Abstract
ᅟ
There is little evidence regarding primary healthcare team members’ perceptions concerning palliative care consultation team (PCCT) and palliative care (PC) issues on their own wards.
Purpose
This study aimed to study whether a PCCT can influence and change primary healthcare team members’ perceptions regarding the palliative care at the end of life they are providing to patients in their own acute wards.
Methods
The intervention was a PCCT visiting surgical and internal medicine wards in 1 year. We used a quasi-experimental design with pre-post-testing, measuring at baseline, and after 1 year’s intervention. A questionnaire was answered by all primary healthcare team members in three acute wards.
Results
A total of 252 team members (pre-post-intervention n = 132/n = 120) participated in the study. Overall, 11 of the 12 statements scored significantly higher after the intervention than before. Responses varied significantly between different professions and depending on the number of dying patients cared for during the last month. The five with the highest Wald values were as follows: the presence of a break point dialogue with a patient, where the changed aim and focus of care was discussed; early detection of impending death; adequate symptom relief and psychological and existential issues.
Conclusion
It is possible to change perceptions about end-of-life care in primary healthcare team members on acute wards. Palliative care consultation teams should be a natural part wherever dying patients are cared for.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Palliative care (PC) has its own definition according to the WHO [1] and is suitable when a patient has a serious, long-lasting disease or a life-threatening disease or is at the end of life. PC services in many countries have developed to include inpatient care, home care, community care and acute hospital consultancy care to enable access to PC principles across most healthcare settings in order to meet the complex needs of patients and families. In some countries, PC services have rapidly been developed and implemented [2–4]; e.g. in Japan, 99 % of the country’s regional cancer centres had some kind of palliative care consultation teams (PCCTs). Studies from California reported that 44 % (n = 141) of California hospitals had a PC program [4] in 2007, but in 2011, the expansion of these programs had stopped increasing [5]. The most common type of PC service in California was an inpatient consultation team. Members in PCCT may differ and might include only physicians or nurses/nurse practitioners, or both, sometimes augmented with another profession [2, 4–9].
When introducing PCCT, patients’ symptom relief has been improved [10, 11]; a significant decrease was observed for pain, nausea, depression, anxiety and somnolence as well as in the number of uncontrolled symptoms and in the symptom distress score [10, 12, 13]. The patients’ perception of their general well-being and satisfaction with their care experience had also improved [12, 14]. Although most studies suggest that patients benefit from PC, there are studies reporting no differences/improvements in symptom scores [14, 15]. In addition, PCCTs are reported to be up-to-date “do not resuscitate/do not intubate” orders and up-to-date comfort care orders, and that patients were referred for hospice care [10, 16], but less admitted to, or to die in intensive care units [14, 17–19]. The recommendations provided by the PCCT were implemented in 88–90 % of cases by the primary team [10]. PCCTs also seem to be cost effective, compared to match controls without PCCT; PC cases in hospitals had a significantly lower cost per day, ranging from US$279 to US$464/day [10, 18–20].
Unmet PC needs among dying patients in hospitals have also been identified [21]. It is also known that team members in settings other than specialised PC might not prioritise PC, do not recognise PC team competencies or are uninterested in PC competencies [21, 22]. Sometimes, acute care and PC are described as different incompatible cultures, with contrasts and contradictions [23]. It is therefore a delicate didactic question whether it is possible for PC competencies to influence the acute care culture and its perceptions about PC. Another question is whether it is possible to improve primary healthcare team members by educating them to handle PC issues better.
There is little evidence regarding primary healthcare team members’ perceptions concerning PCCT and PC issues on their own wards. The available studies report that PCCTs are expected by primary healthcare team members to be experts in managing difficult symptoms and complex psychosocial problems, in communication and emotional support and to clarify care goals [3, 8, 11, 14]. In one survey, more than 90 % of the primary team member respondents considered the effect of the PCCT as excellent or good and were satisfied with the support provided [15]. Primary healthcare team members concluded that PCCT should be visible in the wards, be responsive and be easily accessible [24]. However, conflicting results were also identified; in particular, whether specialists should be providing generalist PC (such as basic psychological support) that was neglected by ward teams, as well as conflicts about the implementation of specialist advice by referrers. These results, on the borders between generalist and specialist provision, provide insights into the different care cultures [24].
Based on the previously mentioned research [24], and the fact that there are few reports on PCCT impacts on staff perception [25] about PC in their own settings, our study focuses on the impact PCCTs might have to change primary healthcare team members’ perceptions about PC offered to patients at their own unit. The current study reports quantitative results from a larger study, where the focus has been to implement PCCT on internal medicine and surgical wards. Although there is evidence about the benefits and effectiveness of PCCT, this study will focus on whether primary healthcare team members perceive that the PC at the end of life they are providing on their wards has changed since the implementation of a PCCT, with regard to communication, patient symptoms, family support, documentation, planning and teamwork in their daily care practise after 1 year’s intervention. We also wanted to study if profession, years of working experience and caring experience of dying patients influenced the participants’ responses. Has the intervention changed the quality of the PC at the end of life provided according to primary healthcare team members’ perceptions? Our hypothesis is that this intervention will positively change primary healthcare team members’ perceptions about the PC they are providing to patients in their own wards. This hypothesis is based on Dewey’s theory [26, 27] that learning is a social and interactive process, where experience and knowledge are intertwined and developed together.
Methods
Design
A quasi-experimental design, with pre-post-comparisons, was used.
Setting
One county in the southeast of Sweden (population approx. 400,000) was chosen. A request from the governing politicians in this county is that high-quality PC should progressively become available to the wider intended group, regardless of where the care is given [28]. The target group in this study was primary healthcare team members on one acute internal medical ward and two surgical wards of a local hospital, where general internal medicine patients (cancer, lung diseases, kidney diseases) and general surgical patients (cancer, GI diseases, urological) in all phases of their disease were cared for. Primary healthcare team members in the wards were nurses, assistant nurses, physicians and physiotherapists and had basic skills in PC [29, 30].
The intervention
The intervention was developed by a regional multidisciplinary team, designed with the purpose of enabling the primary healthcare team members to make positive changes in their clinical practise and the PC they provided in acute wards. An integrative bedside education approach was used, where physicians and nurses specialised in PC and with long experience in PC tried to embed PC principles and interventions into daily practise. PCCT visited the wards and were available between 1 and 8 h/week in 1 year (m = 6.5 h/week), taking part in reports, rounds and communications, with the aim of educating primary healthcare team members in PC. Specific aims were to highlight physical, psychological, social and existential needs in dying patients on the local wards (WHO) by educating primary healthcare team members in the areas of symptom management, improved communication skills and the provision of support to patients and family members, as well as identifying patients at risk for poor outcomes, who may benefit from a PC consultation. PCCT supported primary healthcare team members for example when communicating with patients. The primary team could also ask for specific education for all team members in the wards. Education in PC philosophy, pain management and mouth care were provided (total 48 h). The pedagogical idea was inspired by Dewey [26, 27], who claims that experience and knowledge are intertwined and developed together. Knowledge should be gained in social processes together with others, and he emphasises changes without causing commotion. When integrating new knowledge and comparing it with reality and its consequences, people reconstruct their picture of reality. Participants need to be introduced to the problem, discuss it, argue, negotiate and agree on a solution. Another important aspect in this pedagogical mindset is the evaluation, in the current study, after trying a new way of working. The intervention continued during the course of 1 year.
Sampling and data collection
One hospital where a PCCT was available was chosen. The project was assessed as being a quality improvement project, and the head for each clinic approved the research ethics for this study. All primary healthcare team members on duty in one particular week were asked to participate and anonymously answer a questionnaire. The study was carried out in accordance with the code of ethics of the Declaration of Helsinki: team members were informed orally and in writing about the voluntariness, of their right to refuse to participate in the study or to withdraw consent to participate at any time without reprisal. Data were collected in 2010–2012.
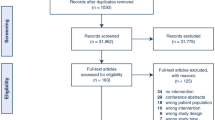
Inclusion criterion for participants was being a primary healthcare team member caring for dying patients in an acute ward. The participants completed a questionnaire at baseline and then again after 1 year of ongoing intervention. For the flowchart, see Fig. 1.
As there was no available questionnaire that covered the area in this study, one was constructed by the authors to capture the aim of the intervention, mainly based on the WHO definition of PC, and addressed primary healthcare team members’ perceptions regarding PC at the end of life that they provided to patients on their own ward. In the questionnaire, five questions concerned the team members’ sociodemographic data and one question was about their interest in PC at the end of life. The next 12 questions were statements concerning a number of areas, including communication and break point dialogue; i.e. a communication between the physician or attending physician responsible and the patient about the stance transition to PC at end of life, where the content of the continued care is discussed based on the patient’s condition, needs and desires [31]. This was followed by statements on symptoms, family support, documentation, planning and teamwork. Each statement started with, “On our ward there is…”, with examples about communication, teamwork etc., in order to capture team members’ own perceptions of the PC at the end of life they were providing themselves in their wards (Likert scale ranging from never (1) to always (6)) (see Table 4). The following is an example of how the questions were formulated: “on our ward patients in palliative end-of-life care are given adequate symptom relief”. Higher scores indicate more favourable responses.
To achieve content validity of the questions, the items were critically discussed among two physicians, two nurses and two researchers (all PC specialists) in order to evaluate the appropriateness and the understanding of the questions. These persons were chosen because they had experience in both specialised PC and PC in acute wards. Only small changes were suggested. The numbers of missing values among the participants were generally small, ranging from 2 to 9 % (statements of family support/bereavement follow-up).
Analysis
Descriptive statistics were calculated for the individual variables. Statistical tests were performed by Fisher’s exact test, T test (non-paired, paired), the Wilcoxon rank-sum test and the McNemar test, where appropriate.
As the responses were on a Likert scale, i.e. ordinal multinomial in nature, data were analysed using generalised linear models, regression analyses with ordinal multinomial distribution and logit link and presented as Wald values. We conducted two different analyses, using the responses to each one of the 12 statements. First, we analysed the responses as affected by time (baseline vs after 1 year), profession (MD, nurse, assist. nurse), “years of experience working in healthcare” and “number of patients”. Secondly, we analysed responses as affected by time (T), profession (O) and their interaction term (T × O) and, based on the outcome, plotted relevant data. P values <0.05 were considered to be significant. All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS, version 20; IBM, USA) and STATISTICA (StatSoft Inc. STATISTICA version 10.0. Tulsa, USA).
Results
Study population
Background data for the 252 participants (baseline n = 132/post-intervention n = 120) who comprise the study sample are presented in Table 1. Response rate at baseline was 78 % and after the intervention 85 %. Participating females were 89/86 %, and the largest professional group was the nurses 54/63 %. No significant differences were found between participants’ sociodemographic data from baseline compared to those participating after 1 year.
Profession and working experience
Overall, 11 of the 12 statements regarding primary healthcare team members’ perceptions of PC at the end of life at their own ward scored significantly higher after the intervention than before (Table 2). For 9 of the 12 questions, responses varied significantly among professions and depending on number of dying patients cared for during the last month. The five with highest Wald values were break point dialogue (35.62; P < 0.001); early detection of impending death (28.09; P < 0.001); a properly functioning teamwork (25.99; P < 0.001); adequate symptom relief (20.78; P < 0.001) and psychological and existential issues (19.20; P < 0.001) (Table 2). In contrast, “years of working experience” was insignificant (Table 2). Regarding the “number of dying patients cared for during the last month”, the highest Wald values were available bereavement follow-up (26.43; P < 0.001); adequate symptom relief (17.01; P < 0.001) and a properly functioning teamwork (16.01; P < 0.001).
As “profession” had such a profound effect, we then ran separate analyses of time and profession. In these analyses, no question had a significant interaction (Table 3), i.e. team members with different “professions” do not perceive changes differently. In these models, which did not account for “number of dying patients cared for the last month”, 8 of 12 questions scored a significant increase after intervention and 5 of these stand out with large Wald values: planning discharge of patients (15.09; P < 0.001), the overall question about good quality in end-of-life care (14.34; P < 0.001), break point dialogue (13.95; P < 0.001), support (13.53; P < 0.001) and communication (11.64; P < 0.001) (Table 3). The profession-wise change in response was invariably in the positive direction (Fig. 2).
Average (95 % confidence intervals) of profession-wise change of responses before and after intervention. ##Break point dialogue: a communication between the physician or attending physician responsible and patient (family member) about the stance transition to palliative care at end of life, where the content of the continued care is discussed, based on the patient’s condition, needs and desires [31]
Pre-post-analysis—total population
In the whole population, there were significant differences in 8 of the 12 statements. The highest levels of significance were found in two statements—“the presence of good quality of communication with patients and their family members” (t = −3.09; P < 0.001) and in the overall question, “presence of good quality in end-of-life care” (t = −3.54; P < 0.001). No significant change was seen for adequate symptom relief (Table 4).
Discussion and conclusion
Discussion
This study showed that a palliative intervention based on Dewey’s theory can change primary healthcare team members’ perceptions, and also their own PC practises, at the end of life in several areas. This means that part of our hypothesis was confirmed. However, the increase was not that high in all areas, for example the interest in PC at the end of life did not change but was initially quite high. In the current study, the communication areas had increased the most, namely break point dialogues and overall communication. Recently, a systematic review explored the current evidence for communication interventions at the end of life and reported that the length of training could range from 3 h to 4 days, but that no consistent relationship between length of training and efficacy was apparent [32]. Communication is an important area in PC, irrespective of profession and in what setting the patient is cared for. There have been many suggestions regarding how to improve communication skills in the end-of-life context but not so many interventional studies with strong research designs; only 17 % of healthcare professional interventions were evaluated in RCTs [32]. Some studies with a similar design to the current study have shown increased confidence in end-of-life care communication, although with quite different efforts to improve the skills of both nurses [33] and physicians [32, 34, 35]. One study [36] concluded that all training enhances skills, but it may only have a minor effect on clinical practise. Instead, these authors highlighted the role of clinical supervision to enhance the clinical effectiveness of communication skills. We agree with this, as it was one of the reasons for providing education in the clinicians’ own area, i.e. carrying out bedside education with a pedagogical theory behind. When they are in their own area, it seems possible to influence thoughts and perceptions by emphasising these issues at the moment they are present. The current study has not only focused on communication but also on other topics, for example symptoms, support, documentation and psychological and existential issues. Previous communication interventions have had their main target in oncology settings [32], while this study has a wider focus, on both surgical and internal medicine wards, where the team members are not only specialised in cancer patients. That makes this study unique and a contribution to the existing knowledge in the field.
One can ask what makes an intervention successful. Recently, a narrative literature synthesis [37] concluded that collaboration between different healthcare teams is fostered when each team recognises and supports the expertise of the other. Effective communication between the different healthcare teams, determination of complementary roles and responsible and mutual problem-solving are facilitators of collaboration. This study might be a sign of this, but as we did not measure collaboration specifically, we cannot say what contributed to the positive results of this study. For this, further evidence is needed.
The present study also showed a significant change regarding psychological and existential issues. Another study [38] used theoretical training in existential issues combined with group reflection to achieve greater understanding and communicative confidence when caring for patients dying of cancer. That study showed a significant increase in the training group, even after 6 months, compared to the non-training group. The psychological and existential areas might be hard to impact through a unidirectional old-fashioned lecture as it needs practise. According to the current study, PCCT presence when these issues arise seems to influence primary healthcare team members’ perception in a positive direction. This was also the idea of using Dewey’s pedagogical theory, trying to reconstruct participants’ reality by integrating new knowledge and comparing it with their actual clinical reality. When, for example, death anxiety occurs, it is possible to discuss different ways of managing this and different consequences, for example by a phone call to PCCT.
It is easy to assume that years of working experience should influence the results positively, but in this study, working experience was unimportant for the responses. On the other hand, the experience of caring for a dying patient during the last months seems important. Again, this might be due to the idea of this intervention, i.e. the presence and support of consultants, in the moment when primary healthcare team members are caring for, are discussing with, examines or treats a dying patient. This attendance seems to positively influence their perceptions of their own work.
It is likely to question whether it is possible to measure changes in one’s own clinical experience. One suggestion might be to measure medical and nursing interventions documented in records. But, records do not always accurately reflect care, and the gap between what is written and what is done might be a bias [39]. Another suggestion is to make qualitative researcher observations like we did in another part of this study (manuscript not published yet).
This study has several flaws, as the questionnaire is not reliability and validity tested in full format, we could for example have tested the questionnaire on primary caregivers on acute wards. Furthermore, we did not use any randomisation or a control group, such as in an experimental design. In the current study, we chose a quasi-experimental design that is weaker than the experimental design but could also be a strength as it gives more flexibility to the wards. In further studies, the quantity should be specified, for example a “dose” of 5 h/week. But instead, we chose to adjust the amount of hours to suit the needs of the participants (1–8 h/week) at certain moments (rounds, reports). All these weaknesses have to be taken into account as they influence the possibility of generalising the results. Furthermore, we have not quantitatively evaluated how the PC end-of-life issues were actually performed, for example the “true” quality of a break point dialogue. For that, a qualitative study is needed. We can only express an opinion about that the participants’ perceived a positive change.
Conclusion
Our hypothesis that a palliative bedside intervention based on Dewey’s theory can change primary healthcare team members’ perceptions was partly confirmed. Short involvement from PCCT can influence primary healthcare team members to provide appropriate general PC at the end of life. However, more evidence is needed, preferably with RCTs or in-depth qualitative studies and in non-cancer populations. PCCT should be a natural part wherever dying patients are cared for, as the changed perceptions among primary team members might positively influence a high-quality PC at the end of life for patients and their families.
References
World Health Organization (2015) WHO definition of palliative care. Available from: http://www.who.int/cancer/palliative/definition/en/. Accessed 16 Sept 2016
Nakazawa Y, Miyashita M, Morita T, Misawa T, Tsuneto S, Shima Y (2012) The current status and issues regarding hospital-based specialized palliative care service in Japanese regional cancer centers: a nationwide questionnaire survey. Jpn J Clin Oncol 42:432–441
Kamal A, Swetz K, Carey E, Cheville A, Liu H, Ruegg S, et al. (2011) Palliative care consultations in patients with cancer: a mayo clinic 5-year review. J Oncol Pract 7:48–53
Pantilat S, Kerr K, Billings J, Bruno K, O’Riordan D (2012) Palliative care services in California hospitals: program prevalence and hospital characteristics. J Pain Symptom Manag 43:39–46
Pantilat S, O’Riordan D, Bruno K (2014) Two steps forward, one step back: changes in palliative care consultation services in California hospitals from 2007 to 2011. J Palliat Med 17:1214–1220
Nelson C, Chand P, Sortais J, Oloimooja J, Rembert G (2011) Inpatient palliative care consults and the probability of hospital readmission. Perm J 15:48–51
Norton S, Powers B, Schmitt M, Metzger M, Fairbanks E, Deluca J, et al. (2011) Navigating tensions: integrating palliative care consultation services into an academic medical center setting. J Pain Symptom Manag 42:680–690
Casarett D, Pickard A, Bailey F, Ritchie C, Furman C, Rosenfeld K, et al. (2008) Do palliative consultations improve patient outcomes? J Am Geriatr Soc 56:593–599
Pantilat S, Kerr K, Billings J, Bruno K, O’Riordan D (2012) Characteristics of palliative care consultation services in California hospitals. J Palliat Med 15:555–560
Hanson L, Usher B, Spragens L, Bernard S (2008) Clinical and economic impact of palliative care consultation. J Pain Symptom Manag 35:340–346
Pantilat S, O’Riordan D, Dibble S, Landefeld C (2010) Hospital-based palliative medicine consultation: a randomized controlled trial. Arch Intern Med 170:2038–2040
de Santiago A, Portela M, Ramos L, Larumbe A, Urdiroz J, Martínez M, et al. (2012) A new palliative care consultation team at the oncology department of a university hospital: an assessment of initial efficiency and effectiveness. Support Care Cancer 20:2199–2203
Laguna J, Goldstein R, Allen J, Braun W, Enguídanos S (2012) Inpatient palliative care and patient pain: pre- and post-outcomes. J Pain Symptom Manag 43
Gade G, Venohr I, Conner D, McGrady K, Beane J, Richardson R, et al. (2008) Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med 11:180–190
Sasahara T, Miyashita M, Umeda M, Higuchi H, Shinoda J, Kawa M, et al. (2010) Multiple evaluation of a hospital-based palliative care consultation team in a university hospital: activities, patient outcome, and referring staff’s view. Palliat Support Care 8:49–57
O’Mahony S, Blank A, Zallman L, Selwyn P (2005) The benefits of a hospital-based inpatient palliative care consultation service: preliminary outcome data. J Palliat Med 8:1033–1039
Morrison R, Dietrich J, Ladwig SEA, et al. (2011) Palliative care consultation teams cut hospital costs for Medicaid beneficiaries. Health Aff (Millwood) 30:454–463
Penrod J, Deb P, Dellenbaugh C, Burgess JJ, Zhu C, Christiansen C, et al. (2010) Hospital-based palliative care consultation: effects on hospital cost. J Palliat Med 13:973–979
Penrod J, Deb P, Luhrs C, Dellenbaugh C, Zhu C, Hochman T, et al. (2006) Cost and utilization outcomes of patients receiving hospital-based palliative care consultation. J Palliat Med 9:855–860
Morrison R, Renrod J, Cassel J, Group. PCLCO, et al. (2008) Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med 168:1783–1790
Le BHC, Watt J (2010) Care of the dying in Australia’s busiest hospital: benefits of palliative care consultation and methods to enhance access. J Palliat Med 13:855–860
Rodriguez K, Barnato A, Arnold R (2007) Perceptions and utilization of palliative care services in acute care hospitals. J Palliat Med 10:99–110
Johansson K, Lindahl B (2012) Moving between rooms—moving between life and death: nurses’ experiences of caring for terminally ill patients in hospitals. J Clin Nurs 21:2034–2043
Ewing G, Farquhar M, Booth S (2009) Delivering palliative care in an acute hospital setting: views of referrers and specialist providers. J Pain Symptom Manag 38:327–340
Tallman K, Greenwald R, Reidenouer A, Pantel L (2012) Living with advanced illness: longitudinal study of patient, family, and caregiver needs. Perm J. 16:28–35
Dewey J (1938) Experience & education. Kappa Delta Pi, New York
Dewey J (1916) Democracy and education. Press N. Macmillan Company, New York
LänsSLAKO (2003) The future of palliative care in the county of Östergötland. Linköpings tryckeri AB, Linköping
The National Board of Health and Welfare (2015) Allmän palliativ vård (Swedish)—general palliative care. http://socialstyrelsen.iterm.se/showterm.php?fTid=481. Accessed 16 Sept 2016
Quill T, Abernethy A (2013) Generalist plus specialist palliative care—creating a more sustainable model. N Engl J Med 368:1173–1175
The National Board of Health and Welfare (2014) Brytpunktssamtal (break point dialogue). http://socialstyrelsen.iterm.se/showterm.php?fTid=748. Accessed 16 Sept 2016
Walczak A, Butow P, Bu S, Clayton J (2016) A systematic review of evidence for end-of-life communication interventions: who do they target, how are they structured and do they work? Patient Educ Couns 99(1):3–16. doi:10.1016/j.pec.2015.08.017
Wilkinson S, Perry R, Blanchard K, Linsell L (2008) Effectiveness of a three-day communication skills course in changing nurses’ communication skills with cancer/palliative care patients: a randomised controlled trial. Palliat Med 22:365–375
Feathers L, DeCaestecker S, Norrie P, Fowler J, Faull C (2014) Developing skills in communication in end of life care: evaluation of a 3 day pilot course for core medical training. Brit Med J Support Palliat Care 4(Suppl 1):2014 A38
Alexander S, Keitz S, Sloane R, Tulsky JA (2006) Controlled trial of a short course to improve residents’ communication with patients at the end of life. Acad Med 11:1008–1012
Heaven C, Clegg J, Maguire P (2006) Transfer of communication skills training from workshop to workplace: the impact of clinical supervision. Patient Educ Couns 60:313–325
Firn J, Preston N, Walshe C (2016) What are the views of hospital-based generalist palliative care professionals on what facilitates or hinders collaboration with in-patient specialist palliative care teams? A systematically constructed narrative synthesis. Palliat Med 30(3):240–256. doi:10.1177/0269216315615483
Henoch I, Danielson E, Strang S, Browall M, Melin-Johansson C (2013) Training intervention for health care staff in the provision of existential support to patients with cancer: a randomized, controlled study. J Pain Symptom Manag 46:785–794
Gunhardsson I, Svensson A, Berterö C (2008) Documentation in palliative care: nursing documentation in a palliative care unit—a pilot study. Am J Hosp Palliat Care 25:45–51
The National Board of Health and Welfare (2014) Brytpunkt (break point). http://socialstyrelsen.iterm.se/showterm.php?fTid=479. Accessed 16 Sept 2016
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author contributions
Design of the study: MF, YH, MJ, PM and AM. Analysis of the data: MF, PM and AM. Writing of the paper: MF, YH, MJ, PM and AM.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Friedrichsen, M., Hajradinovic, Y., Jakobsson, M. et al. Palliative care consultation team on acute wards—an intervention study with pre-post comparisons. Support Care Cancer 25, 371–380 (2017). https://doi.org/10.1007/s00520-016-3406-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3406-9