493).
Procedure
After referral, patients were invited for a research interview at the Radboudumc Centre for Mindfulness. They filled out self-report questionnaires on psychosocial functioning before and after MBSR. Some patients participated in MBSR for breast cancer patients only and they were invited for a focus group interview with their fellow participants 1 week after completion of the training. Some patients participated with their partner in MBSR for patients with various types of cancer. They were invited for an individual interview after completing the course.
Intervention
MBSR consists of 8-weekly group-based 2.5-h sessions, a 6-h silent day between sessions 6 and 7, and daily 45-min home practice. The curriculum was based on the treatment format developed by Kabat-Zinn [7]. The sessions consisted of mindfulness practices, didactic teaching on stress, and sharing experiences with one another. Participants received a CD with guided meditations and a workbook with written information. To tailor the intervention to cancer patients, psycho-education about grief was added [15]. Furthermore, patients could invite their partner or close other to attend a session on mindful communication, discussing the impact of cancer on their relationship. The training was conducted by a qualified health professional and mindfulness teacher who fulfilled the mindfulness-based intervention teacher assessment criteria [16].
Quantitative assessment
Psychological distress
We used the total scale of the 14-item Hospital Anxiety and Depression Scale (HADS), which was developed to measure psychological distress in somatic patient populations. It consists of an anxiety and depression subscale [17].
Rumination
The Ruminative Response Scale (RRS) was used to measure rumination and distinguishes a more adaptive thinking style (reflection) from a more maladaptive one (brooding [18]. We used the 5-item brooding subscale.
Quality of life
The European Organization for Research and Treatment of Cancer (EORTC) Core Quality of Life Questionnaire (QLQ-C30) was used to assess quality of life [19]. It contains several functioning and symptom subscales. We used the Global Quality of Life, emotional and physical functioning subscales.
Well-being
The 14-item Warwick-Edinburgh Mental Well-being Scale (WEMWBS) measures wellbeing [20]. It contains the majority of the range of concepts associated with positive mental health: hedonic and eudemonic aspects, positive affect, satisfying interpersonal relationships, and positive functioning.
Mindfulness
The 24-item Short Form of the Five Facet Mindfulness Questionnaire (FFMQ-SF) [21] is a valid and reliable alternative to the original FFMQ [22]. The FFMQ-SF can be divided into five facets: observing, describing, acting with awareness, non-judging of inner experiences, and non-reactivity to inner experiences. We used the total score.
Self-compassion
The 12-item Short Form of the Self-compassion Scale (SCS-SF) [23] is a reliable and valid alternative to the original SCS [24]. The SCS-SF can be divided into six subscales: self-kindness versus self-judgment, common humanity versus isolation, and mindfulness versus over-identification. We used the total score.
Qualitative assessments: Focus groups and interviews
To explore how patients experience participating in MBSR at different stages of their disease, focus groups and semi-structured individual interviews were used. The MBSR groups existed of a mixed group of breast cancer patients who participated both during and after anticancer treatment. Patients participated in MBSR for breast cancer patients only and they were invited for a focus group interview with their fellow participants 1 week after completion of the training.
Participants were asked the following question: “You participated in the MBSR training while you are in a certain treatment stage for breast cancer. How was it to participate is this stage you are in?” Focus groups took place at the Radboud Centre for Mindfulness 1 week after completion of MBSR, and lasted 100–120 min. Four focus groups were led by a psychiatrist and qualified mindfulness teacher (AS), and one focus group was conducted by a psychologist and qualified mindfulness teacher (EJ). Both interviewers had not been involved in teaching the MBSR training. The individual interviews were also conducted by EJ, by telephone, or face-to-face, and lasted 30–60 min. Focus groups and individual interviews started by explaining confidentiality and the explorative nature of the interview. Questions were asked in an open non-directive manner, allowing participants to speak freely about their experiences. For previous analyses on this qualitative data regarding the experience of peer support, see Schellekens et al. [25].
Quantitative data analysis
Repeated measures ANOVAs were used to examine differences between baseline and post-treatment scores. To examine whether the timing of the intervention (during or after anti-cancer treatment) is a moderator of the intervention, we added Timing as a between subjects factor and examined the corresponding interaction. In addition, we controlled the analysis for covariates (i.e., age, marital status, education, employment).
Qualitative data analysis
The focus group and individual interviews were audio-taped and transcribed verbatim. A summary was returned to the participants for a member-check. Data analysis started after the first focus group had been transcribed, and continued with each additional focus group. Two researchers (EJ and MS, behavioral scientist and mindfulness teacher in training) coded the transcripts independently. After three focus groups, the codes were compared by three researchers (MS, EJ, and AS) until consensus was reached. This led to the identification of several themes. After five focus groups and three semi-structured individual interviews, saturation was reached. Four researchers MS, EJ, AS, and EB (psychiatrist and qualified mindfulness teacher) eventually grouped the subthemes into themes, in order to derive hypotheses from the data. After data analysis, relevant quotes were translated into English.
Results
Study sample
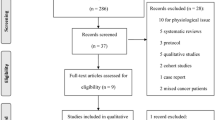
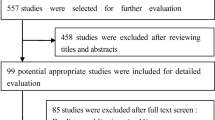
In total, 90 patients were recruited of whom 1 was excluded because she suffered from ovarian cancer. Of the 89 eligible patients, 64 (71%) participated (see Fig. 1 for study flow). As can be seen, the main reasons for declining participation were distance to the centre, scheduling conflicts, and participation in other psychological interventions.
The demographic and clinical characteristics of the 64 patients who started with MBSR are shown in Table 1. Of those who started, ten (16%) dropped out during the intervention. Patients who dropped out did not differ from those who completed the MBSR program. Main reasons for dropout were fear of fellow patients and physical impairments (see Fig. 1).
Effects of MBSR
After MBSR, participants reported significantly less psychological distress (p = 0.03, d = 0.44). In addition, significant improvements were found in mindfulness skills (p = 0.01, d = 0.48), self-compassion (p = 0.00, d = 0.6), wellbeing (p = 0.03, d = 0.31), and physical (p = 0.06, d = 0.40) and emotional quality of life (p = 0.01, d = 0.38) (see Table 2). No significant improvement was found in rumination or global quality of life (all p values >.05). Timing of treatment did not moderate the outcomes, except for mindfulness. Those patients participating after anti-cancer treatment reported a larger increase in mindfulness skills than those participating during anti-cancer treatment, possibly because those participating after anti-cancer treatment reported a lower baseline score of mindfulness skills. When adding Timing of intervention to the analysis, the effects on emotional functioning (p = 0.11) and wellbeing (p = 0.18) were no longer significant. Controlling for baseline variables, age, marital status, education, and employment did not change the results.
Qualitative results
Thirty-seven patients who participated in MBSR solely for breast cancer patients participated in the focus groups. Each focus group varied from 7 to 13 participants. Overall, 12 women participated during treatment and 25 participated after treatment. They were randomly divided over the focus groups. One palliative patient was interviewed individually, because she was not able to join the group. Two patients who participated with their partner in the group for mixed cancer patients were also interviewed individually. Both participated in MBSR during their anti-cancer treatment. The analysis of the five focus groups and three individual interviews resulted in three main themes: MBSR during cancer treatment, MBSR after cancer treatment, and Participation in relation to emotional processing. These themes could be subdivided into seven subthemes (see Table 3). Patients experienced several advantages and disadvantages when participating in MBSR during and after medical treatment. Besides the treatment stage, emotional processing also seemed an important indicator of the most suitable time to enroll.
Theme 1. Participation during anticancer treatment
MBSR supports coping with anticancer treatment
Many patients benefited from MBSR during treatment, which mainly consisted of chemotherapy but also long-term hormone treatment. They noted that what they learned during MBSR was immediately applicable to coping with their anticancer treatment. For instance, the training program in itself helped participants deal with their aversion to aspects of the somatic treatment.
You can apply it immediately, when you want to actively use it and if you need to learn to live in the moment especially, then it’s immediately useful. Then maybe your ideas about that therapy change.
Physical challenges
Several patients, however, were physically challenged to participate during their somatic treatment due to their illness and side-effects of the treatment. Participants mentioned that somatic symptoms or fatigue hindered attendance of the MBSR sessions and home practice. Others described how their somatic treatment schedule limited their time to participate.
Every three weeks I had chemo, so I was there on and off, I also missed two sessions because I really felt ill.
At the same time, a few patients mentioned that they had plenty of time during somatic treatment and that they were able to handle it physically.
Theme 2. Participation after anticancer treatment
Physically stronger
The physical challenges experienced during treatment were not mentioned by participants who participated after treatment. In this phase, participants experienced their physical recovery as being facilitating. Patients had gained energy, felt physically stronger, and generally had a better physical condition. In turn, patients felt they also gained energy from participating in the MBSR.
So some time needs to pass, and then you have a little bit of energy and then with the training, you get the rest of the energy
Too late to benefit
Participants noted that several months after treatment, they already experienced and coped with the fear and insecurities of diagnosis and treatment. They felt it was too late to fully benefit from the training and would have wanted to participate earlier. As one participant noted, she would have been able to move out of her survival mode much sooner. Others described they might have achieved more “clarity and peace” if there had been an opportunity to follow the training earlier, especially regarding work reintegration issues.
I think in that stage I.. in that stage when I tried to get back to work and get on with daily life, it would have clarified things for myself and it would have brought me some rest
Theme 3. Participation in relation to emotional processing
Coping with emotions
The participants noted that the timing of participation also depended on the willingness to emotionally engage with the MBSR, regardless of the treatment phase they were in. The need for psychological help depended on the degree of vulnerability patients allowed themselves to feel.
Are you okay with vulnerability or are you someone who says: no, I don’t want this. That’s what it depends on very much, I think.
Early empowerment
Participants mentioned the value of being able to make their own decision about whether and when to take part. They preferred to be informed about MBSR as soon as possible in order to do so. It seemed to strengthen the sense of autonomy in patients.
You’re in the hospital regularly anyway, they could address it sooner. Then you can decide for yourself, well it’s too early for me or oh, I would like that
Participation too early
A possible barrier of being informed about the MBSR training at an early stage is that patients may participate too early to fully benefit from the program. Some patients mentioned they were not emotionally prepared to participate, they felt too vulnerable to become aware of their thoughts and feelings.
I wanted something quickly, but in hindsight I think it might have been better to start a little bit later. Seeing what the chemo did to me, particularly mentally.
Discussion
This mixed method study explored what patients experience as a suitable stage to participate in MBSR. Our quantitative findings confirmed previous studies in showing that in the whole group of breast cancer patients MBSR resulted in a reduction of psychological distress [8, 9]. The quantitative data showed that participating during or after anticancer treatment interacts with changes in mindfulness. Those participating after anticancer treatment seem to improve more; however, this could possibly be explained by lower baseline scores. The qualitative data revealed that although participating in MBSR during anticancer treatment helped patients to cope with the treatment, their physical symptoms could also hinder participation. After anticancer treatment, their gain in energy facilitated participation in MBSR, but some patients mentioned they participated too late to fully benefit. Finally, in addition to the cancer treatment phase, right timing also seemed to depend on the stage of emotional processing. Women emphasized the importance of being informed about the possibility to take part in MBSR at an early stage as it enabled them to decide for themselves whether and when to enroll. These qualitative findings are in line with former studies showing that patients would like to be offered psychological interventions soon after diagnosis [26,27,28]. A recent meta-analysis showed that the sooner after diagnosis psychological help was offered, the higher the uptake [14].
Nevertheless, a large part of cancer patients decline help, despite being distressed. Patients seem to believe that one’s level of distress is not severe enough to warrant psychosocial interventions and prefer to manage on their own, even in the subgroup with high levels of distress [29].When psychosocial care becomes more integrated into regular cancer care, psychosocial interventions such as MBSR might become more acceptable and accessible for patients. However, as health care professionals focus on physical symptoms and treatment, emotional and psychological symptoms are often overlooked. Health care professionals also report lack of time and lack of confidence as barriers to address psychological symptoms [30]. Patients may be embarrassed or reluctant to mention their psychological problems to their physician [31]. Offering psychosocial help soon after diagnosis and providing clear information about the different options, such as MBSR, to all patients might be a first step. It might contribute to the patients’ autonomy and self-management skills at a moment when they are deprived of these in many ways.
Strengths and limitations
Breast cancer patients with different disease and treatment stages were all welcome to participate, enabling us to explore how women experienced the timing of participating in MBSR. Quantitative findings were presented with qualitative findings to provide an overview of the effects and experiences of MBSR participation. As a relatively large sample of breast cancer patients participated in the focus groups, we reached data saturation and reported on a broad view of experiences. We also performed member-checks, ensuring the interpretation of the data was valid. The study also has a number of limitations. The focus groups were mixed, in line with the mixed group of patients (both during and after anticancer treatment) participating in the intervention. For the aim of this study, we might have gained more specific information about timing of the intervention, by interviewing them separately. The quantitative results were uncontrolled; we did not carefully register all psychosocial treatments participants might have been using. Most of our patients were in a curative stage. In addition, the women who dropped out the intervention were not invited to the focus groups or individual interviews. Although these women provided reasons for dropping out (i.e., fear of fellow patients and physical impairments), unfortunately they did not provide information on how they experienced the time of enrollment and whether the stage of anticancer treatment might play a role in dropping out the intervention.
Clinical implications and further research
Several factors should be taken into account when helping breast cancer patients interested in MBSR to time their participation. To stimulate patients’ self-management, information on MBSR should be provided in an early stage. This can help patients to decide for themselves when they are emotionally ready to participate. Health care professionals should be alert on those women who ‘rush into it’ as they might still be too vulnerable to become mindfully aware of their thoughts, emotions, and bodily sensations. Capability building strategies for health care professionals might support them addressing these issues with patients [32]. Patients should also be informed about how physical symptoms can hinder participation, especially during anticancer treatment.
Depending on women’s’ physical symptoms, participation in MBSR can be experienced as beneficial both during and after anticancer treatment. Future research could examine whether participation during and after anticancer treatment is equally feasible and effective for women with breast cancer. Additionally, it would be interesting to study whether these results extend to cancer patients with a higher symptom burden (e.g., lung cancer). Alternatively, future studies could further explore whether tailored version of the MBSR program, such as online or blended versions, might make MBSR more accessible for patients currently undergoing anticancer treatment [33].
References
Ferlay J et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386
Henselmans I et al (2010) Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychol 29(2):160
Mitchell A, Ferguson D, Gill J, Paul J, Symonds P (2013) Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol 14(8):721–732
Meyer TJ, Mark MM (1995) Effects of psychosocial interventions with adult cancer patients: a meta-analysis of randomized experiments. Health Psychol 14(2):101–108
Osborn RL, Demoncada AC, Feuerstein M (2006) Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta-analyses. Int J Psychiatry Med 36(1):13–34
Goedendorp MM et al (2009) Psychosocial interventions for reducing fatigue during cancer treatment in adults. Cochrane Database Syst Rev 21(1):CD006953
Kabat-Zinn J (1990) Full catastrophe living: using the wisdom of your body and mind in everyday life. Delacorte, New York
Cramer H et al (2012) Mindfulness based stress reduction for breast cancer—a systematic review and meta analysis. Curr Oncol 19(5):e343–e352
Piet J, Wurtzen H, Zacharea R (2012) The effect of mindfulness based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: a systematic review and meta-analysis. J Consult Clin Psychol 80(6):1007–1020
Henderson VP et al (2012) The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: a randomized trial. Breast Cancer Res Treat 131(1):99–109
Lengacher CA et al (2009) Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology 18(12):1261–1272
Hoffman CJ et al (2012) Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: a randomized, controlled trial. J Clin Oncol 30(12):1335–1342
Carlson LE et al (2013) Randomized controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer (MINDSET). J Clin Oncol 31(25):3119–3126
Brebach R et al (2016) Psychological intervention targeting distress for cancer patients: a meta-analytic study investigating uptake and adherence. Psycho-Oncology 25(8):882–890
Schellekens MP et al (2014) Study protocol of a randomized controlled trial comparing mindfulness-based stress reduction with treatment as usual in reducing psychological distress in patients with lung cancer and their partners: the MILON study. BMC Cancer 14:3
Crane RS et al (2012) Competence in teaching mindfulness-based courses: concepts, development and assessment. Mindfulness 3(1):76–84
Spinhoven P et al (1997) A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subject. Psychol Med 27(2):363–370
Raes F et al (2009) Reflection en “brooding”als subtypes van het rumineren: een herziening van de Ruminative Response Scale. Gedragstherapie 42:205–214
Bjordal K et al (2000) A 12 country field study of the EORTC QLQ-C30 (version 3.0) and the head and neck cancer specific module (EORTC QLQ-H&N35) in head and neck patients. EORTC Quality of Life Group. Eur J Cancer 36(14):1796–1807
Stewart-Brown S et al (2009) Internal construct validity of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS): a Rasch analysis using data from the Scottish health education population survey. Health Qual Life Outcomes 7:15
Baer RA, Smith GT, Lykins E (2008) Construct Validity of the Five Facet Mindfulness Questionnaire in Meditating and Nonmeditating Samples. Assessment 15(3):329–342
Bohlmeijer ET, ten Klooster P, Fledderus M, Veehof MM, Baer R (2011) Psychometric properties of the Five Facet Mindfulness Questionnaire in depressed adults and development of a short form. Assessment 18(3):308–320
Raes F et al (2011) Construction and factorial validation of a short form of the Self-Compassion Scale. Clinical Psychology & Psychotherapy 18(3):250–255
Neff C (2003) The development and validation of a scale to measure self-compassion. Self Identity 2(3):223–250
Schellekens MP et al (2016) A qualitative study on mindfulness-based stress reduction for breast cancer patients: how women experience participating with fellow patients. Support Care Cancer 24(4):1813–1820
Shapiro PJ, Coyne JC, Kruus LK (2004) Interest in services among prostate cancer patients receiving androgen deprivation therapy. Psycho-Oncology 13(8):512–525
Allen SM, Shah AC, Nezu AM (2002) A problemsolving approach to stress reduction among younger women with breast carcinoma: a randomized controlled trial. Cancer 94(12):3089–3100
Arving C, Sjoden PO, Bergh J (2006) Satisfaction, utilisation and perceived benefit of individual psychosocial support for breast cancer patients—a randomised study of nurse versus psychologist interventions. Patient Educ Couns 62(2):235–243
Clover KA et al (2014) Why do oncology outpatients who report emotional distress decline help? Psycho-Oncology 24(7):812–818
Maguire P (1999) Improving communication with cancer patients. Eur J Cancer 35(10):1415–1422
Valente SM, Saunders JM, Cohen MZ (1994) Evaluating depression among patients with cancer. Cancer Pract 2(1):65–71
Dilworth S, Higgins I, Parker V, Kelly B, Turner J (2014) Patient and health professional’s perceived barriers to the delivery of psychosocial care to adults with cancer: a systematic review. Psycho-Oncology 23(6):601–612
Compen FR, Bisseling EM, Van der Lee ML, Adang EMM, Donders ART, Speckens AEM (2015) Study protocol of a multicenter randomized controlled trial comparing the effectiveness of group and individual internet-based mindfulness-based cognitive therapy with treatment as usual in reducing psychological distress in cancer patients: the BeMind study. BMC Psychology 3:27
Acknowledgments
This research was funded by the funding agency for breast cancer Pink Ribbon. We would like to thank Rinie van den Boogaart for teaching the MBSR classes and Rhoda Schuling for translating the quotes.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bisseling, E.M., Schellekens, M.P., Jansen, E.T. et al. Mindfulness-based stress reduction for breast cancer patients: a mixed method study on what patients experience as a suitable stage to participate. Support Care Cancer 25, 3067–3074 (2017). https://doi.org/10.1007/s00520-017-3714-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3714-8