Abstract
Purpose
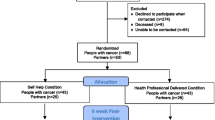
The primary objectives were (1) to examine the importance of sexuality within the self-view and cross-sectional correlates for 120 colorectal cancer patients and (2) to determine whether the importance of sexuality changed for 46 colorectal cancer patients and partners participating in an intimacy enhancement intervention.
Methods
Two newly developed items assessed importance of sexuality within the self-view (1) currently and (2) before cancer; a calculated change score assessed perceived change. In the cross-sectional sample, associations between importance of sexuality and demographic and medical factors and sexual function status were examined. Intervention participants’ importance ratings before and after participation were used to calculate effect sizes.
Results
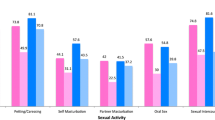
For patients, importance of sexuality before cancer was greater (M = 65.7) than current importance (M = 56.8, p = .001). Greater current importance of sexuality was associated with partnered status, non-metastatic disease, and not being in treatment. Scoring in the sexually functional range was associated with greater current importance of sexuality for men and a smaller perceived change in importance for both men and women (p values <.05). Sexual function status also significantly predicted current importance independent of covariates. Small to medium effect sizes for intervention patients (.37) and partners (.60) were found for increases in importance of sexuality. Items showed evidence of test-retest reliability and construct validity.
Conclusions
Coping with sexual concerns is important to those affected by colorectal cancer. Findings suggest that the importance of sexuality can decrease through colorectal cancer and associated sexual problems and can increase through participating in an intimacy-focused intervention.

Similar content being viewed by others
Notes
To be consistent with the bulk of analyses, these tests were conducted among partnered patients only.
References
Reese JB, Finan PH, Haythornthwaite JA, Kadan M, Regan KR, Herman JM, Efron J, Diaz LA Jr, Azad NS (2014) Gastrointestinal ostomies and sexual outcomes: a comparison of colorectal cancer patients by ostomy status. Support Care Cancer 22(2):461–468. doi:10.1007/s00520-013-1998-x
Traa M, De Vries J, Roukema J, Den Oudsten B (2012) Sexual (dys) function and the quality of sexual life in patients with colorectal cancer: a systematic review. Ann Oncol 23(1):19–27. doi:10.1093/annonc/mdr133
da Silva GM, Hull T, Roberts PL, Ruiz DE, Wexner SD, Weiss EG, Nogueras JJ, Daniel N, Bast J, Hammel J, Sands D (2008) The effect of colorectal surgery in female sexual function, body image, self-esteem and general health: a prospective study. Ann Surg 248(2):266–272. doi:10.1097/SLA.0b013e3181820cf4
Hendren SK, O’Connor BI, Liu M, Asano T, Cohen Z, Swallow CJ, Macrae HM, Gryfe R, McLeod RS (2005) Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg 242(2):212–223. doi:10.1097/01.sla.0000171299.43954.ce
Traa MJ, Orsini RG, Den Oudsten BL, De Vries J, Roukema JA, Bosman SJ, Dudink RL, Rutten HJ (2014) Measuring the health-related quality of life and sexual functioning of patients with rectal cancer: does type of treatment matter? Int J Cancer 134(4):979–987. doi:10.1002/ijc.28430
Angenete E, Asplund D, Andersson J, Haglind E (2014) Self reported experience of sexual function and quality after abdominoperineal excision in a prospective cohort. Int J Surg 12(11):1221–1227. doi:10.1016/j.ijsu.2014.10.003
Perz J, Ussher JM, Gilbert E (2014) Feeling well and talking about sex: psycho-social predictors of sexual functioning after cancer. BMC Cancer 14(1):228–247. doi:10.1186/1471-2407-14-228
Andersen BL, Carpenter KM, Yang HC, Shapiro CL (2007) Sexual well-being among partnered women with breast cancer recurrence. J Clin Oncol 25(21):3151–3157. doi:10.1200/JCO.2006.09.6958
Olsson C, Athlin E, Sandin-Bojo AK, Larsson M (2013) Sexuality is not a priority when disease and treatment side effects are severe: conceptions of patients with malignant blood diseases. J Clin Nurs 22(23–24):3503–3512. doi:10.1111/jocn.12333
Andersen BL (2009) In sickness and in health: maintaining intimacy after breast cancer recurrence. Cancer J 15(1):70–73. doi:10.1097/PPO.0b013e318198c742
Schmidt CE, Bestmann B, Kuchler T, Longo WE, Kremer B (2005) Ten-year historic cohort of quality of life and sexuality in patients with rectal cancer. Dis Colon Rectum 48(3):483–492. doi:10.1007/s10350-004-0822-6
Herman JM, Narang AK, Griffith KA, Zalupski MM, Reese JB, Gearhart SL, Azad NS, Chan J, Olsen L, Efron JE, Lawrence TS, Ben-Josef E (2013) The quality-of-life effects of neoadjuvant chemoradiation in locally advanced rectal cancer. Int J Radiat Oncol Biol Phys 85(1):e15–e19. doi:10.1016/j.ijrobp.2012.09.006
Reese JB, Keefe FJ, Somers TJ, Abernethy AP (2010) Coping with sexual concerns after cancer: the use of flexible coping. Support Care Cancer 18(7):785–800. doi:10.1007/s00520-010-0819-8
Reese JB, Porter LS, Somers TJ, Keefe FJ (2012) Pilot feasibility study of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer. J Sex Marital Ther 38(5):402–417. doi:10.1080/0092623x.2011.606886
Epstein NB, Baucom DH (eds) (2002) Enhanced cognitive behavioral therapy for couples: a contextual approach. American Psychological Association (APA), Washington D.C.
Masters WH, Johnson VE (1970) Human sexual inadequacy. Little Brown & Company, Boston
Barsky Reese J, Porter LS, Regan KR, Keefe FJ, Azad NS, Diaz LA Jr, Herman JM, Haythornthwaite JA (2014) A randomized pilot trial of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer. Psychooncology 23(9):1005–1013. doi:10.1002/pon.3508
Bandura A (2006) Guide for constructing self-efficacy scales. In: Pajares F, Urdan T (eds) Self-efficacy beliefs of adolescents. IAP-Information Age Publishing Inc., Greenwich, CT, pp. 307–338
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’Agostino R Jr (2000) The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26(2):191–208. doi:10.1080/009262300278597
Alder J, Zanetti R, Wight E, Urech C, Fink N, Bitzer J (2008) Sexual dysfunction after premenopausal stage I and II breast cancer: do androgens play a role? J Sex Med 5(8):1898–1906. doi:10.1111/j.1743-6109.2008.00893.x
Speer JJ, Hillenberg B, Sugrue DP, Blacker C, Kresge CL, Decker VB, Zakalik D, Decker DA (2005) Study of sexual functioning determinants in breast cancer survivors. Breast J 11(6):440–447. doi:10.1111/j.1075-122X.2005.00131.x
Wiegel M, Meston C, Rosen R (2005) The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther 31(1):1–20
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49(6):822–830
Canada AL, Neese LE, Sui D, Schover LR (2005) Pilot intervention to enhance sexual rehabilitation for couples after treatment for localized prostate carcinoma. Cancer 104(12):2689–2700. doi:10.1002/cncr.21537
Rosen RC, Cappelleri JC, Gendrano N III (2002) The international index of erectile function (IIEF): a state-of-the-science review. Int J Impot Res 14(4):226–244. doi:10.1038/sj.ijir.3900857
Andresen EM, Malmgren JA, Carter WB, Patrick DL (1994) Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prev Med 10(2):77–84
Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH (1999) Diagnostic evaluation of the erectile function domain of the international index of erectile function. Urology 54(2):346–351. doi:10.1016/S0090-4295(99)00099-0
Baser RE, Li Y, Carter J (2012) Psychometric validation of the female sexual function index (FSFI) in cancer survivors. Cancer 118(18):4606–4618. doi:10.1002/cncr.26739
Baucom D, Porter L, Kirby J, Gremore T, Wiesenthal N, Aldridge W (2009) A couple-based intervention for female breast cancer. Psychooncology 18(3):276–283. doi:10.1002/pon.1395
Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, United States
Milbury K, Cohen L, Jenkins R, Skibber J, Schover L (2013) The association between psychosocial and medical factors with long-term sexual dysfunction after treatment for colorectal cancer. Support Care Cancer 21(3):793–802. doi:10.1007/s00520-012-1582-9
Barsky JL, Friedman MA, Rosen RC (2006) Sexual dysfunction and chronic illness: the role of flexibility in coping. J Sex Marital Ther 32(3):235–253. doi:10.1080/00926230600575322
Flynn KE, Lindau ST, Lin L, Reese JB, Jeffery DD, Carter J, Baron SR, Abramsohn EM, Weinfurt KP (2015) Development and validation of a single-item screener for self-reporting sexual problems in U.S. Adults J Gen Intern Med 30(10):1468–1475. doi:10.1007/s11606-015-3333-3
Reese JB, Shelby RA, Abernethy AP (2011) Sexual concerns in lung cancer patients: an examination of predictors and moderating effects of age and gender. Support Care Cancer 19(1):161–165. doi:10.1007/s00520-010-1000-0
Reese JB, Shelby RA, Keefe FJ, Porter LS, Abernethy AP (2010) Sexual concerns in cancer patients: a comparison of GI and breast cancer patients. Support Care Cancer 18(9):1179–1189. doi:10.1007/s00520-009-0738-8
Hill G, Holborn C (2015) Sexual minority experiences of cancer care: a systematic review. J Cancer Policy 6:11–22. doi:10.1016/j.jcpo.2015.08.005
Ussher JM, Perz J, Kellett A, Chambers S, Latini D, Davis ID, Rose D, Dowsett GW, Williams S (2016) Health-related quality of life, psychological distress, and sexual changes following prostate cancer: a comparison of gay and bisexual men with heterosexual men. J Sex Med 13(3):425–434. doi:10.1016/j.jsxm.2015.12.026
Wassersug RJ, Lyons A, Duncan D, Dowsett GW, Pitts M (2013) Diagnostic and outcome differences between heterosexual and nonheterosexual men treated for prostate cancer. Urology 82(3):565–571. doi:10.1016/j.urology.2013.04.022
Boehmer U, Potter J, Bowen DJ (2009) Sexual functioning after cancer in sexual minority women. Cancer J 15(1):65–69
Gilbert E, Ussher JM, Hawkins Y (2009) Accounts of disruptions to sexuality following cancer: the perspective of informal carers who are partners of a person with cancer. Health (London) 13(5):523–541. doi:10.1177/1363459308336795
Kenny DA, Kashy DA, Cook WL (2006) Dyadic data analysis. The Guilford Press, New York
Acknowledgments
When conducting this study, Dr. Reese was supported by a Postdoctoral Fellowship Grant, PF-09-154-01-CPPB, from the American Cancer Society. Dr. Reese is currently supported by Mentored Research Scholar Grant, MRSG-14-031-01-CPPB, from the American Cancer Society.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional Review Board approval was obtained, and patients provided informed consent.
Conflict of interest
The authors do not have any conflicts of interest to report. The primary author controls all primary data and agrees to allow the journal to review the data if requested.
Additional information
This study was conducted when Dr. Reese was located within the Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, 5510 Nathan Shock Dr., Suite 100, Baltimore, MD, 21224.
Relevance to informing research policies and/or programs
The current study supports and extends models of coping with threats to sexual function and activity for individuals affected by cancer by suggesting that beliefs about one’s sexuality may change in response to both life-altering medical diagnoses and related interventions. These issues are of interest to the growing number of cancer survivors likely to face long-term sexual consequences of their cancer treatments.
Rights and permissions
About this article
Cite this article
Reese, J.B., Haythornthwaite, J.A. Importance of sexuality in colorectal cancer: predictors, changes, and response to an intimacy enhancement intervention. Support Care Cancer 24, 4309–4317 (2016). https://doi.org/10.1007/s00520-016-3265-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3265-4